“It is important to realize that guidelines cannot always account for individual variation among patients. They are not intended to supplant physician judgment with respect to particular patients or special clinical situations. IDSA considers adherence to these guidelines to be VOLUNTARY, with the ultimate determination regarding their application to be made by the physician in the light of each patient’s individual circumstances.”
REBEL Cast Episode 29: IDSA Pneumonia Update
Click here for Direct Download of Podcast
What Article Are We Reviewing:
- Kalil AC et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of america and the american thoracic society. Clinical Infectious Diseases 2016; 63(5): e61-111. PMID: 27418577
What They Did: This article is an updated guideline on the management of patients with hospital acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) based on evidence from systematic literature reviews
Definitions of Nosocomial Pneumonia:
- Health Care Associated Pneumonia (HCAP): pneumonia in a patient who has either recently been hospitalized (within the last 90 days), resided in a nursing home or long-term care facility or received parenteral antibiotics, chemotherapy or wound care within 30 days.
- Hospital Acquired Pneumonia (HAP): Pneumonia occurring within 48 hours or more after a hospital admission and was not present on presentation.
- Ventilator Associated Pneumonia (VAP): Pneumonia that occurs within 48 hours of intubation that wasn’t there prior to that intubation.
What are Some of the Highlights of the 2016 IDSA Nosocomial Pneumonia Guidelines:
- In patients with suspected HAP/VAP, procalcitonin and C-Reactive Protein (CRP) testing are not recommended initially. Instead, clinical criteria alone should be used to decide whether or not to initiate empiric antibiotic treatment. However, use of procalcitonin + clinical criteria can be used to help in discontinuation of antibiotics once patients are admitted to the hospital
- Empiric antibiotics for HAP/VAP should be based on antimicrobial susceptibilities and antibiograms of local pathogens
- Patients with HAP/VAP due to Pseudomonas aeruginosa AND NOT in septic shock or high risk for death consider using monotherapy instead of double coverage
- Length of Therapy for HAP/VAP is a 7-day course of appropriate antibiotics
- The big change in this document, and the highlight this blog post/podcast is going to focus on, is that the Health Care Associated Pneumonia (HCAP) no longer appears alongside HAP and VAP in the treatment recommendations. Prior guidelines stated that HCAP patients were at a higher risk for multi-drug resistant organism (MDRO) infections like HAP and VAP patients and, thus, required broad spectrum antibiotics.
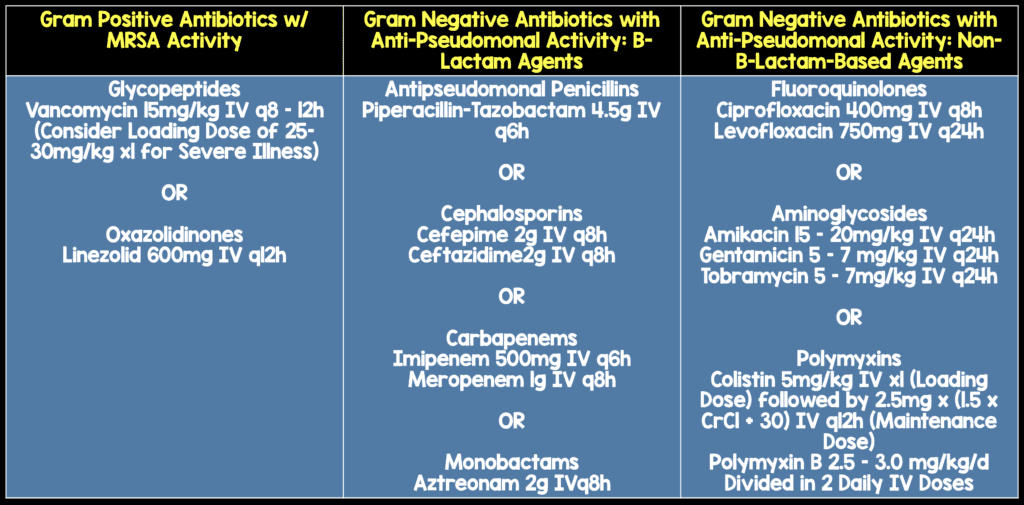
Ventilator Associated Pneumonia Recommended Treatment (Table Modified from [1])
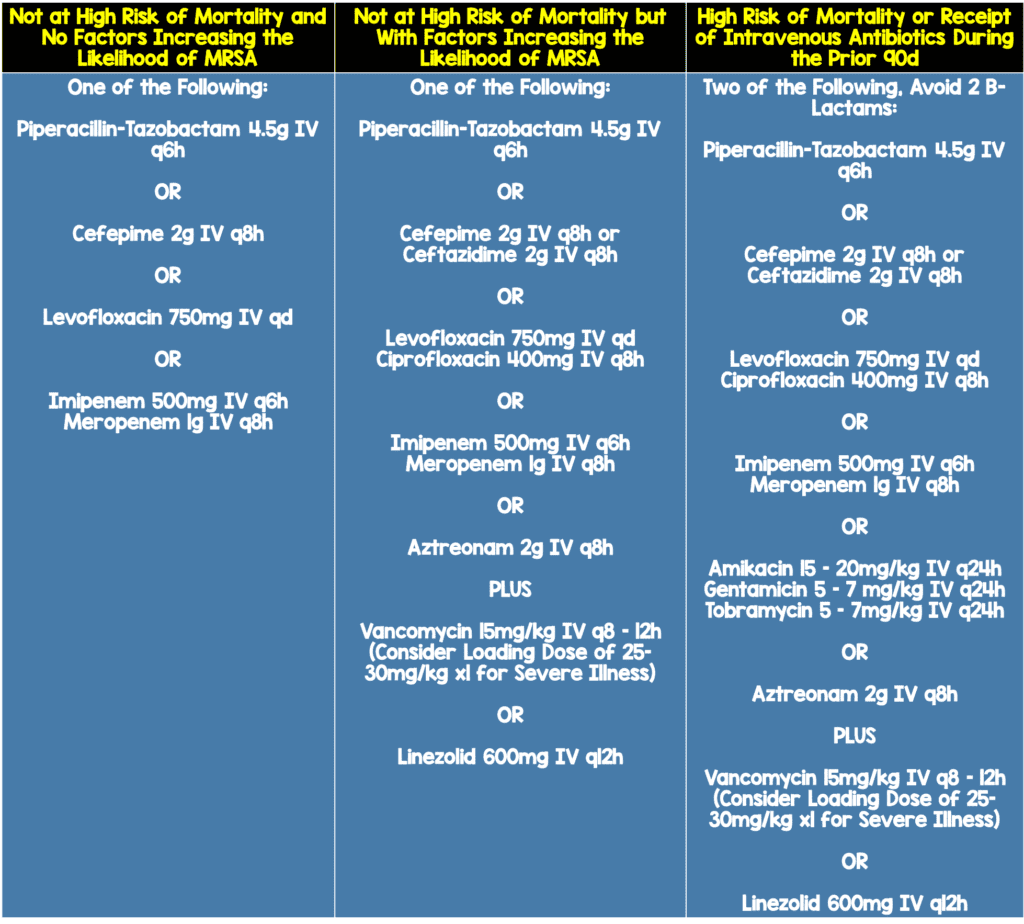
Hospital Acquired Pneumonia Treatment Recommendations (Modified Table 4 from [1])
Why was HCAP Removed in 2016:
This group reviewed a systematic review and meta-analysis of 24 studies and > 22,000 patients published in 2014 that concluded that the designation HCAP does not accurately identify patients with a risk of resistant pathogens (Chalmers 2014). This data was likely a large part of the change.
This change doesn’t mean that HCAP no longer exists but it doesn’t exist in the same breath as HAP and VAP as it once did. The most useful tables in terms of HAP and VAP are tables 3 and 4 which detail recommended empiric antibiotic coverage.
Clinical Bottom Line:
Where does this leave us in terms of HCAP, a more relevant area in Emergency Medicine than HAP and VAP. The truth is that we don’t know. As mentioned in the podcast, many of us see patients who were recently admitted for unrelated issues who now return with pneumonias but are very well appearing and without significant comorbid conditions. Uniformly, admitting these patients and treating them with broad spectrum antibiotics never made sense. It will be interesting to see what subsequent IDSA recommendations are for the treatment of HCAP and how this affects our treatment decisions. For now, in well appearing patients who are otherwise healthy with unremarkable vital signs, we are recommending treating HCAP in the same way we treat community acquired pneumonia and ensuring close follow up and giving explicit return precautions.
For More on This Topic Checkout:
References:
- Kalil AC et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of america and the american thoracic society. Clinical Infectious Diseases 2016; 63(5): e61-111. PMID: 27418577
- Chalmers JD et al. Healthcare-associated pneumonia does not accurately identify potentially resistant pathogens: a systematic review and meta-analysis. Colin Infect Dis 2014; 58(3): 330-9. PMID: 24270053
Post Peer Reviewed By: Salim R. Rezaie (Twitter: @srrezaie)



