To go back to the main post, click on the image below…
COVID-19 Prevention
- General Prevention:
- The focus should be on hygiene and isolation
- Wash hands often with soap and water
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol
- Avoid touching your eyes, nose, and mouth with unwashed hands
- Implement Contact Precautions (Human coronaviruses can remain infectious on inanimate objects from 2hrs up to 9d)[6]
- Implement Airborne Precautions
- In one publication viable SARS-CoV-2 was detected via aerosol and inanimate objects [1]:
- Aerosols: ≈3hrs post aerosolization (median half-life: 1.1 – 1.2hrs)
- Copper: ≈4hrs
- Cardboard: up to 24hrs
- Stainless Steel: 2 – 3d (median half-life: 5.6hrs)
- Plastic: 2 – 3d (median half-life: 6.8hrs)
- The focus should be on hygiene and isolation
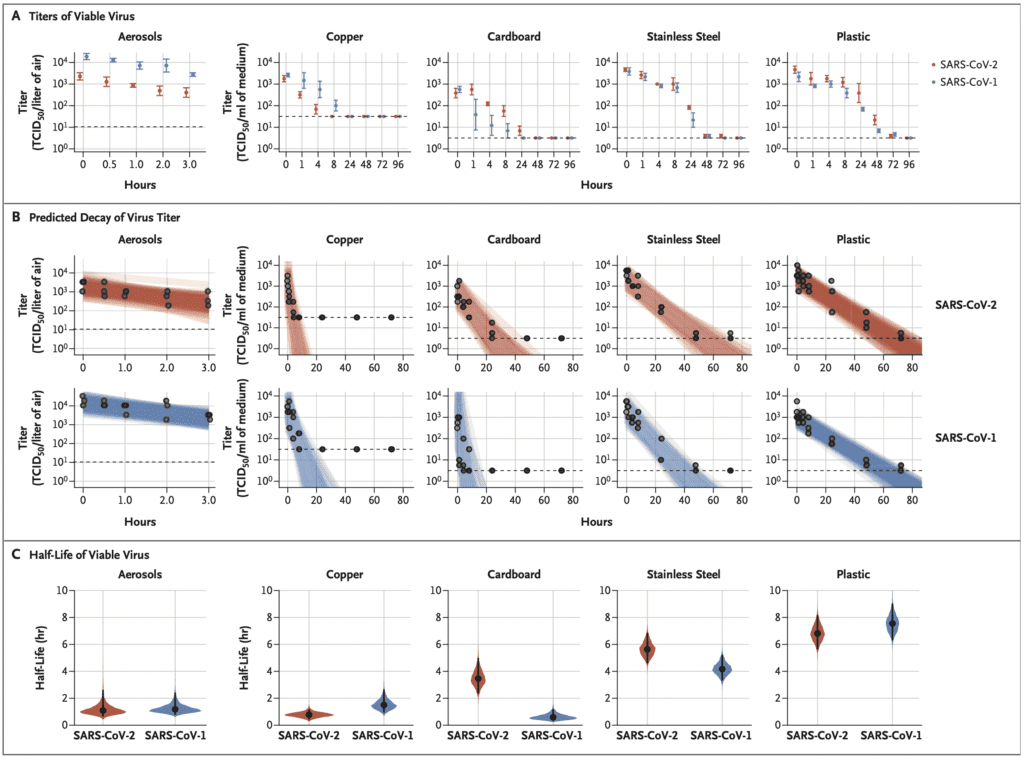
Image from NEJM [1]
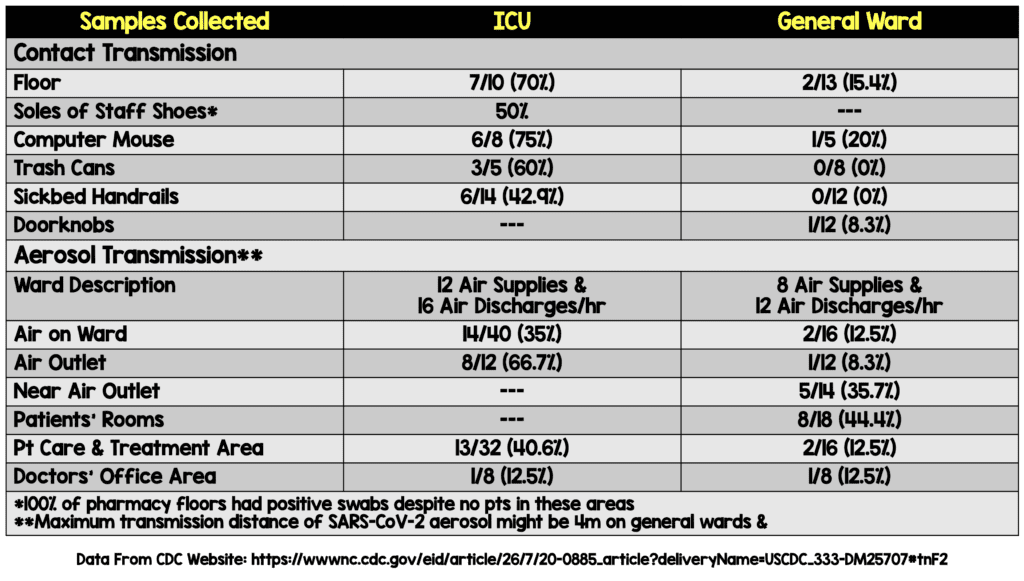
- Swab Samples Collected from Contaminated Objects & Air Samples in the ICU and General Ward in China [Link is HERE]
-
- No staff members in these wards were infected with SARS-CoV-2 (i.e. virus detected ≠ infection)
- Recovery of virus does not necessarily reflect the potential to pick up the virus from casual contact
- Limitations:
- Results of nucleic acid test do not indicate amount of viable virus
- The minimal infectious dose and aerosol transmission distance cannot be strictly determined by this study
- Conclusions:
- SARS-CoV-2 was found in the air and on object surfaces in both the ICU and general ward which implies a high infection risk for medical staff
- Environmental contamination was ICU > General Ward
- Aerosol distribution in the general ward indicates that the transmission distance might be 4m
Social distancing – This will help keep mortality as low as possible without overwhelming the healthcare system
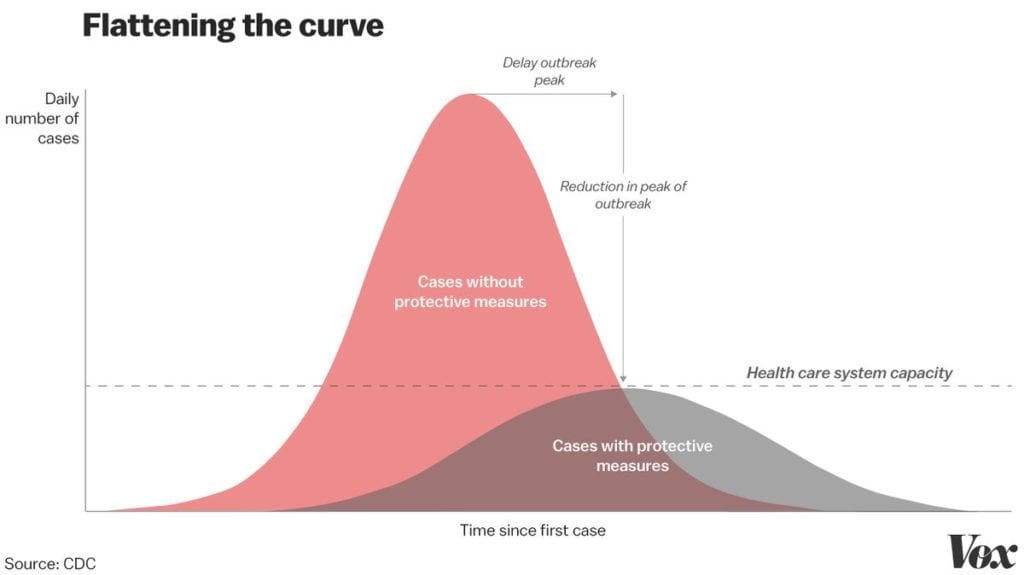
Image from Vox Website
- Masks:
- WHO recommends the use of surgical masks for patients with respiratory symptoms, which prevents suspected individuals from spreading disease
- Surgical Mask: Loose mask used for common respiratory viruses that spread via droplets (travel short distances) and transmitted by cough or sneeze. They prevent the person wearing the mask from spreading large sprays or droplets as well as preventing hand-to-face contact
- Currently, face masks are not recommended to be worn in healthy individuals for protection against acquiring respiratory infection, as there is no evidence that face masks are effective in preventing people from becoming ill
- CDC recommends the use of properly fitted N-95 masks in healthcare workers, but not for general public use in suspected and confirmed cases
- UPDATED CDC Recs (03/10/2020): [Link is HERE]
- Based on local and regional situational analysis of PPE supplies, facemasks are an acceptable alternative when the supply chain of respirators cannot meet the demand. During this time, available respirators should be prioritized for procedures that are likely to generate respiratory aerosols, which would pose the highest exposure risk to HCP.
- Facemasks protect the wearer from splashes and sprays.
- Respirators, which filter inspired air, offer respiratory protection.
- When the supply chain is restored, facilities with a respiratory protection program should return to use of respirators for patients with known or suspected COVID-19.
- Based on local and regional situational analysis of PPE supplies, facemasks are an acceptable alternative when the supply chain of respirators cannot meet the demand. During this time, available respirators should be prioritized for procedures that are likely to generate respiratory aerosols, which would pose the highest exposure risk to HCP.
- N95 Masks: Tight fitting mask that prevent inhalation of smaller infectious particles that can spread through the air over long distances (i.e. tuberculosis, chickenpox, measles, etc…). N95 masks should not be used by individuals with facial hair or children as it is difficult to achieve a proper fit (In these cases a power air-purifying respirator, or PAPR for short, should be used instead).
- There has been lots of confusion regarding the CDC and WHO guideline recommendations for healthcare workers.
- SARS-CoV-2 spread is by droplet (and contact). There the use of eye protection, and surgical mask should take care of droplet precautions
- Airborne precautions and N95 masks should be reserved for pressures resulting in aerosolization (NIV, Nebs, HFNC, Intubation, etc…). This is very important because if we use N95 masks for all situations we will run out of N95 masks when they are actually needed.
- WHO recommends the use of surgical masks for patients with respiratory symptoms, which prevents suspected individuals from spreading disease
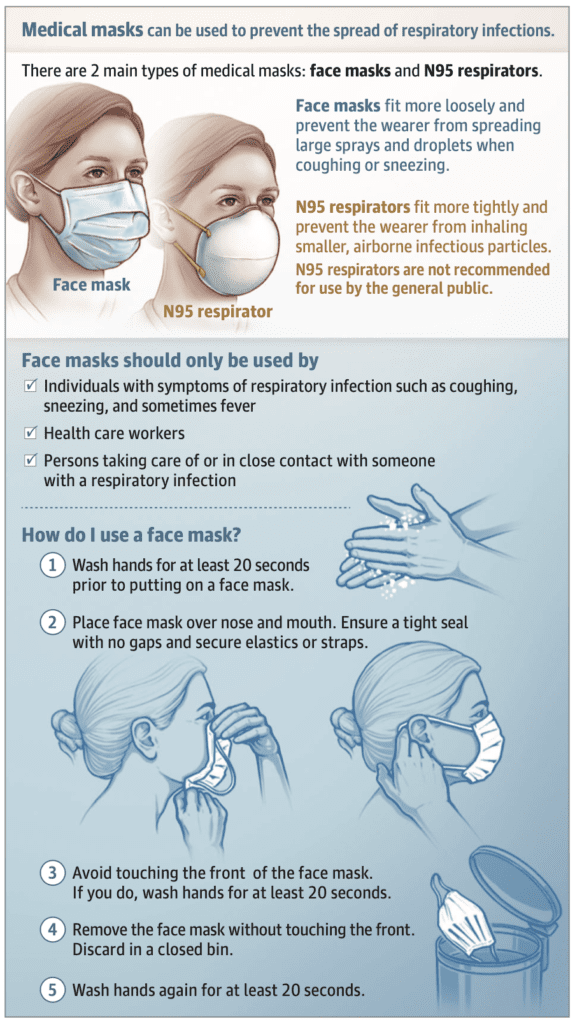
Image from JAMA Network
-
- Study out of the International Journal of Infection Control [2]:
- 30 operating room staff wore “two-ply” disposable face masks
- A blood agar plate was held 10 – 12cm away from the mouth and each person was asked to phonate “ahh”
- Samples were collected without a mask and then 30, 60, 90, 120, and 150 minutes after putting on the mask
- Bacterial counts increased to pre-wear levels by 2 hours and 30 minutes
- This is disconcerting, as viral particles are smaller than bacterial
- Study out of the International Journal of Infection Control [2]:
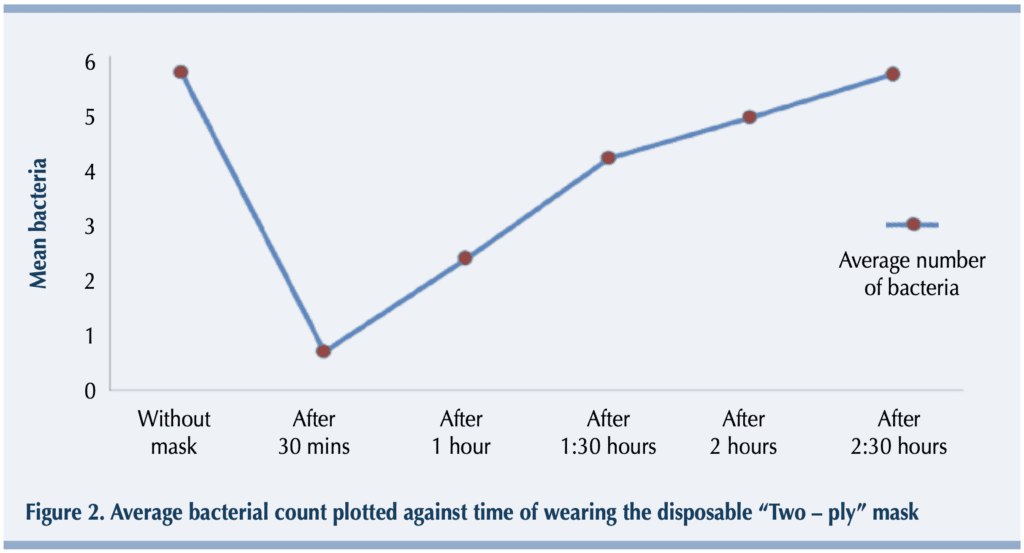
Image from [2]
-
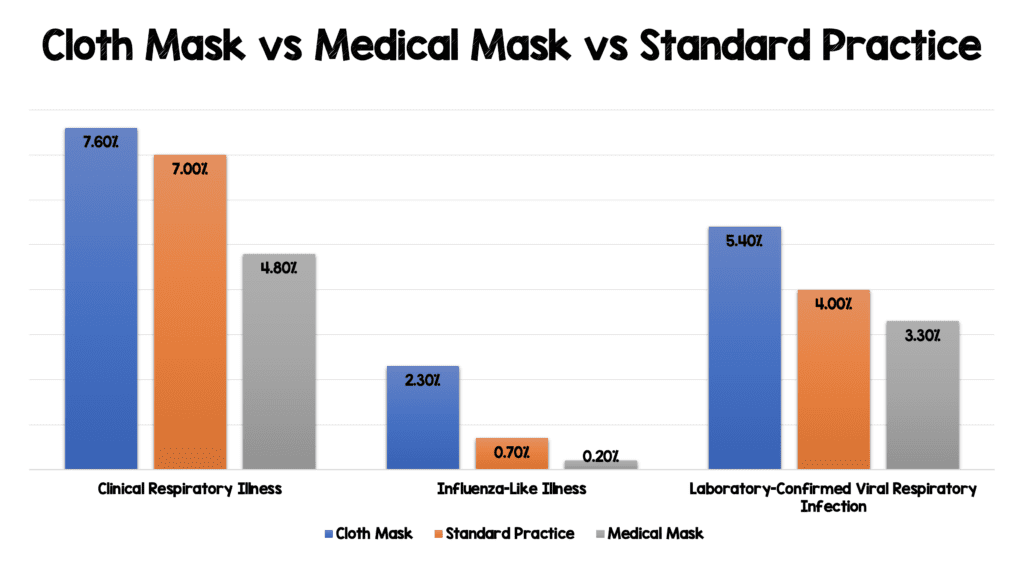
- 1607 Healthcare workers working full-time in high-risk wards[5]:
- Randomized to:
- Medical masks
- Cloth masks
- Standard practice (May or may not include mask use)
- Outcomes:
- Clinical Respiratory Illness (2 or more respiratory symptoms or one respiratory symptom + systemic symptom)
- Influenza-Like Illness (fever ≥38.0C° + one respiratory symptom)
- Laboratory-Confirmed Viral Respiratory Infection
- Results:
- Randomized to:
- 1607 Healthcare workers working full-time in high-risk wards[5]:
-
-
- Interestingly, participants with beards, long moustaches, or long facial hair were excluded
- Bottom line: Cloth masks should not be recommended for healthcare professionals
-
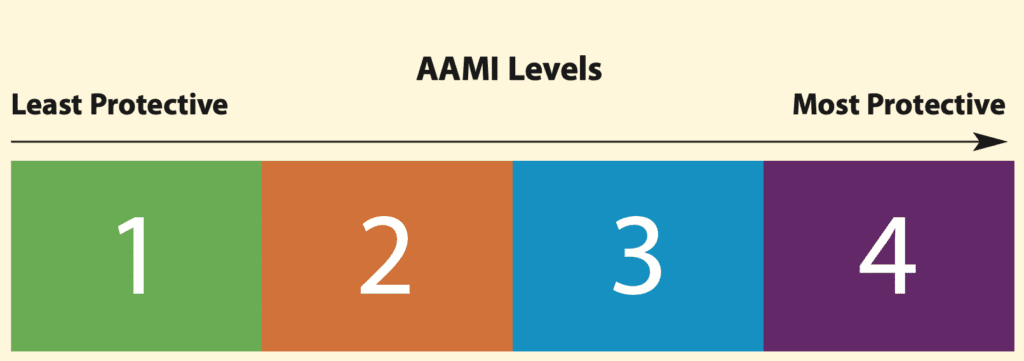
Gowns
- Level 1: Minimal level of fluid barrier protection
- Level 2: Low level of fluid barrier protection (minimum requirement)
- Level 3: Moderate level of fluid barrier protection
- Level 4: Highest level of fluid and viral barrier protection
Surface Disinfectants

- Making Disinfectant with Bleach or Calcium Hypochlorite “Shock”:
- The best sanitizer for surfaces, NOT SKIN, is made by mixing household 5% bleach in 1:50 dilution in water.
- If bleach is not available, a similar solution can be made with powdered pool-shock or calcium hypochlorite.
- Bleach Recipe:
- Add 1/3 cup of bleach in 1 gallon of water.
- Mist onto surfaces with fine mist bottles.
- Wear gloves (kitchen gloves are ideal). Bleach can be absorbed through the skin.
- Calcium Hypochlorite (alternative to bleach) Recipe:
- Slowly add 1/2 cup of granular calcium hypochlorite to a 1 gallon bleach container that is ~2/3 full of water.
- After it dissolves, fill to 1 gallon with water to make the equivalent of a “5% bleach solution”.
- To make the surface disinfectant, further dilute your “5% bleach solution” 1:50 with water. Do this by mixing 1/3 cup of this solution in 1 gallon of water.
- Mist onto surfaces with fine mist bottles.
- Caution: Calcium hypochlorite is a highly caustic compound, so follow manufacturer instructions for safety precautions..
- Making Surface Disinfectant with Benzalkonium Chloride (BAC):
- BAC 0.13% is a widely used disinfectant and is believed to be effective against viruses such as coronavirus.
- Advantages of BAC:
- Has residual killing properties and an antimicrobial effect that persists for 4 hours on skin and 24 hours on surfaces (vs. the alcohols which evaporate and quickly lose any potency).
- Safe on mucosal membranes and does not sting.
- Safest for children’s hands and less painful if there are cuts or abrasions.
- Disadvantages of BAC:
- Does not kill as quickly as the alcohols.
- One study suggests it’s less effective than the alcohols against coronavirus.
- BAC 0.13% recipe:
- Like alcohol and bleach, BAC 0.13% is becoming scarce and expensive. A more affordable method of making a large quantity follows.
- Buy benzalkonium chloride 50% (BAC50) concentrate.
- Dilute the BAC50 down to 0.13% concentration by mixing 10 ml (2 tsp) in 1 gallon of water.
- Using this method, Loren was able to buy 1 liter of concentrate for ~ $200. This made 100 gallons of hand sanitizer which he uses in his ED and has shared with staff/friends.
- BAC + alcohol may be the best “custom” sanitizer of all.
- 2.5ml of BAC 50% to 1 quart of 70% isopropyl alcohol. This yields the fast kill of alcohol and the residual (4 hour) antimicrobial effect of BAC.
- Safe for smartphones and hands
- Disinfecting Your Butterfly IQ US Probe [Link is HERE]
- PDF: Butterfly IQ Disinfection
- Wipe the probe, cable, strain relief, and connector with a Super Sani-Cloth® Germicidal (Purple Top)
- Disposable Wipe. Use additional fresh wipes as needed.
- Make sure the treated surface remains visibly wet for a minimum of two (2) minutes paying attention to seams, gaps, gasket material, and recessed areas.
- Use additional fresh wipes as needed to ensure continuous two (2) minutes of contact time.
- Allow to air dry.
- CORE Ultrasound: Handhelds, Decontamination, and Teaching
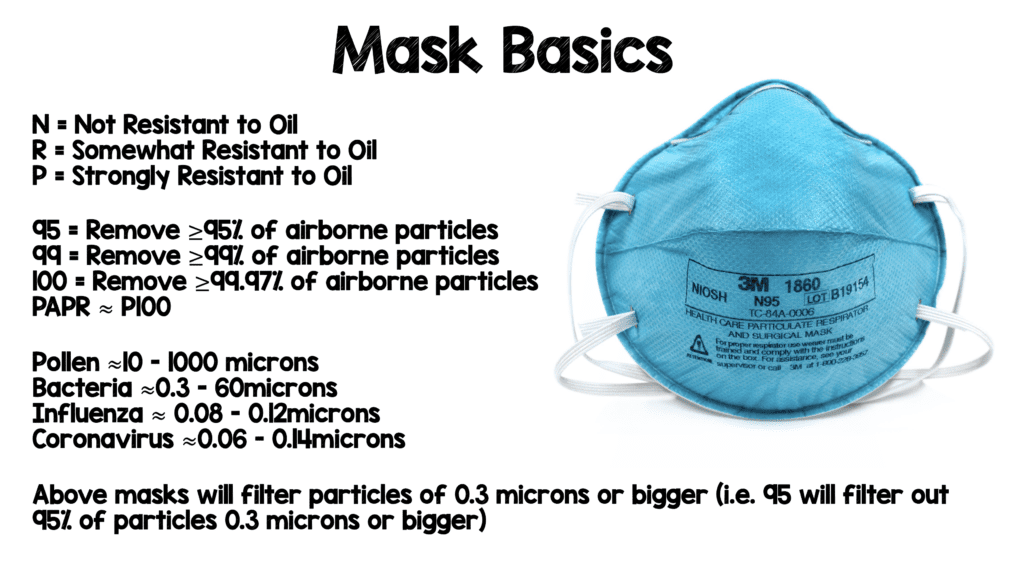
Mask Basics [OSHA Website]
- Letter refers to mask’s resistance to oil:
- N = Not Resistant to Oil
- R = Somewhat Resistant to Oil
- Up to 8hrs or 1 use (whichever comes first)
- P = Strongly Resistant to Oil
- Up to 40hrs or 30d (whichever comes first)
- Number refers to mask’s percentage of airborne particles the filter media will catch:
- 95 = Remove at least 95% of airborne particles
- 99 = Remove at least 99% of airborne particles
- 100 = Remove at least 99.97% of airborne particles
- PAPR similar to P100
- All masks will filter particles of 0.3 microns or bigger (i.e. 95 will filter out 95% of particles 0.3 microns or bigger)
- Important Note: Most viral particles will be contained in droplets (i.e. they will be bigger than their actual size reported below)
For more on different types of masks checkout: Correct the Oversight [Link is HERE]
- Particle Sizes:
- Pollen ≈10 – 1000 microns
- Bacteria ≈0.3 – 60microns
- Influenza ≈ 0.08 – 0.12microns
- Coronavirus ≈0.06 – 0.14microns
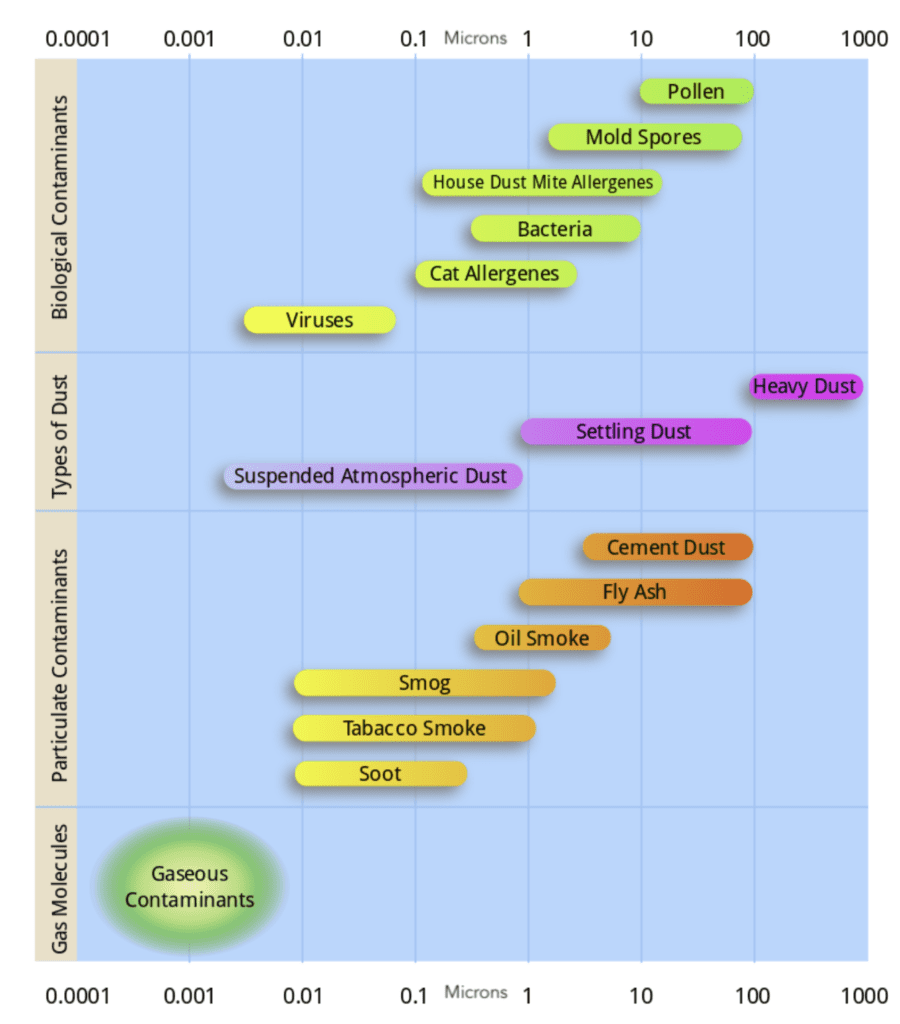
Image from Wikipedia
- In one study [4], particles between 0.08 – 0.2microns (this is the size of coronavirus and influenza) were the most likely range with the lowest protection provided by N95 masks (Important Note: Most viral particles will be contained in droplets meaning they are most likely larger than their actual size)
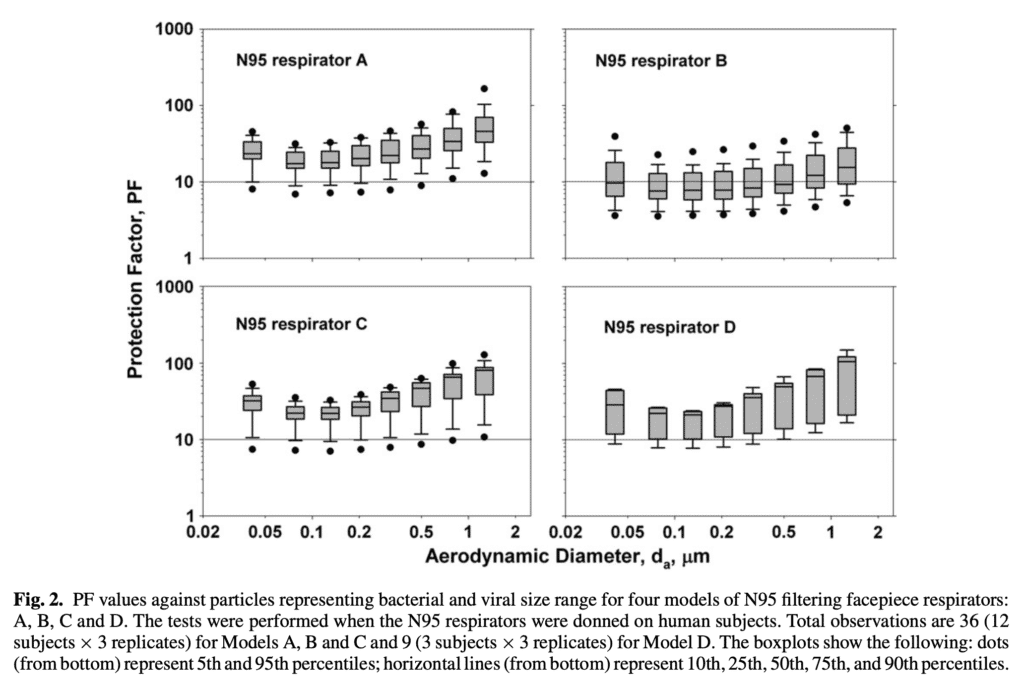
Horizontal line is the OSHA assigned protection factor (10) for 95s
Reusing Masks
- The Institute of Medicine (IOM) projected that a 6-week influenza pandemic would require 90 million face-piece respirators (FFRs)[3]
- The Occupational Safety and Health Administration (OSHA) has predicted that an influenza pandemic would likely last 24 weeks, which suggests that up to 360 million FFRs could be needed in the US alone [3]
- A surge in demand during a pandemic will exceed stockpiles and production capabilities, and would result in shortages of PPE
- Re-use methods SHOULD NOT compromise the respirator’s filtration performance or the ability of the respirator to seal to the wearer’s face as intended
- UV Light [3]
- Ultraviolet germicidal irradiation (UVGI) inactivates microorganisms, primarily by cross-linking thymidine nucleotides in DNA and uracil nucleotides in RNA, which both block replication
- An important consideration for all decontamination methods, including UVGI, is the risk of degradation of respirator material, and will reduce the ability to filter out infectious aerosols
- There is no way of determining the maximum possible number of safe reuses for an N95 respirator as a generic number to be applied in all cases. Safe N95 reuse is affected by a number of variables that impact respirator function and contamination over time. The number of UVGI cycles to which a disposable respirator could be subjected is also a function of the resistance of the respirator to degradation and the UVGI dose used for each cycle
- This study looked to evaluate the effects of UVGI on the filtration performance and structural integrity of four N95 respirators in regard to two aspects:
- Filter penetration = The fraction of aerosol particles that are not removed from the air stream and thus pass through the respirator material
- Flow resistance = The amount of air pressure required for air to flow through the respirator material at a given flow rate
- UVGI doses = 120J/cm2 – 950J/cm2

N95 Masks Evaluated in this Study [3]
-
- Filter penetration increased up to 1.25%, but all N95s had mean penetration values below 5% after maximum exposure levels (basically minimal effect and meets N95 rating)
- Flow resistance was essentially unchanged after UVGI exposure for all respirators
- Bottom Line: UVGI could be used for respirator disinfection, but would need to be implemented cautiously, especially for respirators with a smaller safety margin between the actual penetration value and the 5% maximum allowed for an N95 respirator. It is also unclear what the exact number of times this could be done without losing the integrity of the mask.
- ANYONE REUSING AN N95 MASK OR MAKING ONE:
- Dr. Amanda Deskins, DO contacted Dr. Peter Tsai, MD, the INVENTOR of the filtration fabric in the N95 mask (JAMA Network from March 23rd, 2020) N95 masks are made of polypropylene material and are designed to tightly fit over your face with little leakage around the edge of the mask. She asked Dr. Tsai about reusing the N95 respirator, and what materials could be added in homemade masks to make them more effective. He responded with the following:
- MASK REUSE METHOD #1
- When reusing N95 masks, leave a used respirator in dry, atmosphere air for 3-4 days to dry it out. Polypropylene in N95 masks is hydrophobic and contains zero moisture. COVID-19 needs a host to survive–it can survive on a metal surface for up to 48 hours, on plastic for 72 hours, and on cardboard for 24 hours. When the respirator is dry in 3-4 days, the virus will not have survived.
- Take four N95 masks, and number them (#1-4).
- On day 1, use mask #1, then let it dry it out for 3-4 days.
- On day 2, use mask #2, then let it dry out for 3-4 days.
- Same for day 3, and day 4…
- When reusing N95 masks, leave a used respirator in dry, atmosphere air for 3-4 days to dry it out. Polypropylene in N95 masks is hydrophobic and contains zero moisture. COVID-19 needs a host to survive–it can survive on a metal surface for up to 48 hours, on plastic for 72 hours, and on cardboard for 24 hours. When the respirator is dry in 3-4 days, the virus will not have survived.
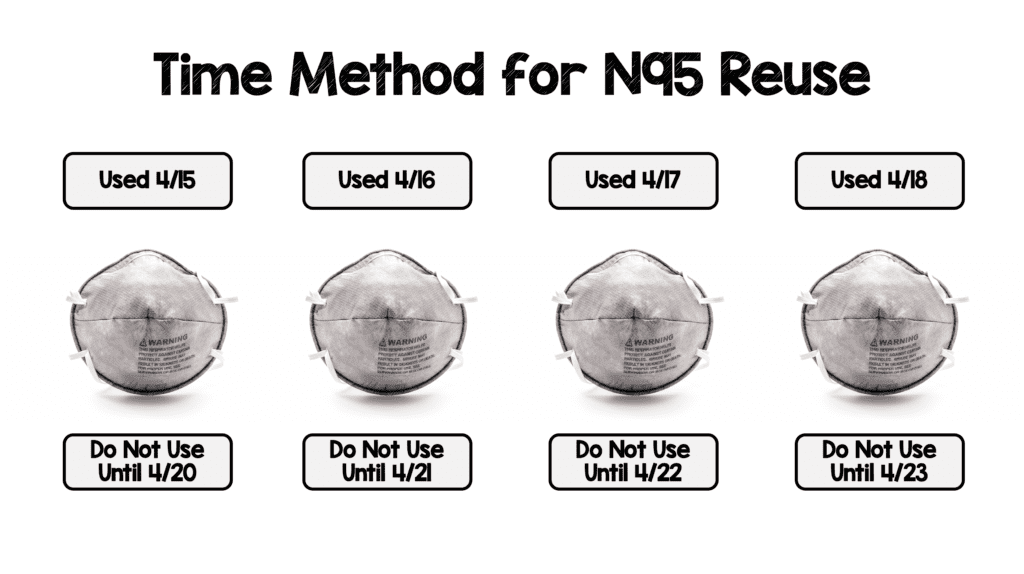
Currently I am using the Time Method for N95 Mask Reuse (Ensure you put two labels with your masks to not confuse last use and when you can use again – Date Used & Do Not Use Until)
-
- MASK REUSE METHOD #2
- You can also sterilize the N95 mask by hanging it in the oven (Not a home oven) without contacting metal at 70C (158F) for 30 minutes—it is reported that COVID-19 cannot survive at 65C (149F) for 30 minutes.
- Use a wood clip to hang the respirator in the kitchen oven to do the sterilization.
- When sterilizing N95 masks, be wary of using UV light–keep N95 masks away from UV light / sunlight. N95 masks are degraded by UV light because it damages the electrostatic charges in the polypropylene material. It is unclear how long the masks can be exposed to UV light before they are ineffective.
- TIPS FOR REUSE METHOD #1 AND METHOD #2
- DO NOT place the respirator on a metal surface, or too close to metal–the temperature on the metal surface is higher than the air temperature.
- Keep N95 masks away from UV light / sunlight.
- When removing the mask, hold the edge of the straps attached to take off the N95 mask. Your hands may be contaminated at this time–don’t touch the inside part of the respirator. Wash your hands with soap for 20 seconds afterward.
- HOMEMADE MASKS
- It is not a good idea to use cotton masks when taking care of infected patients. The effectiveness of a material made of cotton is not high—its fiber is not fine enough, and it cannot be charged. An N95 mask is so thin because it uses Polypropylene which is made of millions of microfibers layered on top of each other that have been permanently electrostatically charged. An electrical field ionizes the air and forces the ions deep into the microfibers which allows the polypropylene to act as a filter.
- However, using a HEPA filter with a face mask might increase its effectiveness, but it may make it harder to breathe. If you place another media over a face mask, the resistance to breathing increases—it is the sum of the two together. When adding an extra layer, make sure it perfectly covers the whole mask. Keep in mind it may make it more difficult to breathe.
- MASK REUSE METHOD #2
- Study out of Stanford shows 70ºC hot air in oven (Not a home oven) for 30 minutes is effective for re-use
- MAJOR CAVEAT: 4C Air confirmed that all proposed treatments have killed coronaviruses, but this data is with E. Coli bacteria and not viral particles
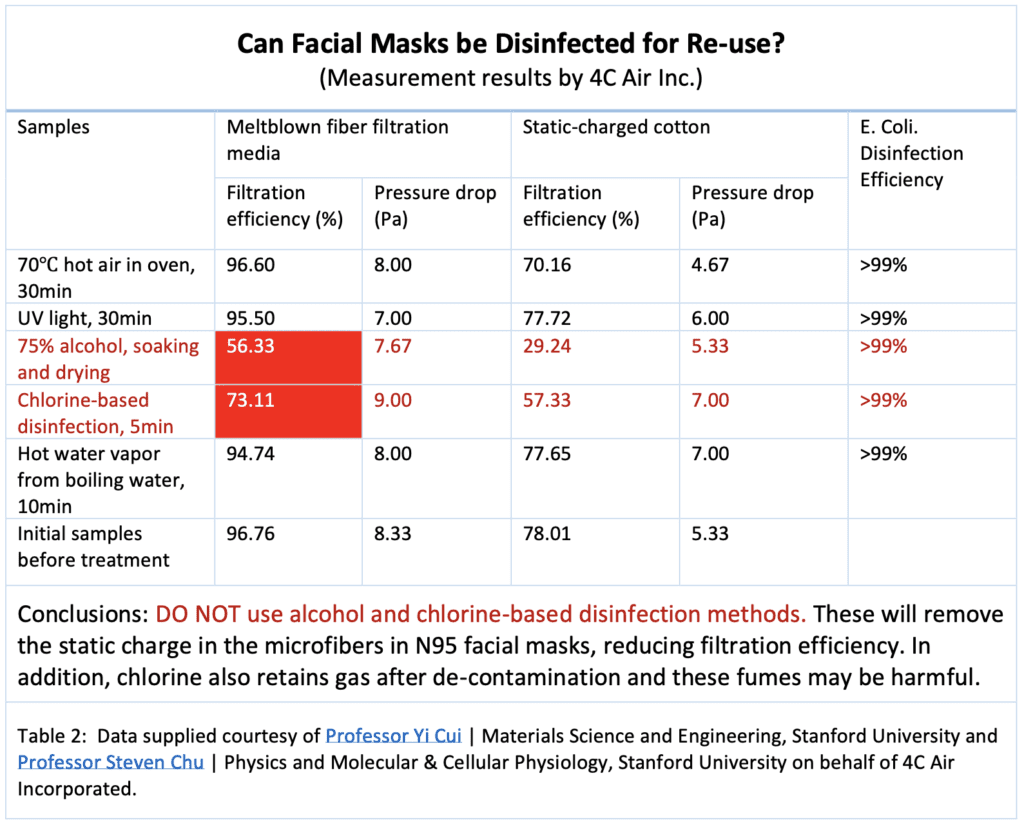
Information from Stanford Medicine Anesthesia Informatics and Media Lab [Link is HERE]
- CDC Decontamination and Reuse of Filtering Facepiece Respirators [Link is HERE]
- Vaporous Hydrogen Peroxide (VHP): Passed filtration performance & fit unaffected for up to 20 cycles
- Ultraviolet Germicidal Irradiation (UVGI): 0.5 – 950J/cm2 Passed filtration performance & 90 – 100% fit unaffected for up to 3 cycles
- Microwave Generated Steam: 1100 – 1250W (40sec to 2 min) Passed filtration performance for 1 to 20 cycles & 95 – 100% pass fit unaffected after 3 to 20 cycles
- Moist Heat Incubation: 15 – 30min (60C) Passed filtration performance after 3 cycles & fit unaffected
Is N95 Extended Use and Reuse a Safe Practice? [8] (Added June 7th, 2020)
- CDC recommends extended use and limited reuse during PPE shortages, but both reuse and extended use policies are based off no robust evidence about efficacy and safety
- N95 Extended Use = Wearing the same N95 for multiple patient encounters
- N95 Limited Reuse = Storing an N95 between encounters for use over multiple encounters
- Question: What is the prevalence of N95 fit test failure with extended use and limited reuse of N95 masks?
- Observational cross-sectional study at a single center in the US
- Convenience sample of health care workers when researchers present
- All participants passed an OSHA mandated N95 fit test within the last 1 to 2 years
- Qualitative fit test done with bitter testing solution on two masks:
- Dome shaped (3M 1860)
- Duckbill (Kimberly-Clark 467272 or Halyard 46867)
- If participants could taste solution, they failed the fit test and fitted with a new N95 test
- Primary Outcome: N95 fit test failure
- Results:
- 68 participants
- Dome shaped N95s used by 75.0%
- Overall, 38.2% failed the fit test
- Duckbill masks, 12/17 (70.6%) failed fit test
- Dome shaped masks, 14/51 (27.5%) failed fit test
- For dome shaped masks, fit test failure associated with increased number of shifts worn (median 4 shifts), increased donning/doffing (median 15), and increased hours worn (14)
- Discussion:
- Duckbill N95s had a high failure rate compared to dome shaped masks and should be limited if alternatives available
- Duration of wear and number of donnings/doffings were self-reported and may not be precise or accurate estimates
- Precise time of failure was not measured
- Confounding (mask quality, characteristics of wearer)
- Failed fit tests may not result in increased rates of infection
- This pub has gotten lots of traction, but some serious issues that make it difficult to interpret results
- Fit test done 1 – 2 years prior (we don’t know how masks fit right before start of study)
- Convenience sample could lead to selection bias (i.e. how were participants selected?)
- No info on characteristics of wearer (facial hair, appropriate initial fit, etc.)
- Failed fit test ≠ increased rate of infection
- Study produces more questions than answers
Stumbled on this video on Facebook and thought it would be worth sharing here. pic.twitter.com/spITZlE7Cq
— DrKKWate (@ChristianAssad) March 31, 2020
- Make your own N95 (It’s sad, but this is what it has come to…Macgyvering N95s for our safety)
- Option 1:
- Anesthesia Mask
- Ventilator Inline Bacterial Viral/Filter
- 2 Elastric Straps from Nebulizer Mask
- Option 1:
[embedyt] https://www.youtube.com/watch?v=Es_iY5WJdmI[/embedyt]
AAEM Position Statement on Use of Self-Supplied PPE [Quoted from Site]
“AAEM believes that emergency physicians are entitled to wear self-supplied PPE including respirators that meet NIOSH standards when, in their medical opinion, hospital or healthcare facility supplied PPE is inadequate.
AAEM will offer support to any emergency physician threatened or terminated for attempting to protect themselves and their patients in this manner. This includes assistance with filing an OSHA complaint and pursuit of litigation for wrongful termination.
AAEM believes that until sufficient evidence exists regarding the safety of such, it is improper to downgrade the level of PPE recommended due to supply chain issues.
AAEM supports other frontline healthcare workers in obtaining and using self-supplied PPE as well.”
ACEP COVID-19 Position Statement on the Use of Donated or Self-Purchased PPE [Quoted from Site]
“Approved March 25, 2020
Global penetrance of COVID-19 has placed significant stress on the ability to produce and supply appropriate PPE to health care workers. Additionally, the risk pool of known and unknown disease in our communities has greatly challenged our ability to reliably determine patients who are at low risk. For these reasons, ACEP has and will continue to support the use of surgical masks with proper eyewear and other protective equipment for all patients. Processes and procedures that create higher risk, such as close contact and aerosolizing procedures, require full PPE, including N95s.
Because the inadequate PPE supply increases the risk to our physicians, they have taken to buying their own PPE or utilizing donations from other industries. ACEP urges hospitals and other health care facilities to allow physicians to use their donated or self-purchased PPE.”
Joint Commission Position Statement on the Use of Self-Purchased PPE [Quoted from Site]
“The Joint Commission supports allowing staff to bring their own masks or respirators to wear at work when their healthcare organizations cannot provide them with adequate protection commensurate with the risk of infection to which they are exposed by the nature of their work. Allowing staff to wear masks (or respirators, depending on the degree of risk) throughout the day should help prevent nosocomial spread, although the evidence supporting this is incomplete. At the same time, we strongly support healthcare organizations’ efforts to conserve PPE and to distribute scarce supplies according to CDC recommendations. Most importantly, hospitals must conserve N95 respirators as much as possible to protect staff who perform high risk procedures that aerosolize viral particles (e.g., bronchoscopy, intubation).”
Personal Protective Equipment (PPE) for Healthcare Workers Dealing with Suspected or Confirmed Cases:
- Gown, gloves, and either an N95 respirator plus a face shield/goggles or a powered, air-purifying respirator (PAPR) for any aerosolizing procedures (i.e. NEBs, NIV, HFNC, Intubation, etc…)
- For Pre-Hospital EMS (My Recs):
- Respiratory complaints: Surgical mask, eye protection, gown, and gloves
- Aerosol producing procedures: Change surgical mask for N95/PAPR
- DON = Contraction for “do (put) on”
- DOFF = Contraction for “do (take) off”
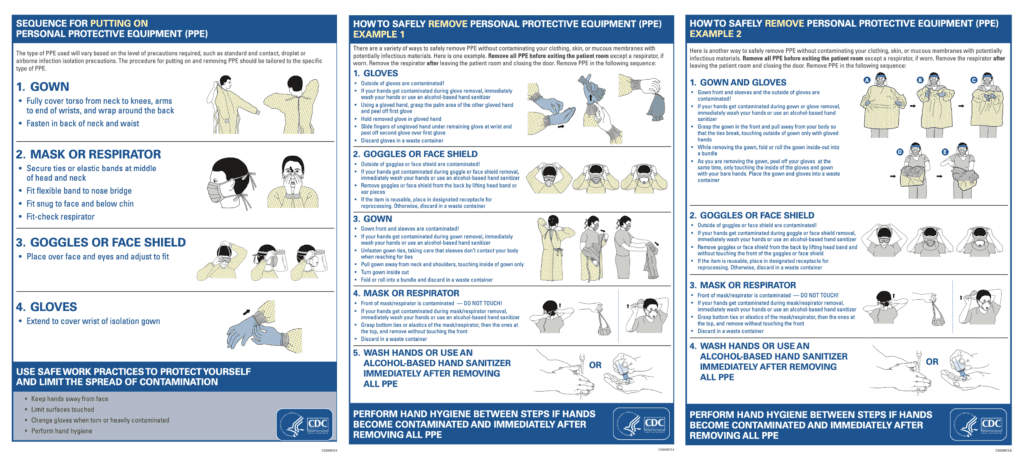
From the CDC Website
[embedyt] https://www.youtube.com/watch?v=bG6zISnenPg[/embedyt]
Donning (at 5:05min) and Doffing (at 11:11min) Video
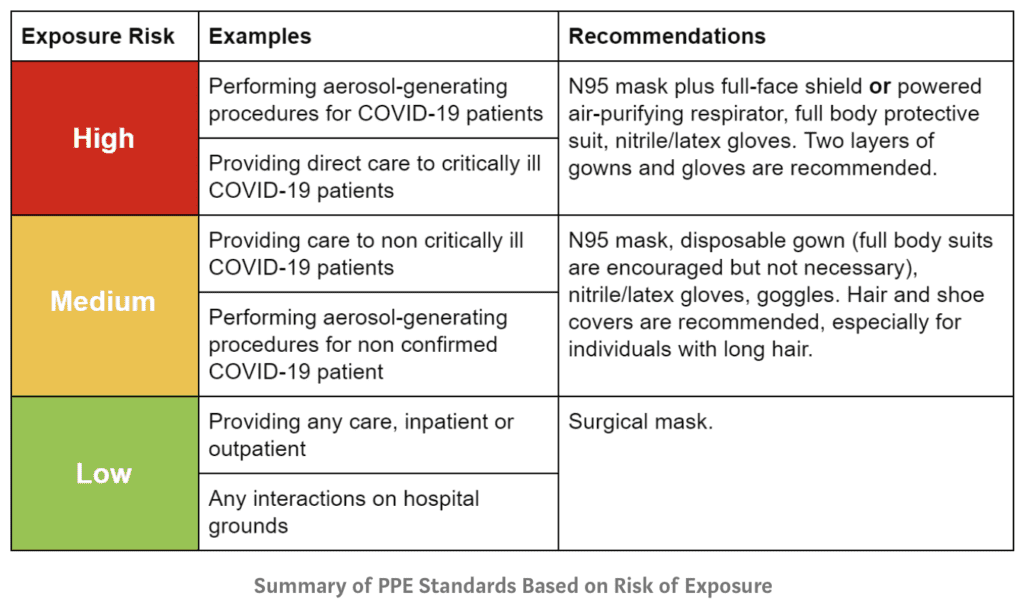
Tailored Standards of PPE Based on Exposure Risk [Link is HERE]
References:
- Holbrook MG et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. NEJM 2020. [Epub Ahead of Print]
- Kelkar U et al. How Effective are Face Masks in Operation Theatre? A Time Fram Analysis and Recommendations. International Journal of Infection Control 2013. [Link is HERE]
- Lindsley WG et al. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. J Occup Environ Hyg 2016. PMID: 25806411
- Lee SA et al. Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation with NaCl Aerosol Representing Bacterial and Viral Particle Size Range. Oxford Academic 2008 [Link is HERE]
- MacIntyre CR et al. A Cluster Randomised Trial of Cloth Masks Compared with Medical Masks in Healthcare Workers. BMJ Open 2015. PMID: 25903751
- Kampf G et al. Persistence of Coronaviruses on inanimate Surfaces and Their Inactivation with Biocidal Agents. J Hosp Infect 2020. PMID: 32035997
- Wilson NM et al. Airborne Transmission of Severe Acute Respiratory Syndrome Coronavirus-2 to Healthcare Workers: A Narrative Review. Anaesthesia 2020. PMID: 32311771
- Degesys NF et al. Correlation Between N95 Extended Use and Reuse and Fit Failure in an Emergency Department. JAMA 2020. PMID: 32496504
For More Thoughts on This Topic Checkout:
- REBEL EM: COVID-19 – The Novel Coronavirus 2019
- Medium: Coronavirus – Why You Must Act Now
- The New Yorker: Keeping the Coronavirus From Infecting Health-Care Workers
- FOAMCast: COVID19 – SARS-CoV-2 Transmission and Masks
- emDocs: Personal Protective Equipment (PPE) Pearls – COVID-19
- EMCases: COVID-19 Part 3 – PPE – What We Know, Conservation Strategies and Protected Code Blue
- St. Emlyn’s: The #COVID19 Safety Bubble
- DFTB: Aerosol Generating Procedures
- First10EM: Aerosols, Droplets, and Airborne Spread: Everything You Could Possibly Want to Know
- First10EM: Aerosol Generating Procedures
- First10EM: Aerosol and Surface Distribution of SARS-CoV-2 (COVID-19)
- REBEL EM: N95 Mask Decontamination and Reuse
- First10EM: Droplets Spread More than 2 Meters (A Systematic Review)
- First10EM: Can We Safely Reuse N95 Masks?
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Mizuho Morrison, DO (Twitter: mizuhomorrison)