Paper: U. Zeymer HT et al. Extracorporeal Life Support in Infarct-Related Cardiogenic Shock. NEJM 2023. PMID: 37634145
Clinical Question: Does early routine ECLS use (along with usual medical therapy) compared with usual medical therapy alone result in improved survival in patients with AMI complicated by cardiogenic shock for whom early revascularization is planned?
What They Did:
- Investigator-initiated, randomized, multicenter, open-label trial in two European countries (Germany and Slovenia)
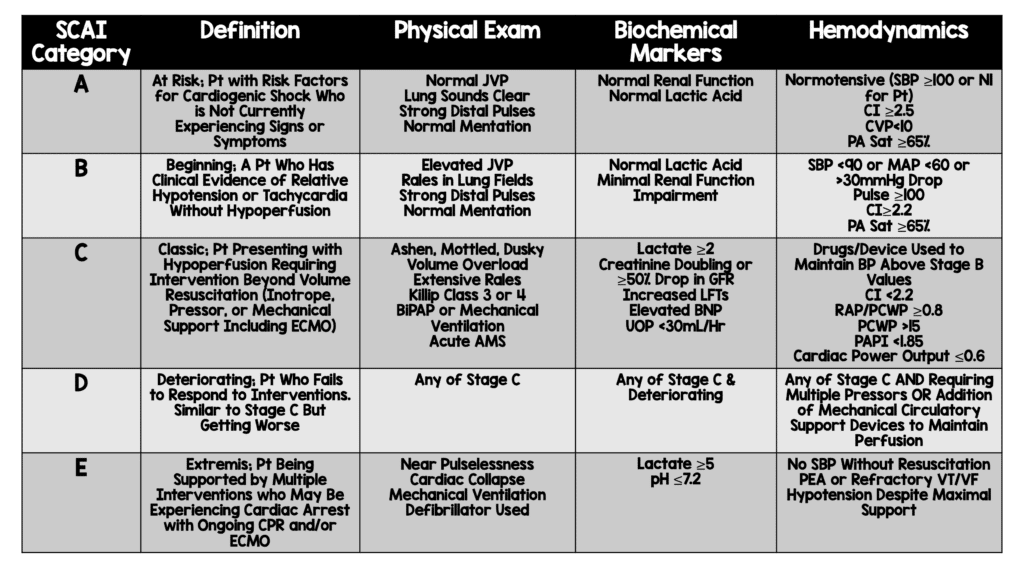
- Immediately after the performance of coronary angiography examining coronary anatomy, patients with AMI complicated by cardiogenic shock (SCAI stage C, D, or E) for whom early revascularization was planned were randomly assigned 1:1 to receive:
- ECLS: Early ECLS + Usual Medical Treatment
- Initiated during index catheterization, preferably before PCI
- Control: Usual Medical Treatment Alone
- Crossover to ECLS was to be avoided according to the trial protocol but could be performed under specific predefined criteria for HD deterioration under medical therapy, escalation therapy using other devices such as IABP or a microaxial transvalvular flow pump was allowed. Criteria included:
- Severe HD instability with impending HD collapse
- Increase in arterial lactate level >3mmol/L during a 6hr period
- Increase in vasopressor use by 50% from baseline to maintain a MAP >65mmHg
- Crossover to ECLS was to be avoided according to the trial protocol but could be performed under specific predefined criteria for HD deterioration under medical therapy, escalation therapy using other devices such as IABP or a microaxial transvalvular flow pump was allowed. Criteria included:
- ECLS: Early ECLS + Usual Medical Treatment
SCAI (Society for Cardiovascular Angiography and Interventions) Criteria
Outcomes:
- Primary: Death from any cause at 30d
- Secondary:
- Time until HD stabilization
- ICU LOS
- Acute renal failure warranting RRT
- Recurrent MI
- Rehospitalization for CHF
- Initiation and duration of catecholamine therapy
- Use and duration of mechanical ventilation
- Poor neurologic outcome (CPC 3 or 4) at 30d
- Safety:
- Moderate or severe bleeding (Type 3 to 5 according to Bleeding Academic Research Consortium [BARC] Criteria)
- Stroke or systemic embolization
- Peripheral vascular complications warranting interventional or surgical therapy
Inclusion:
- Adult patients (18 to 80 years of age)
- AMI complicated by cardiogenic shock
- Cardiogenic shock defined as:
- SBP <90mmHg for >30min OR the initiation of catecholamines to maintain a SBP >90mmHg
- Arterial lactate >3mmol/L
- Signs of impaired organ perfusion with at least one of the following criteria
- AMS
- Cold or clammy skin and limbs
- UOP <30mL/hr
- Planned early revascularization by either percutaneous coronary intervention (PCI) or coronary-artery bypass grafting (CABG)
- Cardiogenic shock defined as:
Exclusion:
- Patients who had undergone cardiopulmonary resuscitation for more than 45 minutes before randomization
- Mechanical cause of cardiogenic shock
- Severe peripheral-artery disease precluding insertion of ECLS cannulas
Results:
- 420 patients underwent randomization:
- 417 patients were included in final analyses
- Median Age ≈63yrs
- Median SBP ≈96mmHg
- Oliguria ≈72%
- AMS ≈95%
- Cold, Clammy Skin/Limbs ≈97%
- STEMI ≈67%
- Most Common Coronary Culprit = LAD (47.6%)
- Multivessel Disease ≈67%
- Cardiac Arrest Prior to Randomization ≈77%
- Median Time Until ROSC = 20min
- Median LVEF = 30%
- Median Lactate 6.9mmol/L
- SCAI Shock Stage:
- C
- ECLS: 49.8%
- Control: 53.4%
- D
- ECLS: 18.2%
- Control 8.7%
- E
- ECLS 32.1%
- Control 38.0%
- Majority of patients had PCI performed (96.6%)
- Impella CP was most common mechanical circulatory support in patients without ECLS (85.7%)
- C
- Death From Any Cause at 30d
- ECLS: 47.8%
- Control: 49.0%
- RR 0.98; 95% CI 0.80 to 1.19; p = 0.81
- Results of the sensitivity analyses in the per-protocol and as-treated populations were similar to the findings of the primary analysis
- Pre-specified and post hoc analyses showed results across all subgroups that were consistent with those of the primary analysis
- Median Duration of Mechanical Ventilation
- ECLS: 7d (Range 4 to 12d)
- Control: 5d (Range 3 to 9d)
- Median Difference: 1d; 95% CI 0 to 2
- No difference between treatment groups regarding
- Duration of catecholamine therapy
- Time until HD stabilization
- Other Secondary Outcomes of Note (ECLS vs Control)
- Renal-Replacement Therapy: 8.1% vs 13.9% (RR 0.58; 95% CI 0.33 to 1.03)
- Poor Neurologic Outcome (CPC 3 or 4): 24.8% vs 22.6% (RR 1.03; 95% CI 0.88 to 1.19)
- Moderate or Severe Bleeding:
- ECLS: 23.4%
- Control: 9.6%
- RR 2.44; 95% CI 1.50 to 3.95
- Peripheral Vascular complications Warranting Intervention
- ECLS: 11.0%
- Control 3.8%
- RR 2.86; 95% CI 1.31 to 6.25
Strengths:
- Asks a clinically important question with sparse evidence
- Multicenter randomized controlled trial
- Groups were well balanced at baseline
- Included only patients with more advanced cardiogenic shock (Required a lactate level >3mmol/L)
- Randomization appropriately performed
- Primary outcome was objective reducing chance for bias
Limitations:
- Open-label trial and therefore blinding of the ECLS intervention not possible. This can have impacts on therapeutic decisions of the treating physicians
- 39 patients crossed over from the control group to ECLS which could dilute any effect that would have been seen between groups
- Convenience sample of patients (non-consecutive enrollment) which causes selection bias
- Groups had some baseline differences
- Prior PCI (ECLS 13% vs Control 20.9%)
- Triple vessel disease (ECLS 30% vs Control 42.0%)
- Unclear time to ECLS (i.e. Door to randomization). Was ECLS instituted to late in this cohort?
Discussion:
- Possible Reasons for absence of benefit of ECLS in cardiogenic shock?
- Device-related complications counterbalance any potential benefit (More bleeding and peripheral ischemic complications warranting intervention occurred more frequently in ECLS group)
- Duration of mechanical ventilation (Longer in the ECLS group which could alter outcomes)
- VA ECMO is associated with increased LV afterload (More dobutamine used in ECLS group suggests increased LV afterload which can be associated with increased oxygen consumption)
- Cause of poor outcomes (Poor outcomes not primarily related to circulatory failure (77% of patients had cardiac arrest prior to randomization and this resulted in 25% of patients having neurologic causes of death)
- It is unclear what the timing of ECLS was. It could be that ECLS was initiated too late in the patient’s clinical course and therefore would not show any benefit.
- Interestingly a subgroup analysis according to shock-severity stage was not included in this trial
- There will most likely be some patients where ECLS is necessary and lifesaving
- The results of the ECLS-SHOCK trial do not tell us which ones
- Patient selection and timing are everything when it comes to ECLS
- How long were the patients down for? What was their initial rhythm? Did they get bystander CPR? We don’t know any of this information unfortunately and all are key in patient selection
- The median lactate level before revascularization was 6.9mmol/L (Range 4.6 to 9.9). This makes me think these patients were down for some time.
- At our institution patients do not go for diagnostic heart catheterization and then get put on ECMO, they are initiated on ECMO during the time of their initial resuscitation and then go for heart catheterization once they are stabilized.
- I have a feeling that the lack of benefit in this trial is due to poor patient selection and the delayed timing of ECMO.
Author Conclusion: “In patients with acute myocardial infarction complicated by cardiogenic shock with planned early revascularization, the risk of death from any cause at the 30-day follow-up was not lower among the patients who received ECLS therapy than among those who received medical therapy alone.”
Clinical Take Home Point: In patients with acute myocardial infarction complicated by cardiogenic shock and needing revascularization, the incidence of death from any cause at 30 days was not decreased among patients receiving ECLS compared to those receiving medical therapy alone. However I have a feeling that the lack of benefit in this trial is due to poor patient selection (We don’t have details of the arrest) and the initiation of ECLS may have simply been too late in the patient’s clinical course (after diagnostic cath instead of during the resuscitation).
References:
- Zeymer HT et al. Extracorporeal Life Support in Infarct-Related Cardiogenic Shock. NEJM 2023. PMID: 37634145
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter/X: @EMSwami)



