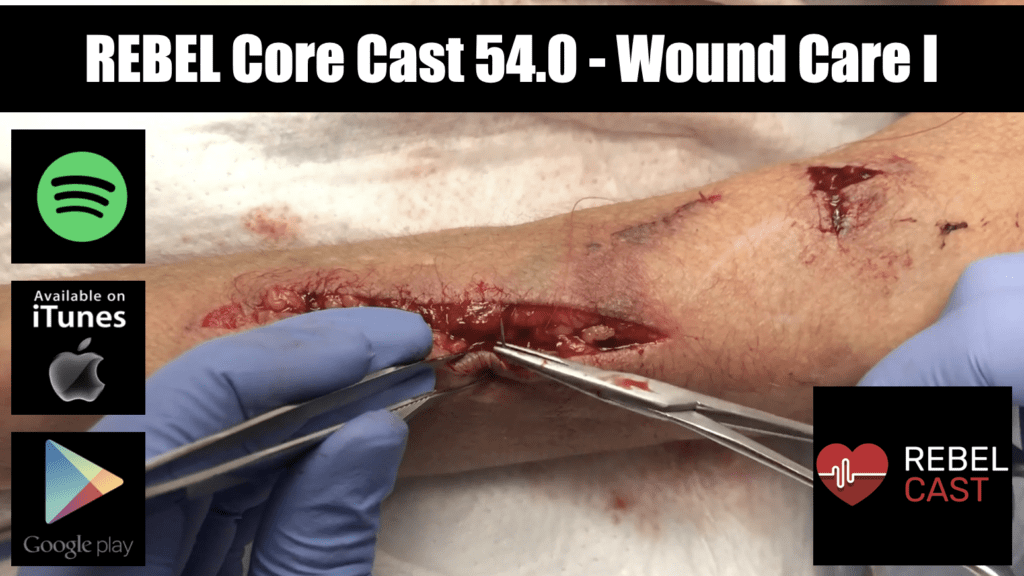
REBEL Core Cast 54.0 Wound Care I – Foreign Bodies
Take Home Points FBs are a very common complication of wounds. X-ray is poor at detecting foreign bodies US is a tremendous tool and be used dynamically at the bedside to assist w FB extraction Prophylactic antibiotics are not routinely …