The BOX Trial: BP & O2 Targets in Comatose Survivors of Cardiac Arrest
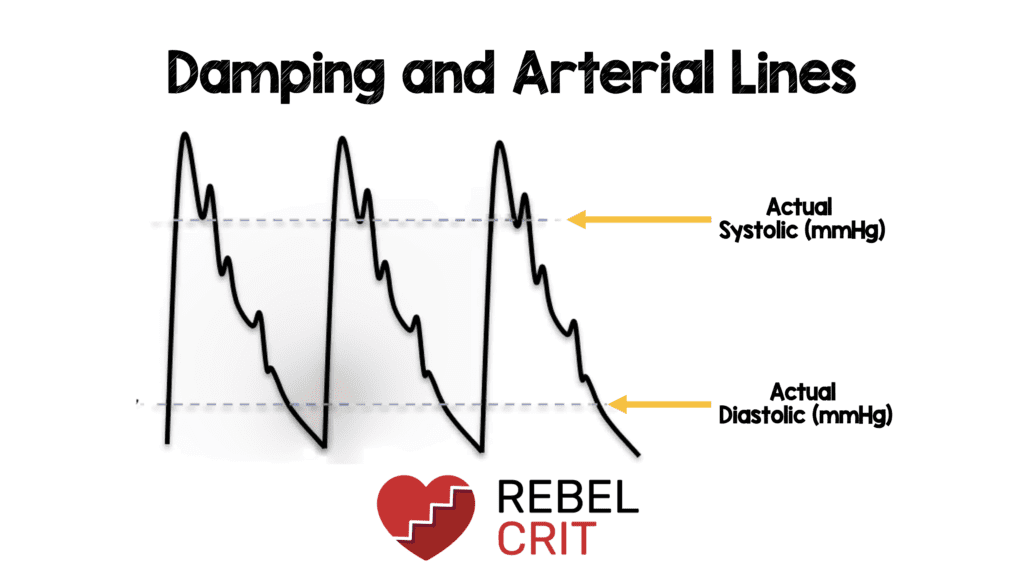
Background: Hypoxemia and hypoperfusion are important factors in outcomes after ROSC. While hypoxemia (SpO2 <90%) is clearly deleterious, it is unclear if hyperoxia is beneficial. Recent studies on patients requiring critical care have demonstrated that hyperoxia is harmful and instead …