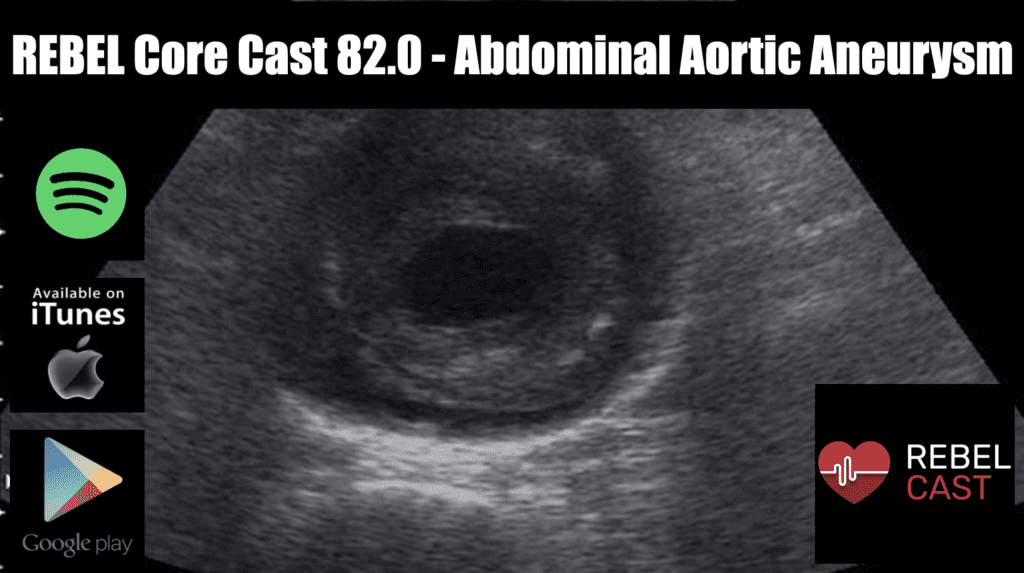
REBEL Core Cast 82.0 – Abdominal Aortic Aneurysm
Take Home Points Consider AAA in patients with acute onset of back or abdominal pain particularly in patients > 50 and in those with a history of hypertension Consider ruptured AAA in patients (especially those > 50 years of age) …