 Preoxygenation and apneic oxygenation are key in emergency airway management, prevention of desaturation, and very important to patient safety. One of the best papers I have ever read on this was written by Scott D. Weingart (@emcrit) and Richard M. Levitan (@airwaycam) in the Annals of Emergency Medicine in March 2012. This article reviewed techniques in preoxygenation and peri-intubation oxygenation in adult patients requiring tracheal intubation.
Preoxygenation and apneic oxygenation are key in emergency airway management, prevention of desaturation, and very important to patient safety. One of the best papers I have ever read on this was written by Scott D. Weingart (@emcrit) and Richard M. Levitan (@airwaycam) in the Annals of Emergency Medicine in March 2012. This article reviewed techniques in preoxygenation and peri-intubation oxygenation in adult patients requiring tracheal intubation.
Is preoxygenation before tracheal intubation important? [1]
- Extends the duration of “safe apnea” = time until a patient reaches an 02 sat of 88 – 90%
 Patients breathing room air (PaO2 ≈ 90 – 100mmHg) before rapid sequence intubation (RSI) can desaturate in 45 – 60 seconds after sedative/paralytic administration
Patients breathing room air (PaO2 ≈ 90 – 100mmHg) before rapid sequence intubation (RSI) can desaturate in 45 – 60 seconds after sedative/paralytic administration- “Safe apnea” in adult patients with preoxygenation before RSI was shown to be: [cite source=”pubmed”]13713131[/cite]
- 100% FiO2 = 4 min to desaturation
- 50% FiO2 = 2 min to desaturation
- 33% FiO2 = 1 min to desaturation
- Room Air (21% FiO2) = 15 – 30 seconds to desaturation
- Goals in the ED for preoxygenation should include:
-
- Achieve an 02 saturation of 100%
- Maximize oxygen storage in the lungs by denitrogenation of the residual capacity of the lungs (Approximately 95% of oxygen reservoir)
- Maximize oxygen storage in the bloodstream (Approximately 5% of oxygen reservoir)
- Conclusion: Preoxygenation prolongs the duration of “safe apnea.”
What is the optimal period of time and best source of high FiO2 for preoxygenation? [1]
 Optimal Time:
Optimal Time:
- 3 minutes of tidal volume breathing (normal respiratory pattern) with a high FiO2 source
- 8 vital capacity breaths (maximal inhalation and maximal exhalation) with a high FiO2 source in cooperative patients
- Optimal Source:
- Standard nonrebreather at 15L/minute will deliver 60 – 70% FiO2
- The FiO2 can be increased to ≥90% by increasing the flow rate to 30 – 60L/min
- Conclusion: A standard reservoir face mask with a flow rate of oxygen set as high as possible for a total of 3 minutes or 8 vital capacity breaths is the optimal time and source of FiO2 in preoxygenation
Can use of positive-pressure ventilation help with preoxygenation? [1]
- In patients who do not achieve an O2 saturation of >93 – 95% with 3 minutes of high FiO2 consider using positive pressure ventilation
 These patients most likely have shunt physiology (i.e.alveoli are perfused but not ventilated), and require positive pressure ventilation and not more O2 to increase their oxygen saturation
These patients most likely have shunt physiology (i.e.alveoli are perfused but not ventilated), and require positive pressure ventilation and not more O2 to increase their oxygen saturation- This is extremely useful in obese patients: [2]
- 66 patients with BMI of approximately 46 kg/m2
- 5 minutes of pre oxygenation with non-invasive positive pressure ventilation (NIPPV) vs spontaneous breathing of 100% FiO2
- After preoxygenation, NIPPV group had a mean SpO2 of 98% vs spontaneous breathing group of 93%
- During intubation NIPPV group only decreased SpO2 to 93% vs spontaneous breathing group of 81%
- Positive pressure can be applied in one of three ways:
-
- Continuous Positive Airway Pressure (CPAP)
- NIPPV
- Positive End-expiratory pressure (PEEP) valves on a bag valve mask (BVM)
- Conclusion: Positive pressure ventilation should be considered in patients who cannot achieve an oxygen saturation greater than 93 – 95% with high FiO2
What is the optimal position for a patient to get preoxygenation? [1]
- Preoxygenation for 3 – 5 minutes in a 20° head up position vs supine position:
 386 seconds vs 283 seconds to desaturate from 100% to 95% O2 saturation [3]
386 seconds vs 283 seconds to desaturate from 100% to 95% O2 saturation [3]- 452 seconds vs 364 seconds to desaturate to 93% [4]
- 214 seconds vs 162 seconds to desaturate to 92% in patients with BMI > 40 kg/m2 [5]
- Also consider reverse Trendelenburg position (head of bed 30º higher than foot) in trauma patients
- Conclusion: Preoxygenation should occur in a head-elevated position to increase “safe apnea”
After preoxygenating patients, how long will it take until they desaturate? [1]
- The lungs hold 450 mL of oxygen when breathing room air but can increase to 3000 mL when breathing 100% O2 and replacing alveolar nitrogen
 Oxygen consumption is about 250 mL/minute or 3mL/kg/minute
Oxygen consumption is about 250 mL/minute or 3mL/kg/minute- A healthy person on room air can have a period of “safe apnea” of ≈ 1 minute
- A healthy person on high FiO2 can have a period of “safe apnea” of ≈ 8 minutes
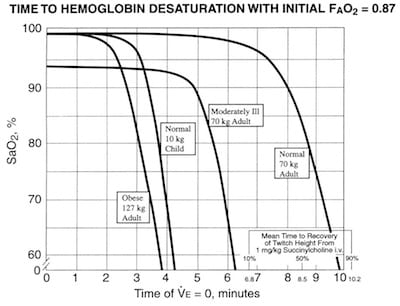
- One study showed time to desaturation of < 90% O2 saturation after succinylcholine administration was 8 minutes (healthy patients), 5 minutes (moderately ill adults), and 2.7 minutes (obese adults) which is shown in the image to the right. [6]
- Conclusion: It is difficult to predict the time to desaturation after preoxygenation in the ED, but it is important to remember that critically ill and obese patients can desaturate quickly.
What is apneic oxygenation and can it extend the duration of “safe apnea”? [1]
- Apneic Oxygenation:
- In apneic patients approximately 250mL/minute of oxygen will move from the alveoli to the blood stream
- At the same time approximately 8 – 20 mL/minute of carbon dioxide moves into the alveoli
- This difference in movement across the alveolar membrane causes the net pressure in the alveoli to become slightly subatmospheric
 Generation of a flow of gas from the pharynx to the alveoli is therefore created (i.e. apneic oxygenation)
Generation of a flow of gas from the pharynx to the alveoli is therefore created (i.e. apneic oxygenation)
- Duration of “Safe Apnea”:
- Study 1: In the operating room at the time of apnea, 5 L/min O2 via nasal cannula vs no O2 was tested to show time to desaturation of 95% and showed no desaturation out to 6 minutes in nasal cannula group vs 3.65 minutes in the no O2 group [7]
- Study 2: Obese patients in the operating room at the time of apnea, 5L/min O2 via nasal cannula vs no O2 was tested to show time to desaturation of ≥95% and showed a time of 5.29 minutes vs 3.49 minutes respectively [8]
- Nasal cannula is the device of choice to provide apneic oxygenation and can be left on during pre oxygenation, bag valve mask ventilation, and during attempts for tracheal intubation.
- Conclusion: Apneic oxygenation can extend the time of “safe apnea” and nasal cannula is the device of choice
During the apneic period when should manual ventilations be initiated? [1]
- During the onset of muscle relaxation two major benefits of ventilation are:
-
 PaCO2 increases 8 – 16 mmHg in 1st minute of apnea and then ≈3mmHg/minute after that. May need to hyperventilate patients with severe metabolic acidosis (for compensation of acidosis) and increased intracranial pressure (Increased PaCO2 increases cerebral vasodilatation).
PaCO2 increases 8 – 16 mmHg in 1st minute of apnea and then ≈3mmHg/minute after that. May need to hyperventilate patients with severe metabolic acidosis (for compensation of acidosis) and increased intracranial pressure (Increased PaCO2 increases cerebral vasodilatation).- Increase oxygenation through alveolar distention, which increases the period of “safe apnea.”
- Aggressive ventilation can lead to regurgitation and aspiration
- Be mindful of rate, volume, and speed of ventilation in critically ill patients as this can decrease venous return, resulting in hypotension
- Conclusion: Be sure to weigh the risks and benefits of active ventilation during the onset of muscle relaxation
What is the optimal positioning of patients during apneic oxygenation? [1]
- The optimal position is having the external auditory meatus on the same horizontal plane as the sternal notch
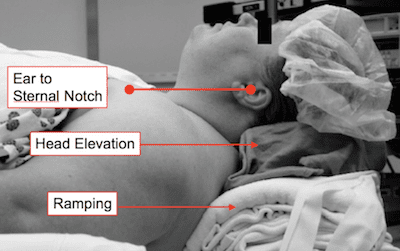 The key maneuvers to relieve obstruction of airways are: head elevation, chin lift, and jaw thrust.
The key maneuvers to relieve obstruction of airways are: head elevation, chin lift, and jaw thrust.- Cricoid pressure can cause lateral displacement o the esophagus and laryngeal/tracheal compression hindering BVM ventilation and reducing tidal volumes
- Conclusion: The optimal position during the apneic period is using an ear-to-sternal notch positioning and cricoid pressure may have a negative effect on apneic oxygenation.
What is the paralytic agent of choice to increase “safe apnea”? [1]
 Study 1: Time to desaturation of 95% was 242 seconds (succinylcholine) vs 378 seconds (rocuronium) [9]
Study 1: Time to desaturation of 95% was 242 seconds (succinylcholine) vs 378 seconds (rocuronium) [9]- Study 2: Time to desaturation of 92% was 283 seconds (succinylcholine) vs 329 seconds (rocuronium) [10]
- ≥1.2 mg/kg of rocuronium provides similar intubation conditions as succinylcholine, with one caveat that succinylcholine has a shorter duration of action. [11]
- Conclusion: Rocuronium at a dose of ≥1.2 mg/kg may provide a longer period of “safe apnea” vs succinylcholine.
Summary and Take Home Messages of Preoxygenation and Apneic Oxygenation
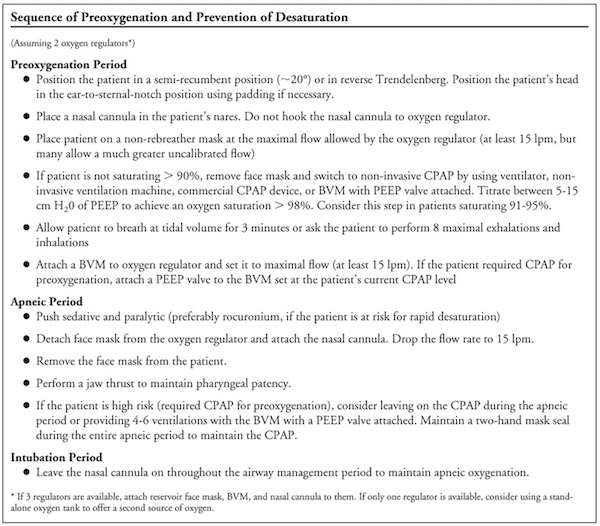
Image from [1]
For more information you can also checkout:
- Richard Levitan’s site: Airway Cam
- Scott Weingart’s site/podcast: EMCrit Blog
- Minh Le Cong’s site: PHARM Blog
References:
- Weingart SD et al. Preoxygenation and Prevention of Desaturation During Emergency Airway Management. Ann Emerg Med 2012. PMID: 22050948
- Futier E et al. Noninvasive Ventilation and Alveolar Recruitment Maneuver Improve Respiratory Function During and After Intubation of Morbidly Obese Patients: A Randomized Controlled Study. Anesthesiology 2011. PMID: 21478734
- Lane S et al. A Prospective, Randomized controlled Trial Comparing the Efficacy of Pre-Oxygenation in the 20 Degrees Head-Up vs Supine Position. Anesthesia 2005. PMID: 16229689
- Ramkumar V et al. Preoxygenation with 20 Head-Up Tilt Provides Longer Duration of Non-Hypoxic Apnea than Conventional Preoxygenation in Non-Obese Healthy Adults. J Anesth 2011. PMID: 21293885
- Preoxygenation is More Effective in the 25 Degrees Head-Up Position Than in the Supine Position in Severely Obese Patients: A Randomized Controlled Study. Anesthesiology 2005. PMID: 15915022
- Benumof JL et al. Critical Hemoglobin Desaturation Will occur Before Return to An Unparalyzed State Following 1mg/kg Intravenous Succinylcholine. Anesthesiology 1997. PMID: 9357902
- Taha SK et al. Nasopharyngeal oxygen Insufflation Following Pre-Oxygenation Using the Four Deep Breath technique. Anaesthesia 2006. PMID: 16674614
- Ramachandran SK et al. Apneic Oxygenation During Prolonged Laryngoscopy in Obese Patients: A Randomized, Controlled Trial of Nasal Oxygen Administration. J Clin Anesthesiology 2010. PMID: 20400000
- Taha SK et al. Effect of Suxamethonium vs Rocuronium on Onstet of Oxygen Desaturation During Apnea Following Rapid Sequence Induction. Anaesthesia 2010. PMID: 20402874
- Tang L et al. Desaturation Following Rapid Sequence Induction Using Succinylcholine vs. Rocuronium in Overweight Patients. Acta Anaesthesiol Scand 2011. PMID: 21226862
- Perry JJ et al. Rocuronium Versus Succinylcholine for Rapid Sequence Induction Intubation. Cochrane Database Syst Rev 2008. PMID: 18425883
Cite this article as: Salim Rezaie, "Preoxygenation and Apneic Oxygenation", REBEL EM blog, March 24, 2014. Available at: https://rebelem.com/preoxygenation-apneic-oxygenation/.