- Airway management is paramount; expect a challenging intubation and consider controlling the airway early if there is apparent airway compromise.
- Understanding the cause of angioedema (mast cell vs. bradykinin mediated) helps dictate directed management.
- Urticaria and pruritus = MAST CELL mediated, which is treated like a standard allergic reaction.
REBEL Core Cast 108.0 – Angioedema
Angioedema:
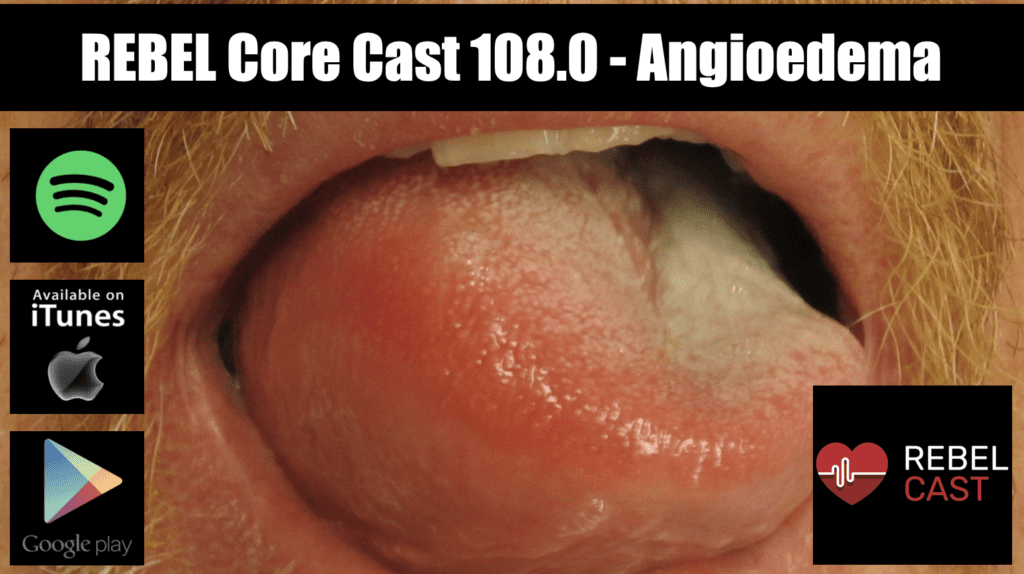
- A transient, localized, non-pitting distention of the skin (subcutaneous layer) or the respiratory and gastrointestinal tracts (submucosal layer)
- Inflammatory mediators cause vascular permeability, allowing fluid to diffuse into the interstitium
- Effects areas with loose connective tissue, like the oropharynx, extremities, and genitalia
Epidemiology:
- 0.1 to 0.3% of people who take NSAIDs (Nzeako 2010).
- 0.1 to 0.7% patients that take ACE inhibitors (but 20-30% of all angioedema presentations to the Emergency Department)
- 3 times more common in Black Americans (Kostis 2005)
- 0.01 to 0.002% of general population exhibit some form of hereditary angioedema (Zuraw 2008)
Mechanism and Pathophysiology:
|
Mast Cell Mediated |
Bradykinin Mediated |
Other |
|
IgE Dependent |
ACE-Inhibitor |
Infectious |
|
IgE Independent |
Hereditary Angioedema |
Iatrogenic |
|
NSAIDs |
Acquired C1 Inhibitor Deficiency |
Idiopathic |
- Mast Cell (granulocyte) Mediated
- Mast cell activation (by IgE crosslinking or directly) leads to the generation of mediators (histamine, heparin, leukotriene and prostaglandin D2), which increases vascular permeability.
- Features
- Urticaria and pruritis
- Rapid onset (1-2 hours)
- IgE Dependent (Type I Hypersensitivity) Reactions
- An allergen cross-links two or more IgE molecules on mast cells or basophils and initiates a signal cascade leading to degranulation.
- Pro-inflammatory mediators then act on the mucosa and cause angioedema. These chemicals can recruit other cells, like eosinophils, and may lead to anaphylaxis.
- IgE Independent Reactions
- Mast cells are activated directly by certain medications (i.e. meperedine, radiocontrast agents)
- Release inflammatory mediators and lead to angioedema.
- NSAIDs hinder the formation of prostaglandins within mast cells and other leukocytes. This can cause an abundance of leukotrienes and other pro-inflammatory mediators and precipitate angioedema (Nzeako 2010).
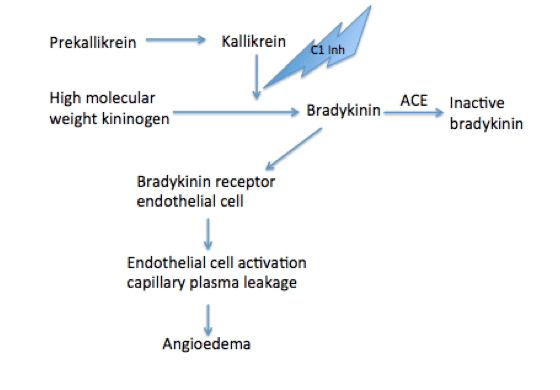
- Plasma globulins called kininogens release bradykinin and cause vascular permeability.
-
- Features
- Absence of urticaria and pruritus
- Insidious onset (24-36 hours)
- ACE Inhibitors
- Inhibition of ACE hinders the degradation of bradykinin and can lead to idiosyncratic angioedema.
- Typically involves the mouth, larynx, pharynx, and subglottic tissue (Kostis 2005).
- Hereditary Angioedema (presents in childhood) and Acquired C1 Inhibitor Deficiency (adulthood)
- Both involve abnormalities in the level or function of the C1 inhibitor.
- Without the C1 inhibitor, the plasma-kallikrein-kinin system produces more bradykinin.
- Both conditions can range in severity from benign to life threatening (Wilkerson 2012).
- Features
- Other Etiologies
- In pediatrics, illnesses like the common cold, Streptococcus pyogenes (GAS) pharyngitis, and urinary tract infections can cause isolated angioedema (without urticaria).
- Iatrogenic agents like calcium channel blockers, fibrinolytic agents, estrogens, and herbal supplements
- Idiopathic
Differential:
- Anaphylaxis
- Erysipelas or cellulitis
- Contact dermatitis
- Superior vena cava syndrome
- Hypothyroidism
- Peritonsillar abscess
- Autoimmune disease
- Parasitic Infection
Presentation:
- Asymmetrical
- Does not regularly involve gravitationally dependent areas
- Frequently painless
- Non blistering, non desquamating
- Hives, pruritus, bronchospasm or flushing = mast cell release (histaminergic)
- Abdominal pain, nausea, vomiting
- Hoarse voice
- Stridor
- Drooling, difficulty swallowing
- Throat tightness
- Inability to phonate high pitched “E” sound
Management:
- Basics- ABCs, IV, O2, Cardiac Monitor
- Anatomically challenging airway
- Edema of the anterior tongue, base of the tongue, or larynx significantly increases the likelihood of intubation or tracheostomy. Stable patients with isolated anterior tongue edema should undergo fiberoptic laryngoscopy in the ED (McCormick 2011)
- Avoid unnecessary airway manipulation (can exacerbate edema)
- Edema may obscure the neck anatomy
- Anatomically challenging airway
- Airway Management
- Early intubation often indicated as swelling may progress and supraglottic rescue devices may be ineffective
- Consider awake intubation
- Double setup with standard intubation equipment and surgical airway tools for possible failed orotracheal airway
- Can’t intubate, cant ventilate event necessitates surgical airway
- Do not rely on external anatomy for cricothyroidotomy as edema will obscure landmarks (Hessert 2013)
- Plan for a large vertical incision in the midline of the neck
- Directed Treatment
- Mast cell mediated (histaminergic) angioedema
- Epinephrine 300 to 500 mcg IM
- H1 antihistamines
- Diphenhydramine 25-50 mg PO/IM/IV
- Cetirizine 5-10 mg PO
- H2 antihistamines
- Ranitidine 50 – 150 mg PO/IV
- Glucocorticoids: Methylprednisolone 1-2mg/kg per day x 2 days
- Bradykinin mediated angioedema
- Unlikely to respond to epinephrine, antihistamines, or glucocorticoids
- Mast cell mediated (histaminergic) angioedema
-
-
- Hereditary Angioedema and C1 esterase deficiencies (Wilkerson 2012)
- Replace C1 inhibitor with Berinert 20units/kg IV (harvested from pooled human plasma)
- Antagonize kallikrein with Ecallantide 30mg IM
- Antagonize bradykinin b2 receptor with Icatibant 30mg SQ
- Replace ACE with 2 units FFP (2nd line)
- ACE inhibitor related angioedema
- Discontinue ACE Inhibitor
- Secure airway, supportive care
- Icatibant
- A single randomized controlled trial comparing Icatibant with prednisone and antihistamines demonstrated more rapid improvement of symptoms with Icatibant (Bas 2015)
- CAMEO: phase III, double blind, placebo controlled trial showed no benefit.
- Fresh Frozen Plasma (FFP)
- Case reports and case series have shown a benefit from FFP (Wilkerson 2012, Hassen 2013)
- However, FFP also contains bradykinin and high molecular weight kininogen which may exacerbate angioedema
- Tranexamic Acid (TXA)
- TXA inhibits the conversion of plasminogen to plasmin which, in theory, could reduce bradykinin production.
- Low quality evidence (case reports and case series) have hinted at benefit but are mixed.
- There is no high-quality evidence to support its use and no safety data.
- Hereditary Angioedema and C1 esterase deficiencies (Wilkerson 2012)
-
Take Home Points:
- Airway management is paramount; expect a challenging intubation and consider controlling the airway early if there is apparent airway compromise.
- Understanding the cause of angioedema (mast cell vs. bradykinin mediated) helps dictate directed management.
- Urticaria and pruritus = MAST CELL mediated, which is treated like a standard allergic reaction.
Read More
- EMCrit: Podcast 145 – Awake Intubation Lecture from SMACC
- ERCast: Angioedema
References:
- Baş M et al. A randomized trial of icatibant in ACE-inhibitor-induced angioedema. N Engl J Med. 2015; 372(5):418-25. PMID 25629740
- Hassen GW et al. Fresh frozen plasma for progressive and refractory angiotensin-converting enzyme inhibitor-induced angioedema. J Emerg Med 2013; 44 (4): 764-772. PMID: 23114109
- Hessert MJ and Bennett BL. Optimizing Emergent Surgical Cricothyrotomy for Austere Environments. Wilderness and Environmental Medicine. 2013;24:53-66. PMID 23062323
- Kostis JB et al. Incidence and characteristics of angioedema associated with enalapril. Arch Intern Med. 2005;165(14):1637-1642. PMID 16043683
- McCormick M et al. Site involvement as a predictor of airway intervention in angioedema. Laryngoscope. 2011;121:262–266. PMID 21271571
- Morgan PB. Hereditary angioedema—therapies old and new. N Engl J Med. 2010;363(27):2673. PMID 20818894
- Nzeako UC. Diagnosis and management of angioedema with abdominal involvement: A gastroenterology perspective. World J Gastroenterol, 2010;16(39):4913-4921. PMID 20954277
- Sinnert R et al. Randomized Trial of Icatibant for Angiotensin- Converting Enzyme InhibitoreInduced Upper Airway Angioedema (CAMEO Study). J Allergy Clin Immune Tract 2017; 5(5): 1402-9. PMID: 28552382
- Wilkerson RG. Angioedema in the Emergency Department: An Evidence Based Review. Emergency Medicine Practice. EBMedicine.net. 2012; 14(11).
- Zuraw et al. An overview of angioedema: Clinical features, diagnosis, and management. In: UptoDate, Feldweg AM (ed.) UpToDate, Waltham, MA.
- Zuraw BL. Clinical practice. Hereditary angioedema. N Engl J Med. 2008;359(10):1027-1036.
PMID 18768946
Post Created By: Anand Swaminathan MD, MPH (Twitter @EMSwami)
Post Peer Reviewed By: Salim Rezaie MD (Twitter @SRRezaie)
Cite this article as: Anand Swaminathan, "REBEL Core Cast 108.0 – Angioedema", REBEL EM blog, September 13, 2023. Available at: https://rebelem.com/rebel-core-cast-108-0-angioedema/.