- Clinical presentation is very nonspecific; evaluate all patients presenting with back pain for infectious risk factors.
- Baseline labs should not guide diagnosis, but may assist in later management.
- MRI is key to diagnosis, obtain this imaging in all patients who raise clinical suspicion
- Patients with hemodynamic instability and neurologic compromise warrant empiric antibiotics. The initiation of empiric antibiotics in hemodynamically stable, neurologically intact patients should be done on a case-by-case basis.
REBEL Core Cast 107.0 – Vertebral Osteomyelitis
Definition
- Inflammation of the vertebrae due to a pyogenic, fungal or mycobacterial organism.
- Classified as either acute (days), subacute (weeks) or chronic (months)
- Spondylodiscitis: a term encompassing osteomyelitis, spondylitis and discitis. Often used interchangeably with osteomyelitis.
Epidemiology
- 1 to 2.4 cases per 100,000 people (Zimmerli 2010)
- More common in males with M:F of 3:1
- Rate is also increasing due to increased number of spinal procedures
- Typically affects adults, with most cases occurring in patients over 50 years old.
Pathogenesis
- Infection occurs by three routes:
- Hematogenous spread – secondary to infections of the GU, skin, soft tissue and respiratory system, indwelling catheters or endocarditis
- Due to the bifurcated structure of the arterial supply, generally presents as infection of 2 contiguous vertebrae and the intervertebral disc
- Direct inoculation during trauma or spinal surgery
- Spread from adjacent soft tissue infection
- Hematogenous spread – secondary to infections of the GU, skin, soft tissue and respiratory system, indwelling catheters or endocarditis
- Organism
- Most cases in the United States are pyogenic.
- Most common organism is Staph Aureus (36-67% of cases) (Boody 2015).
- Other pathogens include: E. Coli, Pseudomonas Aeruginosa and Group B and G hemolytic Strep
- Other pathogens to consider:
- Fungal – blastomycosis, coccidiomycosis, histoplasmosis, aspergillosis
- Brucellosis
- Mycobacterial
- Most cases in the United States are pyogenic.
- Location: lumbar (48%) most common, followed by thoracic (35%) and cervical (6.5%)
History and Physical
- Symptoms
- Back pain – often described as dull, may be present for weeks to months
- Neurologic symptoms (paresthesias, weakness or radiculopathy) present in approximately one-third of patients
- Most patients lack systemic symptoms
- Exam
- Tenderness over affected vertebrae
- Paraspinal tenderness or spams may be present which may mislead the clinician towards a musculoskeletal diagnoses
- Risk Factors:
- Diabetes Mellitus (most common)
- Immunosuppression: HIV, Malignancy, chronic steroids or immunosuppressant medication use
- Spinal fracture, trauma or recent procedure
- Substance Abuse: Alcoholism and IVDU
- Presence of an indwelling vascular device
- Elderly
Diagnosis
- Labs
- Leukocytosis and Neutrophilia are poorly sensitive and highly non-specific (Gouliouris 2010). The degree of elevation does not predict disease severity.
- ESR and CRP are sensitive, yet not specific.
- CRP concentration rise and fall quicker than ESR, often used to guide treatment
- Blood Cultures – an important element in management and treatment
- Blood culture positivity often decides whether a patient will require a bone biopsy.
- Cultured specimen narrows antibiotic coverage
- Urinalysis/Urine Culture –UTI is a frequent missed source of bacteremia (especially in diabetic patients).
- Imaging
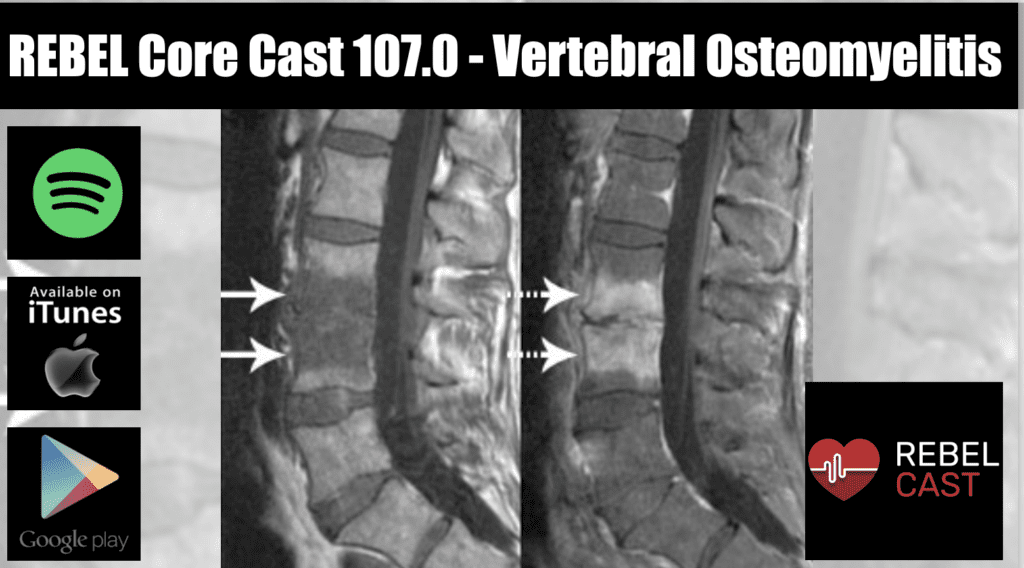
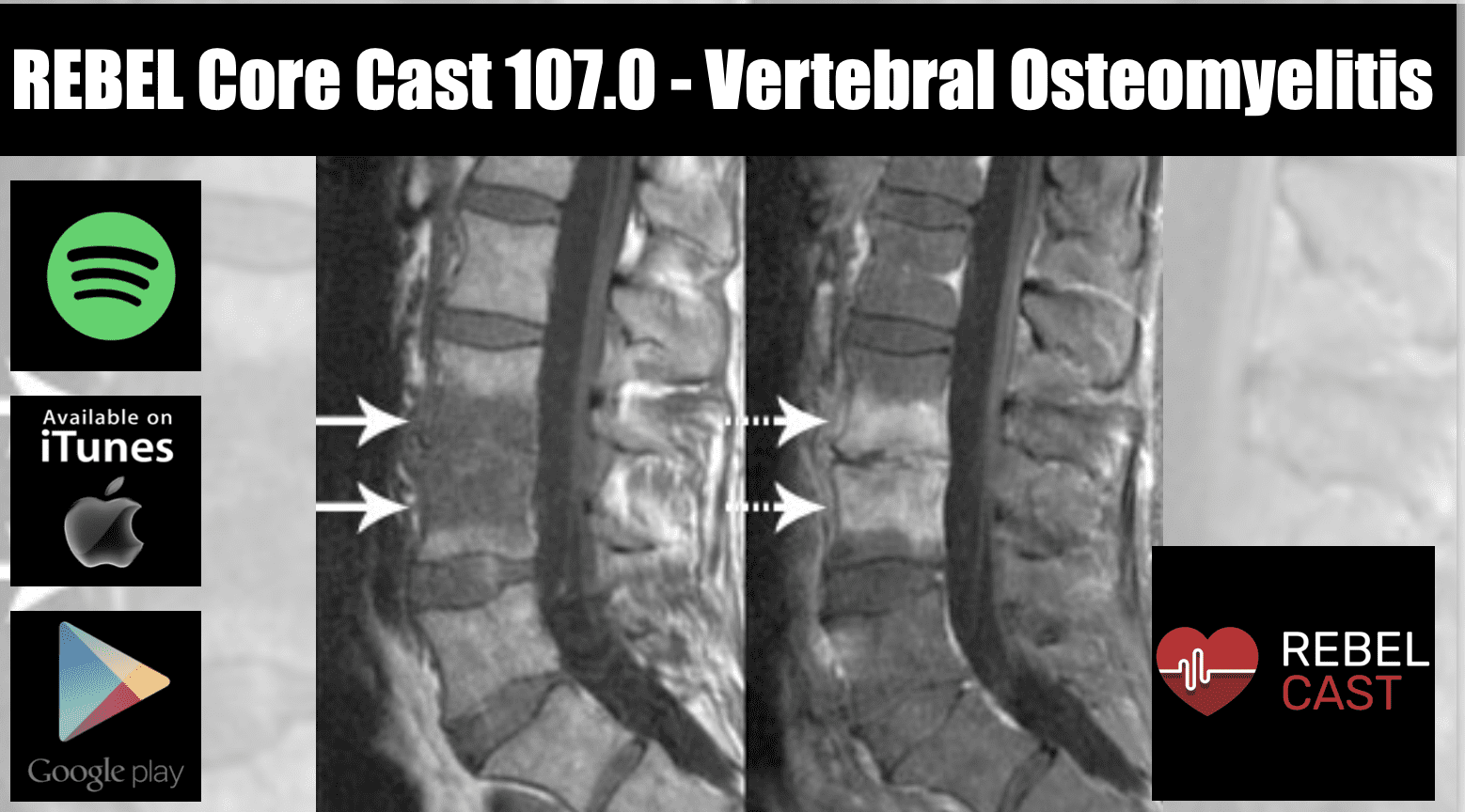
- Gadolinium enhanced MRI – modality of choice, highly sensitive and specific (Mylona 2009).
- Although MRI with and without contrast is preferred, a non-contrast MRI can evaluate for inflammatory processes.
- If a patient requires premedication or has renal failure, obtain the non-contrast MRI first. A contrast MRI can be done later to delineate subtle findings.
- Findings include: enhancement (hypointense on T1 and hyperintense on T2) of vertebral endplates and adjacent disc space (Image 1)
- CT Scan with IV contrast – use only of MRI contraindicated
- Inferior in evaluation of disc spaces and neural tissues
- Less sensitive than MRI and may be falsely negative in early disease
- Used primarily by surgeons for biopsy of spine
- Findings include loss of end plate definition and narrowing of disc space (Image 2)
- Previously used CT Myelogram now out of favor due to potential for intradural spread of infection.
- Inferior in evaluation of disc spaces and neural tissues
- Plain Radiographs – often done to evaluate other causes (masses, fracture) however not recommended for diagnosis
- Poorly sensitive and findings typically present in advanced disease (10-14 days after onset), once significant bone demineralization has already occurred
- Radionuclide studies – (including: Tech 99m Bone scan, Gallium -67)
- Sensitive but not specific, long acquisition time and difficult to obtain in the emergent setting
- Gadolinium enhanced MRI – modality of choice, highly sensitive and specific (Mylona 2009).
Management
- Pathogen directed therapy – Antibiotics tailored towards cultured organism
- Given the dependence on blood culture results to guide therapy, current recommendations (IDSA 2015 Guidelines) suggest holding empiric antibiotics in medically stable patients (non-septic, hemodynamically stable, neurologically intact) until cultures grow out.
- Note: this is a weak recommendation based on low quality evidence and patients should be managed on a case by case basis in conjunction with the inpatient treatment team
- Empiric coverage:
- Vancomycin 15-20 mg/kg/dose every 8-12 hrs
- Given the dependence on blood culture results to guide therapy, current recommendations (IDSA 2015 Guidelines) suggest holding empiric antibiotics in medically stable patients (non-septic, hemodynamically stable, neurologically intact) until cultures grow out.
PLUS
-
-
- 3rd Generation Cephalosporin: Cefotaxime (2 g IV every 6 hrs), Ceftriaxone (1 to 2 g IV daily) or Ceftazidime (1 to 2 g IV every 8 -12 hrs)
-
OR
-
-
- Cefepime 2 g IV every 12 hours
- Duration: 6 weeks (occasionally 12 weeks if advanced disease) of IV antibiotics followed by 1-2 months of oral antibiotics
-
- Surgical Consult – although most patients are successfully treated with antibiotics alone, some may require surgical intervention if there is concern for vertebral instability or spinal cord compromise.
- Indications for surgical intervention include: associated abscess formation, spinal cord compression, progression of disease despite antimicrobial treatment
- Obtain consult (Neurosurgery or Orthopedics) early, since patients may require bone biopsy for detection of organism
Take Home Points
- Clinical presentation is very nonspecific; evaluate all patients presenting with back pain for infectious risk factors.
- Baseline labs should not guide diagnosis, but may assist in later management.
- MRI is key to diagnosis, obtain this imaging in all patients who raise clinical suspicion
- Patients with hemodynamic instability and neurologic compromise warrant empiric antibiotics. The initiation of empiric antibiotics in hemodynamically stable, neurologically intact patients should be done on a case-by-case basis.
Graphics
Image 1: http://www.mghradrounds.org/clientuploads/nov_dec_2006/figure2.jpg
Image 2: http://www.thelancet.com/cms/attachment/2000991969/2003662063/gr3.jpg
References
Berbari EF, Kanj SS, et al. Executive Summary: 2015 Infectious Disease Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin Infect Dis 2015 Sept 15;61(6):859-63. PMID: 26316526
Boody B, et al. Vertebral Osteomyelitis and Spinal Epidural Abscess: An Evidence-based Review. J Spinal Disord Tech. 2015 Jul;28(6):E316-27 PMID: 26079841
Chowdhury V, Gupta A, Khandelwal N. Diagnostic Radiology: Musculoskeletal and Breast Imaging. 3rd ed. New Delhi: JP Brothers Medical Ltd; 2012
Della-Guistina, D. Evaluation and Treatment of Acute Back Pain in the Emergency Department. Orthopedic Emergencies 2015 May; 33(2) 311-26. PMID: 25892724
Gouliouris T, et al. Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother. 2010 Nov;65 Suppl 3:iii 11-24 PMID: 20876624
Mylona E, et al. Pyogenic Vertebral Osteomyelitis: A Systematic Review of Clinical Characteristics. Semin Arthritis Rheum. 2009 Aug; 39(1):10-7. PMID: 18550153
Pruitt CR, Perron AD. Specific Disorders of the Spine. In: Sherman SC eds. Simon’s Emergency Orthopedics. 7th ed. New York, NY: McGraw-Hill; 2014
Winters ME, Kluetz P et al. Back Pain Emergencies. Med Clin North Am, 2006 May;90(3):505-23. PMID: 16473102
Zimmerli W. Vertebral Osteomyelitis. N Engl J Med 2010 Mar; 362(11)1022-9. PMID: 20237348
Post Created By: Anand Swaminathan MD, MPH (Twitter @EMSwami)
Post Peer Reviewed By: Salim Rezaie MD (Twitter @SRRezaie)