The standard weight based dosing of UFH is 80U/kg bolus followed by an infusion started at 18U/kg/hr, titrated to a target activated partial thromboplastin time (aPTT) of 1.5 to 2.5x the control range or an anti-Xa level of 0.3 to 0.7u/mL. The efficacy of UFH in reaching and maintaining appropriate anticoagulation is poorly understood.
REBEL Cast 125: 1st 48 Hours of PE Management – How Good is Unfractionated Heparin?
Paper: Prucnal CK et al. Analysis of Partial Thromboplastin Times in Patients With Pulmonary Embolism During the First 48 Hours of Anticoagulation With Unfractionated Heparin. Acad Emerg Med 2020. PMID: 31625654
Clinical Question: How effective is UFH in obtaining appropriate anticoagulation during the first 48 hours of administration to patients with acute PE?
What They Did:
- Retrospective analysis of a PE response team (PERT) data base
- Single, large, urban academic teaching hospital (Massachusetts General Hospital)
- October 2012 to April 2017
- 2 Standard Dosing Regimens Evaluated
- Bolus + Drip (Low Risk of Bleeding): 80U/kg + Continuous titrated infusion starting at 18U/kg/hr
- Drip Only (Higher Risk of Bleeding): Continuous titrated infusion starting at 18U/hr
- Subsequent aPTT (seconds) and Rate Changes
- <40: +3U/kg/hr
- 40 – 49.9: +2U/kg/hr
- 50 – 49.9 +1U/kg/hr
- 60 to 80: No change
- 1 to 100: -2U/kg/hr
- >100: Hold for 60minutes then -3U/kg/hr
Outcomes:
- Proportion of patients with a therapeutic aPTT value during each 6 hour time period
- A therapeutic aPTT was defined as a value of 60 to 80seconds
- A therapeutic Anti-Xa level was defined as a value of 0.3 to 0.7u/mL
Inclusion:
- Adult patients
- Acute PE
- PERT team consulted
- Received anticoagulation with UFH according to guideline standard dosing
Exclusion:
- Patients treated with nonstandard dosing regimens
Results:
- 505 patients met inclusion criteria
- PE Severity
- Saddle: 17.4%
- Rt Heart Strain on CT: 46.9%
- Hemodynamic Collapse: 7.9%
- Massive PE: 28.3%
- Right Heart Strain on Echo: 21.4%
- Elevated Troponin Level: 55.3%
- Interventions Received:
- Systemic thrombolysis: 4.0%
- Catheter-Based Intervention: 5.9%
- Surgical Thrombectomy: 2.0%
- ECMO: 1.4%
- IVC Filter: 5.0%
- 30d Outcome:
- Mortality: 5.7%
- Re-Thrombosis: 3.9%
- Bleeding: 3.0%
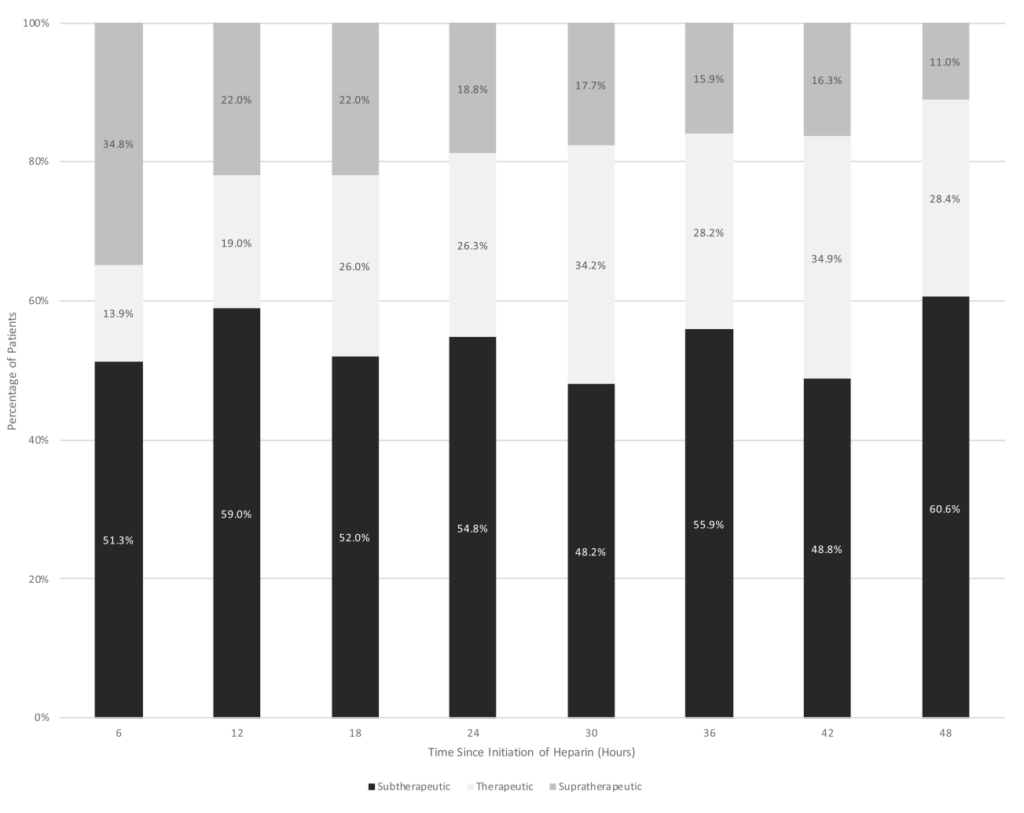
- Therapeutic aPTT in patients receiving bolus and infusion of UFH
- At 6hrs: 13.9% (10.2 to 18.5%)
- At 12hrs: 19% (14.2 to 25.0%)
- At 24hrs: 26.3% (25.3 to 33.1%)
- At 36hrs: 28.3% (22.0 to 35.4%)
- At 48hrs: 28.4% (20.8 to 37.5%)
- PE Severity
- Therapeutic aPTT in patients receiving infusion only of UFH
- At 6hrs: 14.5% (9.5 to 21.5%)
- At 12hrs: 23.3% (15.2 to 32.3%)
- At 24hrs: 41.4% (31.6 to 51.9%)
- At 36hrs: 37.0% (26.8 to 48.5%)
- At 48hrs: 42.1% (30.2 to 55.0%)
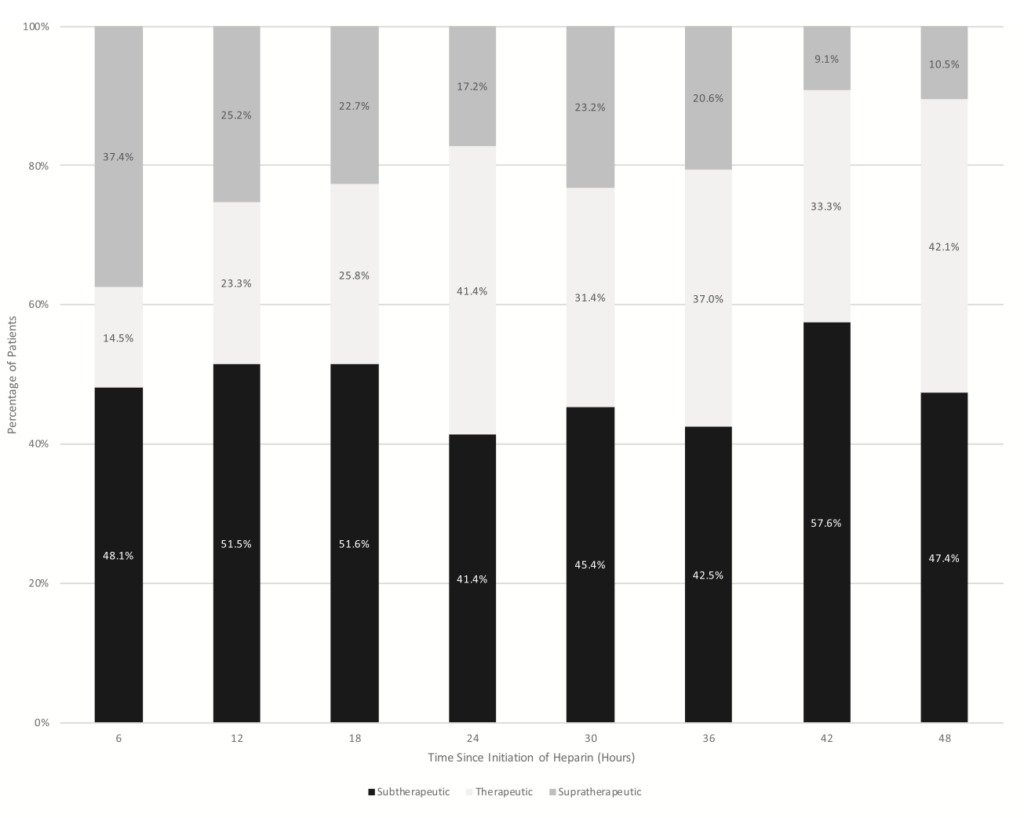
- No patients had all therapeutic aPTT values
Strengths:
- Asks a clinically important question
- Study was stratified for patients being treated with bolus plus titrated infusion or titrated infusion only
- Used UFH standard dosing strategies used by most physicians
- Performed a sensitivity analysis that excluded all patients treated with systemic or catheter-directed thrombolysis, surgical embolectomy, or ECMO
Limitations:
- Initiation of AC was defined as the order start time for UFH in the electronic medical record. There could have been delays in actually starting the UFH
- No real details on chart extraction methodology (i.e. how they handled incomplete or conflicting data)
- Only one abstractor where there is no assessment of the abstractors performance or comparison to another abstractor
- Unclear why one strategy was chosen over another
- Selection bias: Only patients consulted by PERT
- For patients with more than one aPTT value in a given 6 hour time period, the first therapeutic value was selected for analysis. If there was no therapeutic value, the first aPTT value reported was used
- Single center study meaning local factors may limit generalizability to other institutions
- Time outside therapeutic aPTT is not all equal. An aPTT that is slightly above or below the reference range would be considered outside the range (i.e. values close to the therapeutic cutoff were considered equivalent to those far from the cut-off range)
- This study does not determine whether time spent in the therapeutic range affects morbidity and mortality (Very low mortality rate = 6%)
Discussion:
- Only a minority of patients in whom the PERT team was consulted treated with UFH using standard dosing had a therapeutic aPTT during the first 48 hours of anticoagulation with the majority of patients being subtherapeutic
- The proportion of patients in therapeutic range was lowest at 6 hours (14%) and highest at 42 hours (35%)
- Approximately 40% of patients failed to reach the therapeutic range in the first 48 hours of AC
- It wasn’t until 36 hours after the initiation of UFH that >50% of patients had at least one therapeutic aPTT
- There were no patients who had all aPTT values within the therapeutic range during the first 48hours of UFH therapy
- Something to Think About: Thrombus burden can be substantial and heparin resistance may be present, so standard dosing may be inadequate in these patients
- My Opinion: LMWHs offer several advantages over unfractionated heparin including a longer half-life, increased bioavailability, and a more predictable dose response. In addition, LMWHs are dosed by weight, administered subcutaneously, and usually do not require dose adjustments or laboratory monitoring. Whereas unfractionated heparin is largely hepatically cleared, LMWHs are renally cleared
- In 2017 [2], there was a Cochrane review that compared LMWH to UFH for the initial treatment of VTE. This included 29 RCTs with over 10,000 patients. The authors concluded that with moderate quality of evidence fixed dose LMWH reduced the incidence of recurrent thrombotic complications and occurrence of major hemorrhage during initial treatment with no difference in overall mortality compared to UFH
- The 2019 European Society of Cardiology [3] also states: “LMWH and fondaparinux are preferred over UFH for initial anticoagulation in PE, as they carry a lower risk of inducing major bleeding and heparin-induced thrombocytopenia. Neither LMWH nor fondaparinux need routine monitoring of anti-Xa levels. Use of UFH is nowadays largely restricted to patients with overt hemodynamic instability or imminent hemodynamic decompensation in whom primary reperfusion treatment will be necessary. UFH is also recommended for patients with serious renal impairment [creatinine clearance ≤30mL/min] or severe obesity. If LMWH is prescribed in patients with CrCl 15 – 30mL/min, an adapted dosing scheme should be used.”
Author Conclusion: “The majority of patients with acute PE spend most of their first 48 hours outside of the therapeutic range of AC when treated with guideline standard dosing of UFH. Over half of the patients fail to achieve any therapeutic PTT level within 24 hours of UFH initiation, and no patient had all therapeutic aPTTs. Future research should focus on identifying factors associated with achieving therapeutic AC with UFH.”
Clinical Take Home Point: In this single center study of PERT team consulted PE patients standard dosing of UFH left most patients with a subtherapeutic aPTT level in the first 48 hours of treatment. Either we need to question the dosing regimen we use for UFH or we should consider switching to LMWH in the initial treatment of PE patients.
References:
- Prucnal CK et al. Analysis of Partial Thromboplastin Times in Patients With Pulmonary Embolism During the First 48 Hours of Anticoagulation With Unfractionated Heparin. Acad Emerg Med 2020. PMID: 31625654
- Robertson L et al. Fixed Dose Subcutaneous Low Molecular Weight Heparins Versus Adjusted Dose Unfractionated Heparin for the Initial Treatment of Venous Thromboembolism. Cochrane Database Syst Rev 2017. PMID: 28182249
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter/X: @EMSwami)



