REBEL Core Cast 110.0 – On Shift Learning Pearls
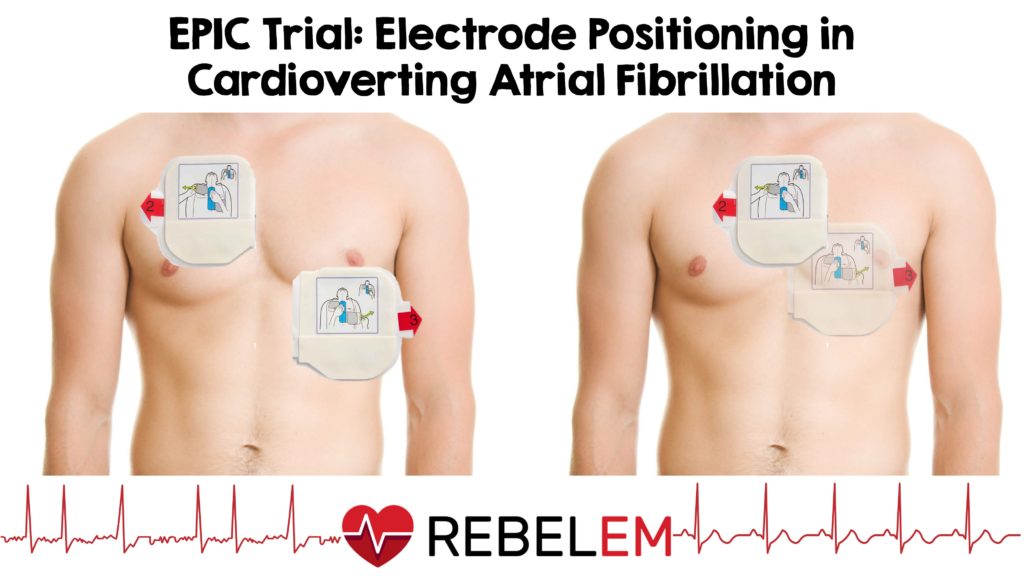
Take Home Points: Patients with recent onset atrial fibrillation can safely be cardioverted if they are 1) on anticoagulation 2) Low risk based on CHADS-VASC with onset < 48 hours or 3) High risk based on CHADS-VASC with onset < …