 If you mainly treat adults or both adults and children like me, then you have probably heard the (very annoying) quote, “kids are not just small adults”, and so I won’t say it again. Well, I guess I just did, but at least I wont stop at this quote, but attempt to explain how kids are not small adults, and how this may impact their care in the emergency department and the intensive care unit.
If you mainly treat adults or both adults and children like me, then you have probably heard the (very annoying) quote, “kids are not just small adults”, and so I won’t say it again. Well, I guess I just did, but at least I wont stop at this quote, but attempt to explain how kids are not small adults, and how this may impact their care in the emergency department and the intensive care unit.
Nearly all organ systems of young children are immature and developing throughout childhood and on into adulthood, including the cardiovascular system. Without a basic understanding of the key physiologic differences, the emergency and intensive care physicians will be ill equipped to care for the critical ill child.
To understand how kids with shock present differently than adults, it’s important to discuss a few basic differences regarding intravascular volume and cardiovascular system in children especially neonates and infants (1-24 months of age). Also remember shock is defined the exact same way as it would be in adults even though the presentation and underlying physiology may differ. Shock is simply a state where tissue/organ blood flow is inadequate to meet tissue/organ metabolic demands.
Intravascular Volume
Newborns have a larger proportion of total body water compared to adults (75% vs. 60%) with the majority of it being in the extracellular fluid (ECF) (~40% vs. 25%) (1). Interestingly, the percentage of ECF decreases throughout childhood while the percentage of intracellular fluid (ICF) remains relatively stable throughout life. So logically one may think that given the higher percentage of fluid in the ECF, and therefore a larger portion of fluid contained in the intravascular space, that newborns and infants might be protected against volume depletion. However, given their large surface area to weight ratio compared to adolescents or adults, younger children may have a greater proportion of fluid losses from their ECF and intravascular space, which can lead to, decreased preload (2). Therefore, children may present more profoundly volume depleted, despite shorter duration of illness and relatively shorter exposures to environmental stress. As we will see later, children present with later stages of shock and volume depletion and may require more early aggressive volume resuscitation compared to adults.
Cardiovascular Differences
There are also major cardiovascular differences between children and adults, which makes them more susceptible to cardiovascular collapse in the setting of shock.
Newborns and infants have an immature myocardial calcium regulation system (t-tubes and sarcoplasmic reticulum) and have difficulty storing and releasing calcium for myocyte contraction (3). Because of this, they can become highly dependent on extracellular calcium for adequate myocardial contractility. This is the reason why the uses of Calcium Channel Blockers (ie Diltiazem, Verapamil) are contraindicated in pediatric tachydysrhythmia’s (3). Their use in the young child with a tachydysrhythmia can precipitate severe myocardial depression and even cardiac arrest. It is also a reason that the pediatric sepsis guidelines (as we will review in a later article) recommend checking ionized calcium levels and repleting calcium early. Intravenous calcium can have significant inotropic effects and may restore myocardial function and hemodynamic stability especially when ionized calcium levels are low.
Newborns and infants also have limited ability to increase inotropic function and stroke volume and operate at a higher baseline contractile state (4). Their myocardium contains more Type I collagen, which is more fibrous and less elastic, making it stiffer and less compliant (5). Throughout childhood the amount of elastic Type III collagen increases, making the myocardium more compliant and able to increase it’s contractile ability, and improve stroke volume in the face of hemodynamic compromise.
Due to their stiffer, less compliant myocardium the main way newborns and infants can increase their cardiac output is by increasing their heart rate. Unfortunately because of their baseline higher resting heart rates, their ability to further increase their heart rate and cardiac output is limited (6). This will make more sense by comparing heart rate responses between healthy 16-year (resting HR~60-80 bpm), and 4-month olds (resting HR ~120-140 bpm). If the 16-year old developed a hypovolemic shock, it would be easy to imagine their HR could at least double (140-150 bpm) to maintain an adequate CO and increase their BP. Now image our 4-month old developed hypovolemic shock, it would be impossible to double their HR 240- 260 bpm. Recall maximal heart rate 220- age, so this is usually the upper limit that a healthy infant can increase their heart rate. Also, to sustain an elevated heart rate response even close to that, would severely limit diastolic filling time leading to decreased stroke volume as well as decreased coronary perfusion and myocardial ischemia.
Figure 1
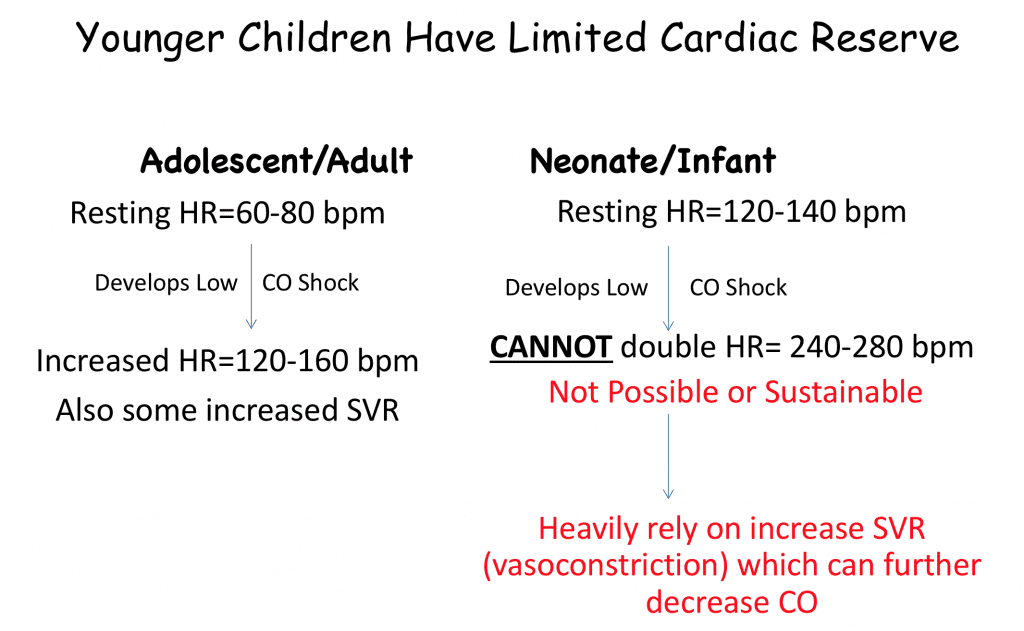
Newborns and infants also have less β-adrenergic receptors and sympathetic innervations, and a more dominant parasympathetic nervous system leading to more exaggerated vagal responses.
So young children have limited cardiac reserve with limited ability to increase contractility (inotropic), and heart rate (chronotropic) response to improve cardiac output. Because of these factors, children heavily rely on increases in systemic vascular resistance (SVR) to maintain blood pressure in the setting of shock.
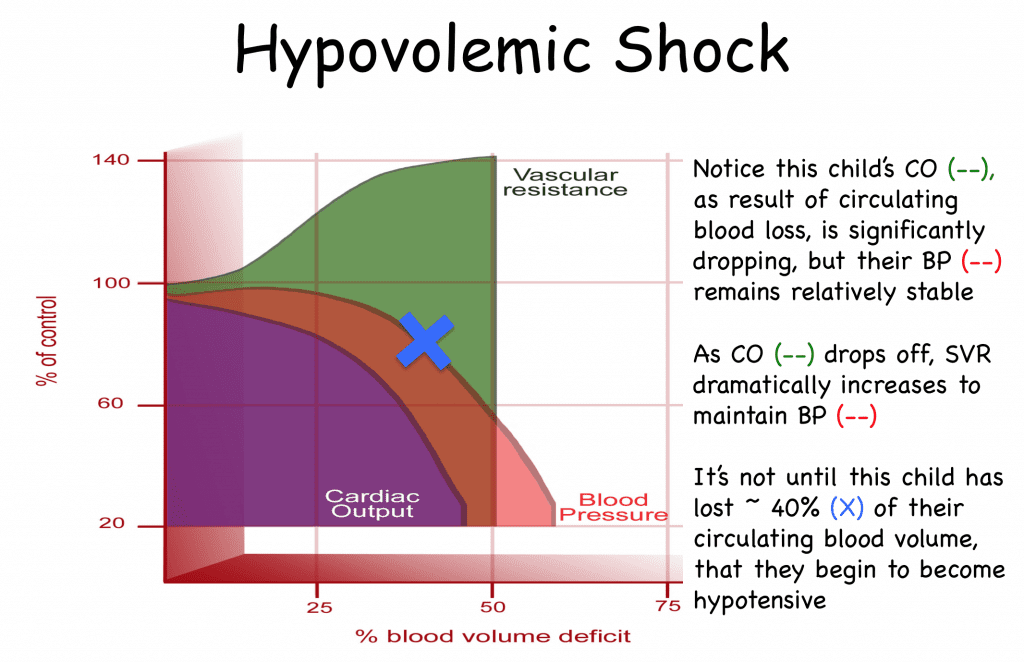
Figure 2 below demonstrates just how effective children are at increasing their systemic vascular resistance to maintain their blood pressure in the setting of shock. In fact, a healthy child can lose up to 30-40% of their circulating blood volume before they even develop hypotension. This is due in large part to increased systemic vascular resistance. The neuro-hormonal responses to the early phases of shock, results in sympathetic activation and systemic vasoconstriction. The coronary and cerebral circulations are not directly affected by these sympathetic responses. So the rise in SVR allows the child to redistribute and preserve blood flow to these vulnerable circulations. Blood pressure (diastolic more so than systolic) can be maintained because of this compensation. Unfortunately, as shock progresses, compensatory mechanisms become less effective at preserving cardiac output. The elevated SVR presents an additional stress on the LV in the form of increased afterload. Sustained tachycardia prevents diastolic filling and further reduces preload. When these compensatory mechanisms are exhausted, children develop hypotension. Therefore, hypotension, is always a late finding in pediatric shock. .
Figure 2
“Cold” Vs. “Warm” Shock:
So if hypotension is a late finding, we want to start treatment for these children as early as possible. They key is early identification of these hemodynamically compromised children, and then further differentiating the cause of their shock state.
In children, we tend to use many physical exam findings to help us differentiate whether a child is in shock and also the type of shock. We categorize shock into 2 major categories, “Cold” or low cardiac output shock and “warm”, vasodilatory shock from decreased systemic vascular resistance.
Figure 3:
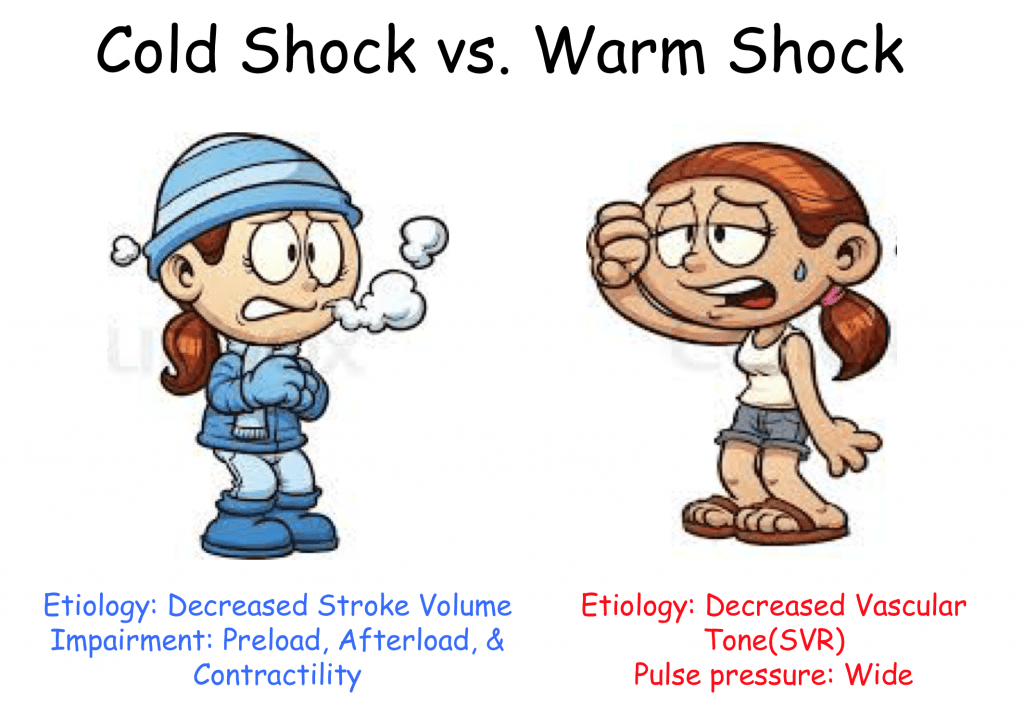
Cold Shock:
The term cold shock describes a child with poor cardiac output, mainly due to a decreased stroke volume, which results in poor perfusion. As stroke volume decreases, heart rate increases making our patient tachycardic with poor peripheral perfusion. Because of poor peripheral perfusion, children will actually feel cold to the touch, have decreased strength of their pulses, mottled skin, and develop capillary refill >2 seconds.
As shock progresses, children will increase SVR and vasoconstrict to compensate for their shock, in turn further worsening their perfusion. Eventually both peripheral pulse as well as central pulses (femoral, carotid) will be diminished in late stages of shock. Their blood pressure may be normal as children further increase SVR. A narrowing of their pulse pressure (difference between SBP – DBP) may be seen, which is another sign of a low stroke volume state. Other signs and symptoms of shock would be similar to adults, as they would develop end organ dysfunction as the body attempts to shunt blood from non-vital organs to vital organs such as the heart, lungs and brain. Children may have altered mental status, tachypnea, nausea, vomiting, acute kidney injury (oliguric), acidemia, and lactic acidosis.
Figure 4:
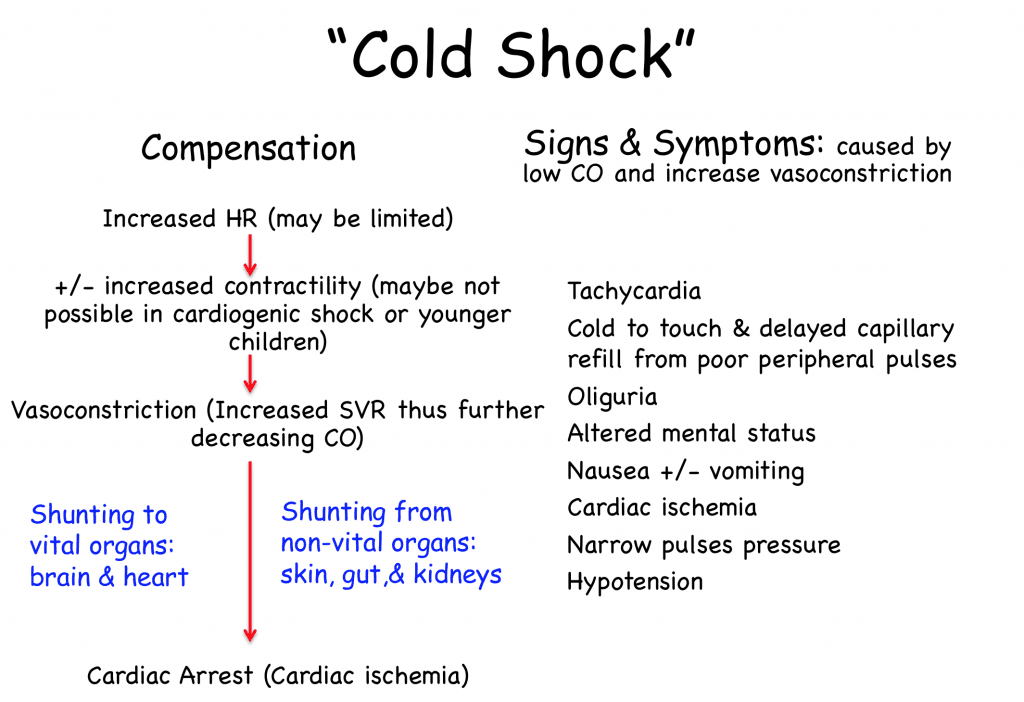
A simplistic view is to think of systolic blood pressure correlating with a patient’s stroke volume. Systolic blood pressure may be high, normal or low as children may be exhausting all compensatory mechanisms to maintain stroke volume. However, as they compensate they will increase their diastolic blood pressure, which reflects a patient’s systemic vascular resistance (vascular tone). As systolic blood pressure or stroke volume is compromised, patient will increase their diastolic blood pressure as systemic vascular resistance increases. As their stroke volume drops and systolic blood pressure decreases, diastolic blood pressure rises as SVR increases. The net result is a narrowing of the patient’s pulse pressure. You may actually see a child with other evidence of poor perfusion (delayed capillary refill, weak pulse strength, cold to touch), narrowed pulse pressure with a normal overall normal blood pressure, but they are in compensated shock. So pulse pressure represents stroke volume, and a narrow pulse pressure should indicate to the clinician that your patients stroke volume is compromised. It doesn’t tell you why it’s compromised, just that the determinants of stroke volume are impaired (low preload, low contractility or increased afterload). When a patient develops hypotension, or uncompensated shock, then cardiac arrest can soon follow.
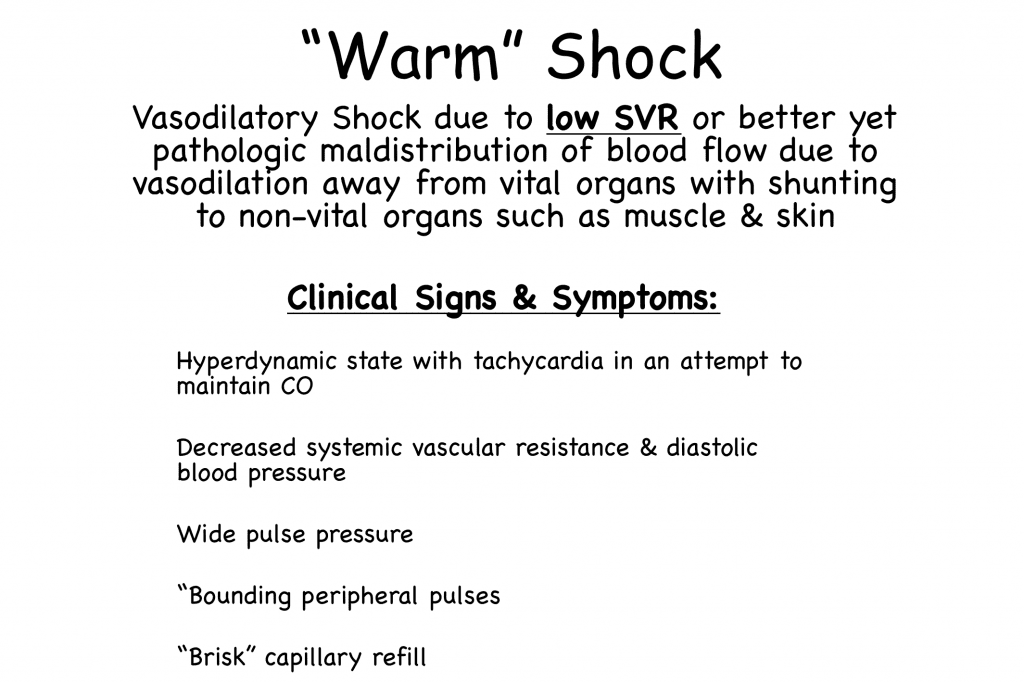
Warm Shock:
In “warm” or distributive shock the main pathophysiologic issue is profound vasodilation with low systemic vascular resistance. Interestingly, these children have a pathologic maldistribution of blood flow away from vital organs to non-vital organs like skin and muscle explaining some of their findings on presentation. These children present warm to the touch, bounding peripheral pulses and capillary refill that is almost instantaneous or “brisk”. There pulse pressure is usually wide owing to the low diastolic blood pressure from decreased systemic vascular resistance. They also will have evidence of decreased organ perfusion and may present with altered mental status, tachypnea, acidemia, and lactic acidosis.
Figure 5:
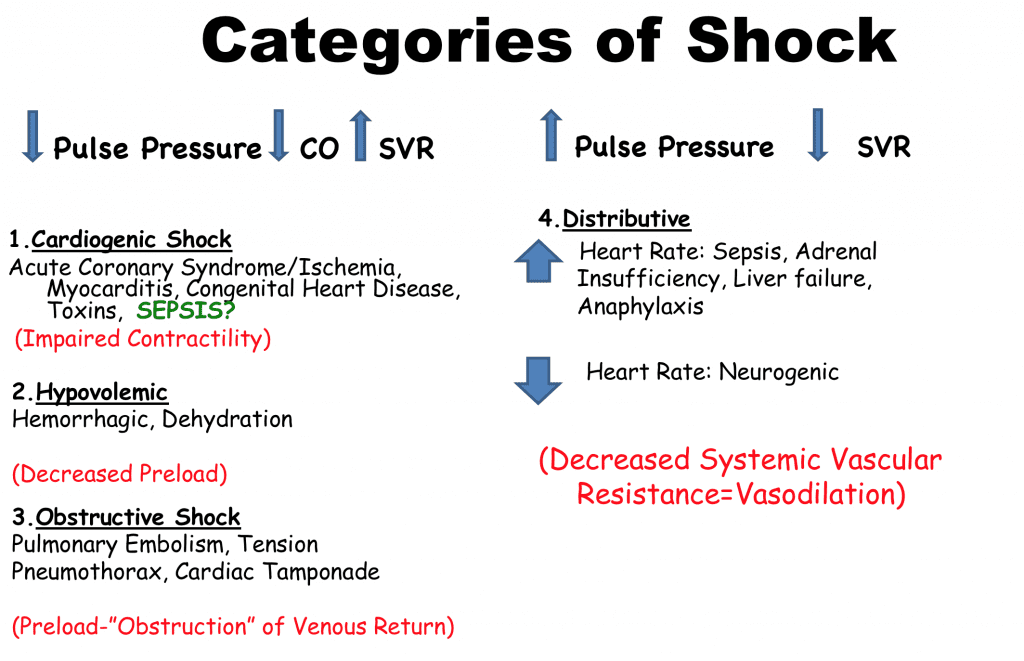
Categories of Shock:
The below figure separates the 4 major categories of shock into how they normally would present in either “cold” or “warm” shock. The confusion often lies in how to categorize septic shock. Classic teaching has placed septic shock into “warm” or vasodilatory shock, but as we will see in the next part, septic shock, especially in young children, can present as either “warm” or “ cold” shock but more commonly as “cold” shock (7). Many of the above cardiovascular differences contribute to this presentation as well as additional factors that we will discuss in our next part.
Figure 6:
Post Written by Frank Lodeserto, MD
and
Expert Peer Reviewed By:

Frank A. Maffei, MD
Chairman, Pediatrics
Director, Pediatric Critical Care Medicine
Janet Weis Children’s Hospital at Geisinger
Associate Professor of Pediatrics
Temple University School of Medicine
References:
- Friis-Hansen BJ, et al. Total body water in children. Pediatrics.1951. PMID: 148276342.
- Thomas NJ, et al. Hypovolemic shock in the pediatric patient. New Horizons. 1998. PMID: 9654319
- Brillantes AM, et al. Developmental and tissue-specific regulation of rabbit skeletal and cardiac muscle calcium channels involved in excitation-contraction coupling. Circ Res.1994. PMID: 8062423
- Luce WA, et al. Bench-to-bedside review: Developmental influences on the mechanisms, treatment and outcomes of cardiovascular dysfunction in neonatal versus adult sepsis. Critical Care. 2007. PMID: 17903309
- Marijianowski MM, et al. The neonatal heart has a relatively high content of total collage and type I collagen, a condition that may explain the less compliant state. Journal American College Cardiology.1994. PMID: 7722119
- Aneja RJ, et al. Difference between adult and pediatric septic shock. Minerva Anesthesiology. 2011. PMID: 21952599
- Ceneviva G, et al. Hemodynamic Support in Fluid-refractory Pediatric Septic Shock. Pediatrics. 1998. PMID: 9685464
Additional Reading:
- Maffei, FA, et al. The Approach to the Critically Ill Infant. Pediatric Critical Care Study Guide. 2012. Link HERE
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)



