 The use of heated and humidified high flow nasal cannula has become increasing popular in the treatment of patients with acute respiratory failure through all age groups. In part 1 we summarized how High Flow Nasal Cannula (HFNC) works. In part 2, we will discuss the main indications for its use in adult and pediatric patients.
The use of heated and humidified high flow nasal cannula has become increasing popular in the treatment of patients with acute respiratory failure through all age groups. In part 1 we summarized how High Flow Nasal Cannula (HFNC) works. In part 2, we will discuss the main indications for its use in adult and pediatric patients.
Adult Indications:
Acute Hypoxemic Respiratory Failure (Mainly from Pneumonia)
- HFNC may allow patients to cough, mobilize secretions and suction if necessary, which is difficult with NIPPV mask
- The only exception may be in my patients with acute COPD exacerbations from pneumonia, as there is evidence demonstrating a decreased mortality and need for intubation using NIPPV
- Frat, JP et al (1) conducted a a multi-centered, open-label RCT with 300 patients, mainly with community acquired pneumonia (CAP), randomized to either oxygen (NRBM), HFNC (for 2 days), or NIPPV (for at least 8hrs/day for 2 days)
- Primary outcome: Intubation rates, and the data did not show a difference between the groups in rates of intubation
- Secondary outcomes: Decrease in 90-day all-cause mortality with use of HFNC even after adjusted for illness severity (APACHE II & cardiac insufficiency)
- A post-hoc analysis showed a statistically significant reduction in intubation rate in patients with severe respiratory failure (PaO2/FiO2 ≤ 200) on Hi Flow
- A meta-analysis by Ni Y-N et al. (2) demonstrated that the use of HFNC compared to NIPPV and conventional oxygen therapy (COT) was associated with a reduction in endotracheal intubation rates in acute respiratory failure
Post-Extubation (Patients at low risk for Re-intubation)
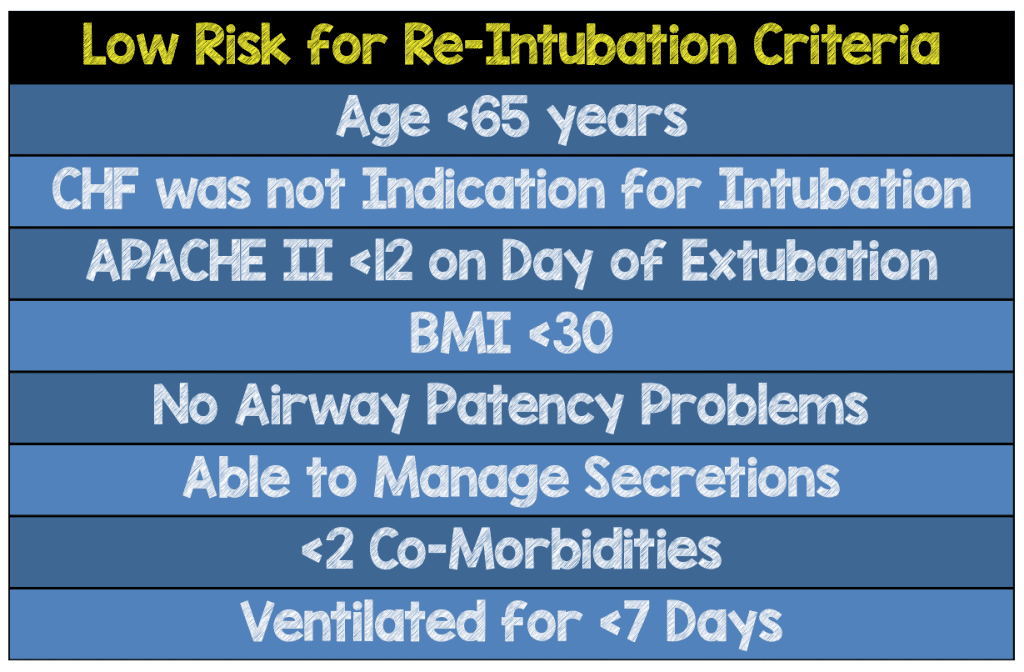 Hernandez et al (3) performed an RCT in 527 patients at LOW RISK for needing re-intubation
Hernandez et al (3) performed an RCT in 527 patients at LOW RISK for needing re-intubation- Patients were extubated to either oxygen (NC or NRBM) which would be considered the standard of care vs. HFNC
- Hi Flow therapy had re-intubation rate of 4.9% vs. Oxygen therapy of 12.2%
Pre-Oxygenation Prior to Intubation
- Can be used for pre-oxygenation prior to intubation and continued to left applied to your patient for apneic oxygenation (4 – 6).
DNR/DNI in Respiratory Distress
- Peters et al. (7) demonstrated that HFNC may be an effective therapy for patients who are DNI with acute hypoxemia and mild hypercapnia (pCO2 < 65)
- Was well tolerated and provided acceptable oxygenation without need for escalation to NIPPV in 82% of the subjects
- Provides both therapeutic and palliative benefits and may allow for patients to be treated outside the ICU
Cardiogenic Pulmonary Edema
- There isn’t a lot of really good data on this topic, however as mentioned earlier, we do know that it can change the IVC collapsibility, so there certainly may be a benefit in this domain
- Makdee et al (8) looked at this patient population to determine the effectiveness of HFNC compared to Oxygen (NC or NRBM) in the ED
- More data needed but may be a reasonable therapy for those not able to tolerate NIPPV
Pediatric Indications:
Bronchiolitis
- Pediatric patients with mild to severe bronchiolitis has the most evidence to support its use
- Various studies showing that it may decrease need for intubation (9 – 11, 14), prevention of ICU admission (9 – 10), and may be as efficacious as NIPPV in prevention of intubation (11, 14)
Other Uses in Pediatrics:
- Outside of bronchiolitis there is limited data however here are some current uses:
- Asthma (12, 14): I frequently use in asthma especially given heated, humidified oxygen may decrease further inflammation and bronchoconstriction and especially for its high flow rates
- Pneumonia: Much of this data I extrapolate from adult data
- Croup (12)
- Transporting Critically Ill Children from ED to Children’s Hospital PICU (13):May be as safe as NIPPV in transporting critically ill children between hospitals
- Post-Extubation (14): There is now pediatric, neonatal, and adult data supporting its use here
- Pre-oxygenation prior to Intubation: Here again I extrapolate from the adult data (and my current practice)
Is HFNC Working or Not?
When applying any therapy, it’s always important to asses if your patient is responding or not responding. A study by Kang BJ et al (7) showed that failure of HFNC, causing delayed intubation, might have worse clinical outcomes in patients with respiratory failure. So keeping a patient on HFNC too long without an adequate response may delay what is still considered the standard of care in patients with acute respiratory therapy; intubation.
I typically ask the following questions (my opinion here) when assessing my response to HFNC:
- Is my patient’s tachypnea improved?
- Is their work of breathing improved?
- Has their hypoxemia improved?
- Can I wean their fiO2 < 60% while maintaining their saturations? (Being on 60L flow & 100% fiO2 & barely maintaining their saturation targets is a failure for me!)
Roca O. et al (8) proposed an objective bedside tool using O2 sats, fiO2 and respiratory rate to predict success or failure on HFNC known as the ROX Index.
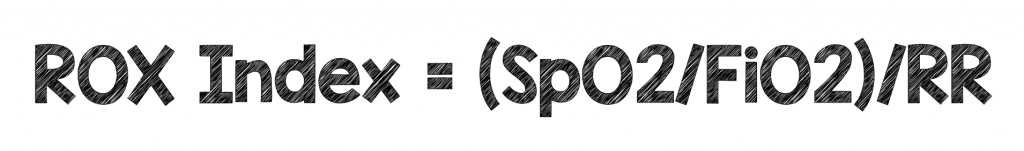
He proposed at 12-hours after initiation of HFNC, a ROX index value of ≥ 4.88 was found to be significantly associated with HFNC success. A higher ROX index score was associated with HFNC success at all time points analyzed. Interestingly, unlike Kang et al (7) this study did not find worse outcomes in patients, which were intubated after 48 hours of presentation.
In kids, predicting success using an objective tool like the ROX Index can be much more difficult as respiratory rate can vary with age. Abboud PA et al (8) retrospectively looked at children with viral bronchiolitis who failed HFNC (needing intubation) compared to children who were successful. Improved respiratory rate and clearance of repeat pCO2 were predictors of success. As of now we do not have enough information to recommend an objective measure to determine success or failure with HFNC. However with any therapy, we must re-asses our patient’s response clinically to see if they are responding to HFNC. So it is important that you have some measures that you are assessing clinically to determine if HFNC is working or not.
Practical Tips For High Flow Use:
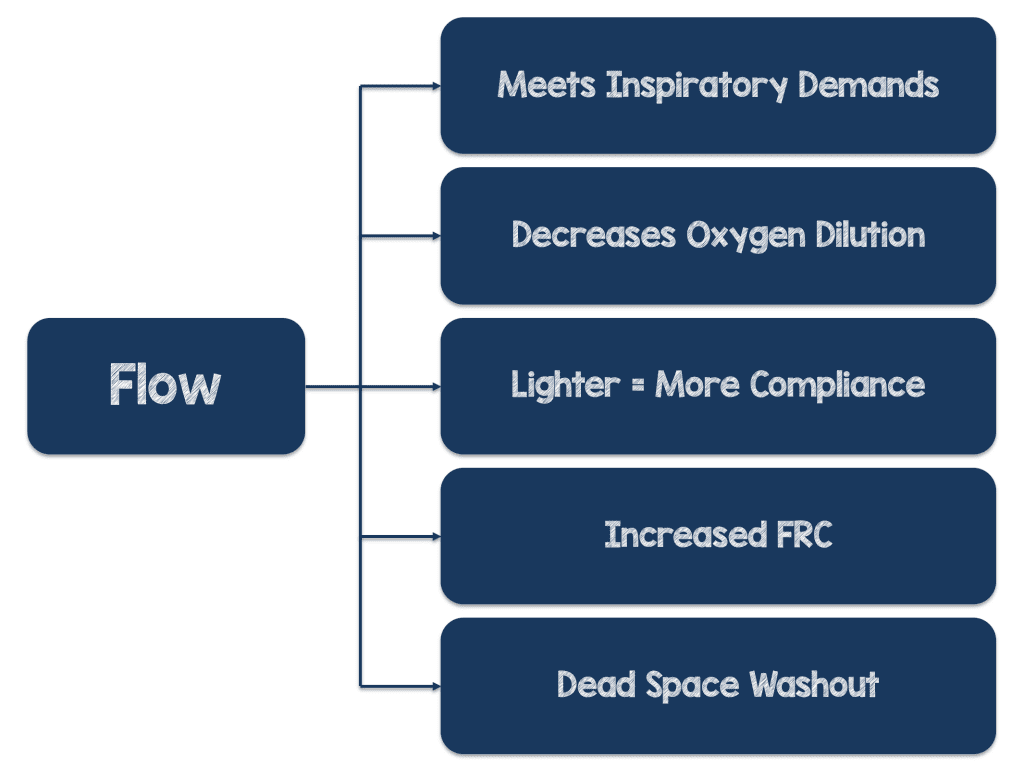
- Most of the benefits are from the high flow rates (of course the heating & humidification of gas is significant), SO OPTIMIZE THE FLOW TO START!!!
- Adult devices max out at 50-60 L/Min (max it out to start) and the dose for pediatric patient’s (based on trials) is 2L/Kg/Min
- Maximize your devices flow rate initially and wean the fi02 to maintain your oxygen saturation goal (patients typically don’t need to be left on 100%)
- Barely maintaining saturations on fi02 >60% is failing to me!!!
- If HFNC is going to be successful, then optimize the flow initially!
Guest Post Co-Written By
Frank Lodeserto, MD
AND:

Thomas Lettich, D.O.
Internal Medicine/Pediatrics Resident Physician
Geisinger Medical Center
Danville, Pennsylvania
References:
- Frat JP et al. High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure. NEJM 2015. PMID: 25981908
- Ni LJ et al. Can High-flow Nasal Cannula Reduce the Rate of Endotracheal Intubation in Adult Patients With Acute Respiratory Failure Compared With Conventional Oxygen Therapy and Noninvasive Positive Pressure Ventilation? A Systematic Review and Meta-analysis. Chest 2017. PMID: 28089816
- Hernandez G et al. Effect of Postextubation High-Flow Nasal Cannula vs. Conventional Oxygen Therapy on Reintubation in Low-Risk Patients: A Randomized Clinical Trial. JAMA 2016. PMID: 26975498
- Ricard, JD et al. Hazards of Intubation in the ICU: Role of Nasal High Flow Oxygen Therapy for Preoxygenation and Apneic Oxygenation to Prevent Desaturation. Minerva Anestesiol 2016. PMID: 27152499
- Miguel-Montanes R et al. Use of High-Flow Nasal Cannula Oxygen Therapy to Prevent Desaturation During Tracheal Intubation of Intensive Care Patients with Mild-to-Moderate Hypoxemia. Crit Care Med 2015. PMID: 25479117
- Ni LJ, et al The Effect of High-Flow Nasal Cannula in Reducing the Mortality and the Rate of Endotracheal Intubation When used Before Mechanical Ventilation Compared with Conventional Oxygen Therapy and Noninvasive Positive Pressure Ventilation. A Systematic Review and Meta-Analysis. American Journal of Emergency Medicine 2017. PMID: 28780231
- Peters SG et al. High-Flow Nasal Cannula Therapy in Do-Not-Intubate Patients With Hypoxemic Respiratory Distress. Respiratory Care 2013. PMID: 22781059
- Makdee O et al. High-Flow Nasal Cannula Versus Conventional Oxygen Therapy in Emergency Department Patients With Cardiogenic Pulmonary Edema: A Randomized Controlled Trial. Ann Emerg Med 2017. PMID: 22781059
- Kepreotes E et al. High-Flow Warm Humidified Oxygen Versus Standard Low-Flow Nasal Cannula Oxygen for Moderate Bronchiolitis (HFWHO RCT): An Open, Phase 4, Randomised Controlled Trial. Lancet 2017. PMID: 28161016
- Franklin D et al. A Randomized Trial of High-Flow Oxygen Therapy in Infants with Bronchiolitis. NEJM 2018. PMID: 29562151
- Schibler A et al. Reduced Intubation Rates for Infants after Introduction of High-Flow Nasal Prong Oxygen Delivery. Intensive Care Med 2011. PMID: 21369809
- Wing, R et al. Use of High-Flow Nasal Cannula Support in the Emergency Department Reduces the Need for Intubation in Pediatric Acute Respiratory Insufficiency. Pediatr Emerg Care 2012. PMID: 23114231
- Schlapbach LJ et al. High-Flow Nasal Cannula (HFNC) Support in Interhospital Transport of Critically ill Children. Intensive Care Med 2014. PMID: 24531340
- Christophe M et al. High-Flow Nasal Cannula: Recommendations for Daily Practice in Pediatrics. Ann Intensive Care 2014. PMID: 25593745
- Kang BJ et al. Failure of High-Flow Nasal Cannula Therapy may Delay Intubation and Increase Mortality”. Intensive Care Med 2015. PMID: 25691263
- Roca O et al. Predicting Success of High-Flow Nasal Cannula in Pneumonia Patients with Hypoxemic Respiratory Failure: The Utility of the ROX Index. Journal of Critical Care 2016. PMID: 27481760
- Abboud PA et al. Predictors of Failure in Infants with Viral Bronchiolitis Treated with High- Flow, High-Humidity Nasal Cannula Therapy. Pediatric Critical Care Medicine 2012. PMID: 22805160
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)



