
Background: The ongoing debate between video laryngoscopy (VL) and direct laryngoscopy (DL) has ignited intense debate within the emergency medicine and critical care communities. A recent pragmatic, randomized, multicenter trial (The DEVICE Trial) compared the two techniques to determine if VL outperformed DL in first-pass success (FPS). In this blog post, we explore the study’s key findings, strengths, and limitations, providing valuable insights while navigating the complexities of airway management in critically ill adults.
REBEL Cast Ep121: The Battle of the Blades – VL vs DL
Article: Prekker ME, Driver BE, Trent SA, et al. Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults [published online ahead of print, 2023 Jun 16]. N Engl J Med. 2023;10.1056/NEJMoa2301601. PMID: 37326325.
Clinical Question: In critically ill adults (P), does the use of a video laryngoscope (I) compared to a direct laryngoscope (C) improve the first-pass success rate of intubation (O)?
What They Did:
- Investigators conducted a pragmatic, multicenter, unblinded, randomized, parallel-group trial comparing video laryngoscopy to direct laryngoscopy for tracheal intubation in critically ill patients.
- Patients meeting eligibility criteria were randomly assigned in a 1:1 ratio to undergo intubation with either video or direct laryngoscopy.
- 11 medical centers in the United States enrolled 1417 patients from 17 sites, including 7 emergency departments and 10 intensive care units.
- The Trial was registered at ClinicalTrials.gov: NCT05239195
Population:
- Critically ill adults (age ≥18 years) undergoing orotracheal intubation using a laryngoscope.
Inclusion Criteria:
- Age ≥18 years
- Patients undergoing orotracheal intubation
- The patient is located in a participating unit
Exclusion Criteria:
- Known pregnancy
- Prisoners (incarcerated or involuntarily detained)
- Immediate need for tracheal intubation that precludes randomization
- Clinician-determined necessity or contraindication for video laryngoscopy or direct laryngoscopy on the first attempt.
Intervention:
- Video Laryngoscope Group: Use of a video laryngoscope on the first intubation attempt.
Comparator:
- Direct Laryngoscope Group: Use of a direct laryngoscope on the first intubation attempt.
Outcomes:
Primary Outcome: Successful intubation on the first attempt.
- Defined as correct placement of endotracheal tube with a single insertion of laryngoscope blade and endotracheal tube or bougie.
Secondary Outcomes: Severe complications of tracheal intubation.
- Defined as one or more of the following occurring between induction and 2 minutes after successful intubation:
- Severe hypoxemia (lowest oxygen saturation measured by pulse oximetry < 80%)
- Severe hypotension (systolic blood pressure < 65 mm Hg or new or increased vasopressor administration)
- Cardiac arrest not resulting in death within 1 hour of intubation
- Cardiac arrest resulting in death within 1 hour of induction
Exploratory Outcomes:
- Duration of laryngoscopy and tracheal intubation
- Number of laryngoscopy attempts
- Number of attempts to cannulate the trachea with a bougie or an endotracheal tube
- Composite of patients who meet the primary outcome (successful intubation on the first attempt) without meeting the secondary outcome (severe complications of tracheal intubation)
- Reason for failure among those who did not meet the primary outcome
- Inadequate view of the larynx
- Inability to intubate the trachea with an endotracheal tube
- Inability to cannulate the trachea with a bougie
- Attempt aborted due to change in patient condition (e.g., worsening hypoxemia, hypotension, bradycardia, vomiting, bleeding)
- Technical failure of the laryngoscope (e.g., battery, light source, camera, screen)
- Other
- Operator-reported aspiration
- Esophageal intubation
- Injury to the teeth
- ICU-free days in the first 28 days
- Ventilator free days in the first 28 days
- All-cause in-hospital mortality
Results:
- Between March 19, 2022, and November 17, 2022, 1,947 patients were assessed for eligibility.
- 1420 patients were enrolled.
- Three patients were identified as prisoners and were excluded after enrollment.
- 1,417 patients were included in the primary analysis.
- 705 patients (49.8%) were assigned to the video-laryngoscopy cohort.
- 712 patients (50.2%) were assigned to the direct-laryngoscopy cohort.
- The most common indications for tracheal intubation were AMS (45.3%) and acute respiratory failure (30.4%).
- 69.7% of intubations were performed in the emergency department.
- An emergency medicine resident or critical care fellow performed 91.5% of intubations.
- Operators had performed a median of 50 previous tracheal intubations (Range 25 to 92)
- The median proportion of previous intubation operators performed with VL was 0.69.
- Median APACHE II score was 16 (Score range 0 to 71)
- Most intubation was anticipated to be easy to moderate, with very few anticipated as difficult (9.5% VL vs 8.7% DL).
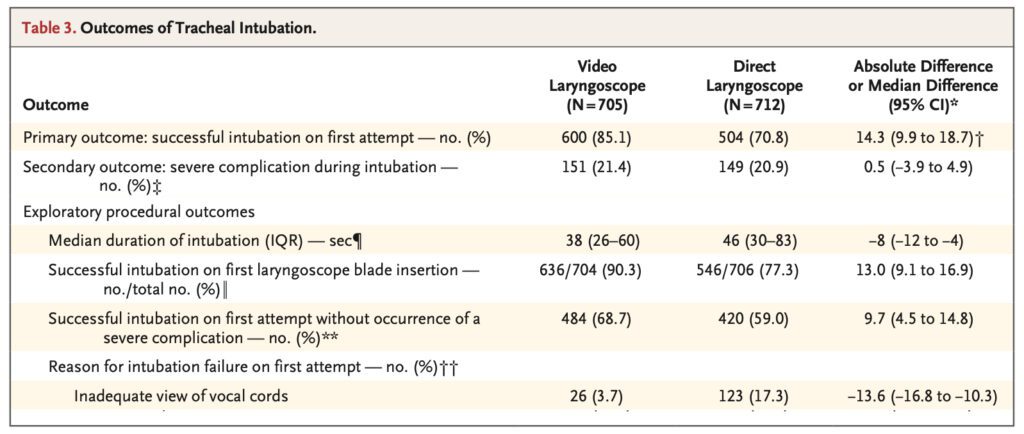
Primary Outcome:
- First-pass success was 600/705 patients (85.1%) in the VL group and 504/712 patients (70.8%) in the DL group
- The absolute risk difference was 14.3 percentage points; 95% CI, 9.9 to 18.7; P<0.001
Secondary Outcome:
- 151 patients (21.4%) in the VL group and 149 patients (20.9%) in the DL group met the secondary outcome.
- The absolute risk difference was 0.5 percentage points; 95% CI, −3.9 to 4.9.
Exploratory Outcomes:
- Successful intubation on the first attempt without severe complication: 68.7% VL vs. 59.0% DL.
- Failure to intubate trachea due to inadequate view: 3.7% VL vs 17.3% DL.
- Median time to intubation: VL 38s vs DL 46s.
Strengths:
- The study addressed a clinically relevant and heavily debated question.
- Patients were recruited from various centers and clinical site types, enhancing the external validity and generalizability of the findings.
- The pragmatic study design closely mirrored real-world clinical experiences.
- The RCT study design allows for balance in baseline characteristics and limits the potential for bias.
- Randomization was employed, and the allocation sequence was concealed, ensuring unbiased assignment of interventions.
- The trial was registered with clinicaltrials.gov, increasing transparency and facilitating reproducibility.
- The inclusion criteria were broad, allowing for a diverse patient population to be included.
- Adequate sample size determination was conducted.
- A large number of patients (>1400) were enrolled.
- Data collection was performed by a trained observer independent of the procedure, minimizing potential bias.
- Adherence to group assignments was excellent, and there were minimal missing data and protocol violations, enhancing the robustness of the analysis.
- Patients appeared to have a similar prognosis at the start of the trial, and the collected demographic information was well-balanced.
- Intention-to-treat analysis was performed by the investigators, ensuring the integrity of the treatment comparisons.
- Multiple sensitivity analyses were conducted, accounting for factors such as trial site, protocol violations, and missing data, and an additional analysis where the operator had a similar proportion of previous intubations with VL and DL.
- Predetermined stop criteria were utilized during interim analysis.
Limitations:
- The study was conducted in a single country, limiting its generalizability to other regions or populations.
- Most facilities were teaching hospitals, limiting generalizability to community hospitals.
- Although the overall sample size was large, only 387 unique operators were involved, which may affect the variability and representativeness of the results.
- Clinicians and research personnel were unblinded, potentially introducing bias in the study outcomes.
- The primary outcome, FPS, is disease-oriented, and components of the secondary outcome were also disease-oriented.
- The secondary outcome is a composite measure, combining multiple factors, which can make interpretation and analysis more complex.
- Important information regarding the mode of oxygenation, medication types and dosages used for induction and paralytic agents, and other therapies that could impact the secondary outcomes are not provided, potentially introducing bias.
- Airway assessments, such as the anticipated difficulty of the procedure and Cormack-Lehane grade of view, are subjective and prone to variability influenced by individual operators.
- Investigators assumed a FPS of 80% in the DL cohort but only achieved 70%.
- The trial was prematurely stopped due to observed benefits, which could overestimate the results and limit the completeness of the findings.
- The trial did not specify the specific brand of video laryngoscope or blade shape used, creating uncertainty regarding how these factors may have influenced operator performance and introducing a source of variability in the data.
- Most intubations were performed with a standard geometry blade, limiting the generalizability to other blade shapes, such as the hyper-angulated and miller blades.
- Most intubations (70%) were performed in the emergency department, potentially influencing the generalizability of the results to other clinical settings.
- More than 90% of the intubations were performed by emergency medicine residents and critical care fellows, indicating that operators consisted primarily of trainees.
- The majority of operators had minimal intubation experience; therefore, the results may not apply to operators with more experience.
- Operators reported a median of 69% of their previous intubations utilizing VL, suggesting a higher baseline proficiency with VL and biasing results favoring VL.
Discussion:
Study Outcomes:
- The primary outcome of FPS is commonly used in comparative trials evaluating intubation devices, including this study. While FPS provides a measurable parameter for comparison with existing literature, it is primarily a disease-oriented outcome. Similarly, components of the secondary outcomes, such as severe hypoxemia and severe hypotension, are also disease-oriented.
- The study did not find a statistically significant difference in the secondary outcome between DL and VL interventions. While interesting, it is essential to consider the limitations of interpreting these outcomes within a 2-minute timeframe. In clinical practice, physicians would typically intervene before patients reach critically low levels of oxygenation or blood pressure.
- Furthermore, the study lacks detailed information on essential factors such as the specific mode of preoxygenation, the types and dosages of medications administered during intubation, and other therapies provided, such as intravenous fluids. These details are crucial because differences in preoxygenation modalities, medications, and dosages can significantly impact the components measured in the secondary outcome. Without granular information on these factors, fully understanding the potential effects of DL and VL interventions on the measured secondary outcomes is challenging.
The Operator:
- Investigators found a statistically significant difference in FPS favoring VL over DL for FPS (absolute risk difference, 14.3 percentage points; 95% CI, 9.9 to 18.7; P<0.001). However, several operator-specific factors need consideration. The study involved 387 unique operators who performed a total of 1400 intubations. Any limitations specific to individual operators may be compounded as they perform more intubations.
- Emergency medicine residents and critical care fellows performed most (91%) intubations. These operators had a median of 50 prior intubations. Notably, just under two-thirds of operators used VL in 25% to 75% of their previous intubations, more than one-third used VL in >75% of previous intubations, and only 5% of operators used VL in <25% of previous intubations. Therefore, the operators in this study can be considered relatively inexperienced, with a higher baseline proficiency in VL.
- Although there was no disparity in the anticipated intubation difficulty, the Cormack-Lehane grade 1 view was achieved in 76.3% of intubations using VL compared to only 44.7% with DL. This indicates that operators could visualize the anatomy more effectively with VL, resulting in a superior view and increased likelihood of FPS.
- The likelihood of successful intubation on the first attempt is increased when using video laryngoscopy (VL) for operators at all experience levels. However, the difference in the primary outcome between groups seems to be most prominent among the least experienced operators. This is likely because operators with less familiarity with anatomical landmarks derive greater benefit from improved laryngeal visualization provided by VL. Additionally, VL allows for real-time feedback from a second clinician, further contributing to its effectiveness.
- Furthermore, researchers observed that operators with fewer than 25 intubations had an absolute risk difference of 26.1%, which decreased to 5.9% (95% CI, -4.1 to 16.0) among operators with over 100 prior intubations. These findings indicate that operators with less intubation experience should opt for VL. As operators gain more experience with intubation, this difference gradually diminishes.
Preparation:
- To ensure successful intubation, it is vital to meticulously plan an approach that incorporates multiple contingencies prior to any attempt. A chosen plan may be unsuccessful due to various factors. It is imperative to practice and master alternatives. While acknowledging the benefits of VL for FPS, it is equally essential to maintain proficiency in other advanced airwar techniques. Various devices, such as the C-MAC, McGrath video laryngoscope, and GlideScope with standard geometry blades, enable clinicians to switch between VL and DL using a single device seamlessly. This adaptability ensures enhanced accuracy and proficiency in both techniques.
Author’s Conclusion: “Among critically ill adults undergoing tracheal intubation in an emergency department or ICU, the use of a video laryngoscope resulted in a higher incidence of successful intubation on the first attempt than the use of a direct laryngoscope.”
Our Conclusion:
This study comparing VL to DL for tracheal intubation in critically ill adults revealed that VL was associated with a higher incidence of FPS compared to DL. However, most operators were relatively inexperienced trainees with a higher baseline proficiency in VL. VL offers advantages in visualizing the anatomy and facilitating FPS for intubation, particularly for clinicians in specialty training. However, there is some signal that the benefit of VL diminishes as technical proficiency increases.
Clinical Bottom Line:
We recommend VL with a standard geometry blade, allowing for a seamless transition to DL if needed. Additionally, employing VL provides resident physicians with valuable hands-on experience while ensuring optimal visualization and patient safety under attending physician supervision.
Post-Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)




