REBEL Cast Ep91: Static Ultrasound vs Landmark Placement of Subclavian Central Lines
Paper: Wang Q, et al. Static Ultrasound Guidance VS. Anatomical Landmarks for Subclavian Vein Puncture in the Intensive Care Unit: A Pilot Randomized Controlled Study. J Emerg Med. Sep 22 2020; PMID: 32978029
Clinical Question:
- Does ultrasound or landmark guided placement of subclavian central lines result in improved success rates and lower rates of complications?
What They Did:
- Single center blinded randomized controlled pilot trial in China
- Patients were randomized to:
-
- Ultrasound Group
- Anatomic Landmark Group
- Subclavian access was at physician discretion
- All physicians placing lines had at least one-year experience in the ICU. After 3 unsuccessful attempts, the operating physician was replaced with another physician after 3 unsuccessful attempts
- Defined puncture failure as: unsuccessful cannulation after 5 attempts OR a puncture time > than 5 minutes
- In the Ultrasound Group, doppler was used to confirm the vein and a marker pen on the skin in front of the clavicle was made to indicate the direction of the subclavian vein puncture. (See IMAGE BELOW). The rest of the procedure, including needle stick and catheter insertion was then performed similar to the Landmark Group.
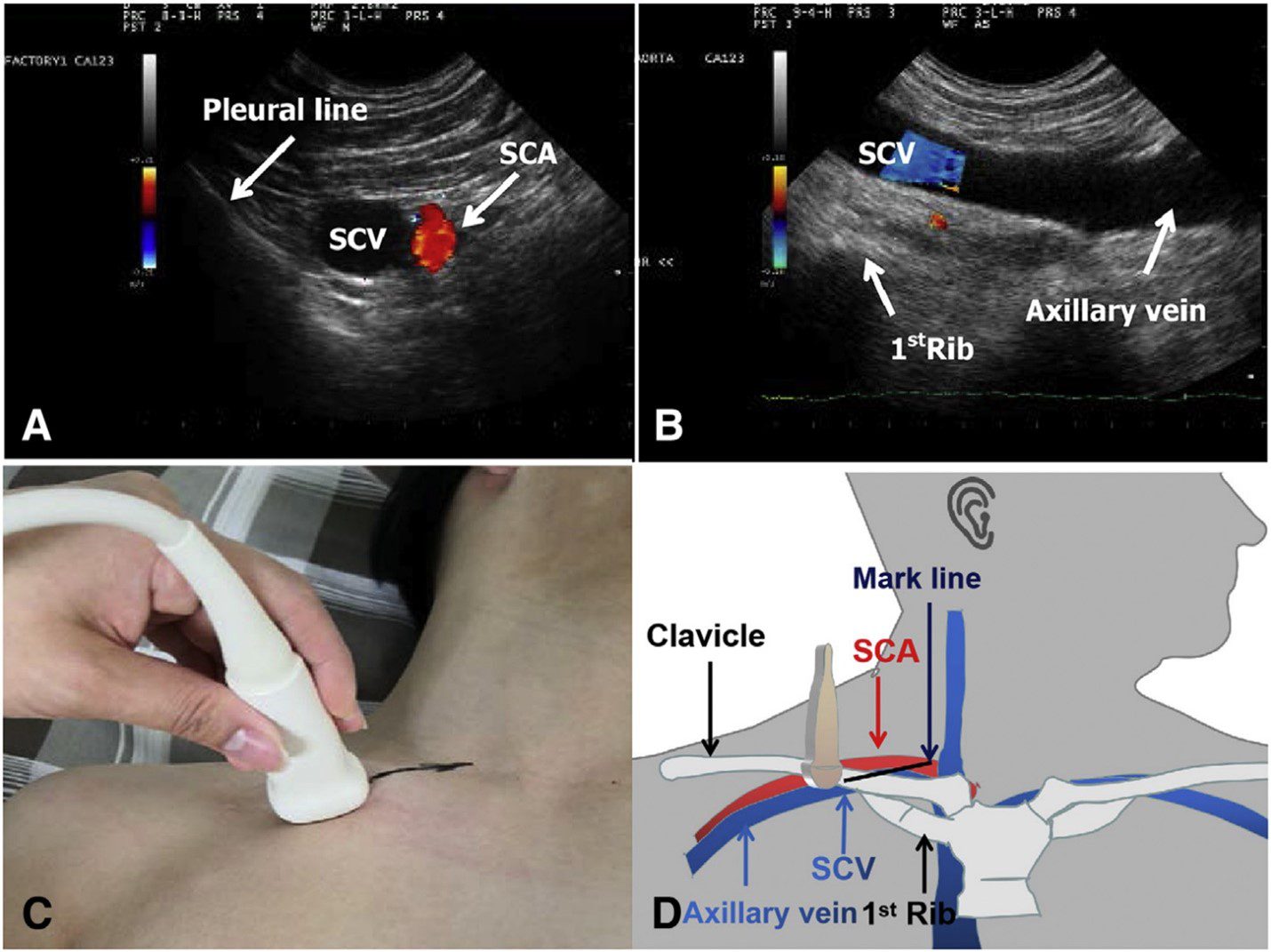
Figure 1. Ultrasound-guided puncture of the subclavian vein (SCV). (A) Short-axis image of the subclavian artery (SCA) and SCV. (B) Long-axis image of the SCV. (C) CA123 probe used for long axis exploration of the SCV and marking of the puncture direction. (D) Anatomic diagram of ultrasound-guided puncture. Image from original paper (PMID: 32978029)
Inclusion Criteria:
- ICU patients
- Age ≥ 18 years old
- Required subclavian central access
Exclusion Criteria:
- Severe coagulation disorder
- INR ≥ 3.5
- Disseminated intravascular coagulation with active bleeding
- Platelet count < 20,000
- Bilateral pneumothorax
- Requiring CPR or emergent central venous access
- Patients who had a puncture time of > 5 minutes
Outcomes:
Primary
- Puncture success rate
Secondary
- Number of puncture attempts
-
- Defined as number of individual needle insertions including needle retraction and reinsertion
- Success rate of first attempt
- Puncture time
- Defined as time from skin puncture to placement of guidewire
- Rates of complications
- Such as pneumothorax, puncture of an artery, hematoma formation, ectopic catheterization, thoracic duct injury, hemothorax and pericardial tamponade
Results:
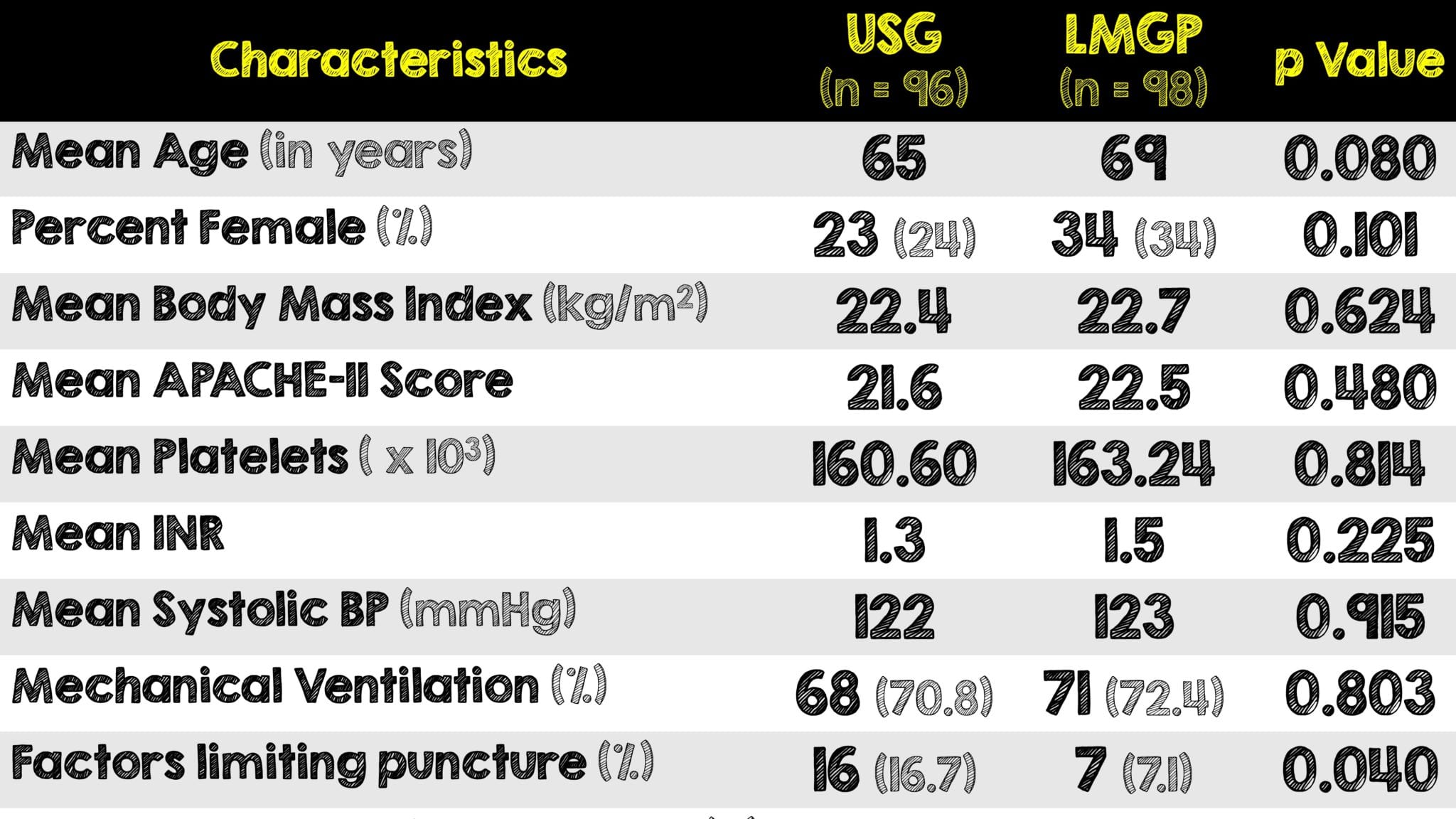
- Of the 207 total patients approached, 200 met inclusion criteria, and 194 were included in the final analysis
- Presence of factors limiting puncture was the only parameter that differed between the two groups and was more common in the ultrasound group
- This included presence of a pacemaker or local anatomical changes due to surgery/trauma
Critical Results:

- The ultrasound group had a higher rate of puncture success, a lower incidence of complications and a lower rate of artery puncture than the landmark group
- Secondary outcomes of number of attempts, first-try success rate and puncture time were all comparable between the two groups
Strengths:
- Addresses a clinically relevant question related to ultrasound use during a common procedure of obtaining central venous access
- Clear definitions of puncture attempt, puncture time and anticipated complications
- Had an organized system when several unsuccessful punctures were made in succession
- Both ultrasound and landmark group were fairly well balanced
- There were no significant differences in age, sex, BMI, APACHE II score, INR, platelets, blood pressure, use of vasoactive medications, use of mechanical ventilation, puncture site or diagnosis upon ICU admission
- There was no difference between in operator experience between groups
- Limited confounding variables by using the same procedure for central line insertion across both groups
Limitations:
- Small sample size
- Unknown ultrasound experience of physicians
- Unclear if there was central line procedure skills training given beforehand
- There are several factors that could affect the results of ultrasound-guided puncture including physician experience, inter-physician variability, ultrasound exploration, patient positioning and the population studied
- Performed in a single center at a single institution which could limit external validity to other institutions
- All patients were placed in a supine position, however a Trendelenburg position could have helped to obtain the largest vein size
Discussion:
- The ICU physicians involved in this study had at least one year of ICU experience, although most had >3 years. All had ultrasound-guided puncture training; however, the article did not explicitly state how much training these physicians, especially given how operator dependent ultrasonography is
- Complications were greater in the landmark group and more specifically, mis-puncture of the artery was statistically significant. It is not reported whether there were any arterial cannulations.
- A possible future study should evaluate the success rate of real-time vs static ultrasound guidance in the placement of subclavian central lines.
- Although not statistically significant, the use of ultrasound resulted in higher success on the first attempt, less puncture time and less complications than the landmark guided group.
- Ultrasound is becoming more common in clinical settings and newer generations of physicians are using it more and more. Studies like this one helps raise awareness for their need especially when performing bedside procedures.
- One thing to consider is that Chinese people may be thinner than westerners and hence easier to image. The average BMI in this study was 22.
- The debate between using ultrasound and “doing it blind” is clouded behind a potential clinical bias of “wasting time” with ultrasound. While retrieving, setting up and actually performing the procedure with ultrasound does take substantially more time, the results of this study, specifically the rate of mis-puncture complications, show that it’s better for patient care and overall procedural success when ultrasound is used.
Author’s Conclusions:
- Static ultrasound-guided subclavian vein puncture is superior to the traditional landmark-guided approach for critically ill patients in the ICU. It is suggested that static ultrasound-guided puncture techniques should be considered for subclavian vein puncture.
Our Conclusion:
- Although a single center study with some potential limitations, this pilot study showed static ultrasound guided subclavian vein catheterization resulted in a higher overall success of venous catheterization when compared to the landmark group. Furthermore, the higher first pass successes, faster procedure time and less complications strongly support the notion that ultrasound should be used for all central line procedures. The idea of “wasting time” with the ultrasound is a moot point when doing it “blind” takes longer and has a higher likelihood of resulting in an artery mis-puncture as observed in this study.
Clinical Bottom Line:
- Ultrasound should be utilized for venous identification of the subclavian vein prior to central catheterization as it can overcome challenges associated with variation in local vascular anatomy and resulted in more successful punctures when compared to landmark guided palpation.
REFERENCES:
- Wang Q, et al. Static Ultrasound Guidance VS. Anatomical Landmarks for Subclavian Vein Puncture in the Intensive Care Unit: A Pilot Randomized Controlled Study. J Emerg Med. Sep 22 2020; PMID: 32978029
- Brass P, et al. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015 Jan 9; PMID: 25575245
- Kornbau C, et al. Central line complications. Int J Crit Illn Inj Sci. 2015 Jul-Sep; PMID: 26557487
- Lalu MM, et al; Canadian Perioperative Anesthesia Clinical Trials Group. Ultrasound-Guided Subclavian Vein Catheterization: A Systematic Review and Meta-Analysis. Crit Care Med. 2015 Jul; PMID: 25803646
- Rezayat T, et al. Ultrasound-Guided Cannulation: Time to Bring Subclavian Central Lines Back. West J Emerg Med. 2016 Mar;17. PMID: 26973755
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srreziae)