 Patients with corneal abrasions typically come to the emergency department for eye pain. Most physicians treat these with topical antibiotics, oral analgesia, and for those who are lucky enough 48 – 72 hour follow up with ophthalmology. Oral analgesia does a poor job of controlling these patients pain. Tetracaine is an esterase type anesthetic with a onset of action of 10 – 20 seconds and a duration of action of 10 – 15 minutes. Use of topical anesthetics are very effective at reducing pain, but there use is discouraged secondary to poor wound healing of the corneal epithelium. So what is the evidence for topical anesthetic use on corneal abrasions?
Patients with corneal abrasions typically come to the emergency department for eye pain. Most physicians treat these with topical antibiotics, oral analgesia, and for those who are lucky enough 48 – 72 hour follow up with ophthalmology. Oral analgesia does a poor job of controlling these patients pain. Tetracaine is an esterase type anesthetic with a onset of action of 10 – 20 seconds and a duration of action of 10 – 15 minutes. Use of topical anesthetics are very effective at reducing pain, but there use is discouraged secondary to poor wound healing of the corneal epithelium. So what is the evidence for topical anesthetic use on corneal abrasions?
Where does the evidence for NO topical anesthetic use on corneal abrasions come from?
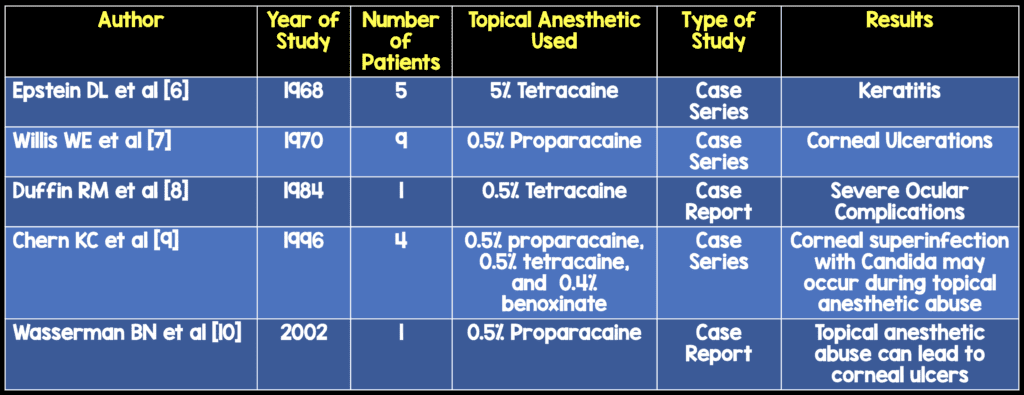
 The evidence for the toxic effects of topical anesthetics comes from case reports, case series, and animal studies. The case reports and series are listed above, and in all but one of the cases the patients were abusing topical anesthetics for weeks to months and/or concentrations higher than that typically used today. So the statements that topical anesthetics have toxic effects to the cornea and decrease or inhibit corneal reepithelialization come from patients abusing these medications and not using them for short periods of time.
The evidence for the toxic effects of topical anesthetics comes from case reports, case series, and animal studies. The case reports and series are listed above, and in all but one of the cases the patients were abusing topical anesthetics for weeks to months and/or concentrations higher than that typically used today. So the statements that topical anesthetics have toxic effects to the cornea and decrease or inhibit corneal reepithelialization come from patients abusing these medications and not using them for short periods of time.
Two animal studies [1] and [2] were examining toxicity of topical anesthetics. Topical anesthetics were being used at increasing concentrations until corneal epithelial damage was seen. Both studies were from the corneas of rabbits who have a more sensitive cornea and a reduced blinking rate when compared to humans, therefore it is hard to draw generalizations to humans.
What trials have evaluated the use of topical anesthetics on corneal abrasions?
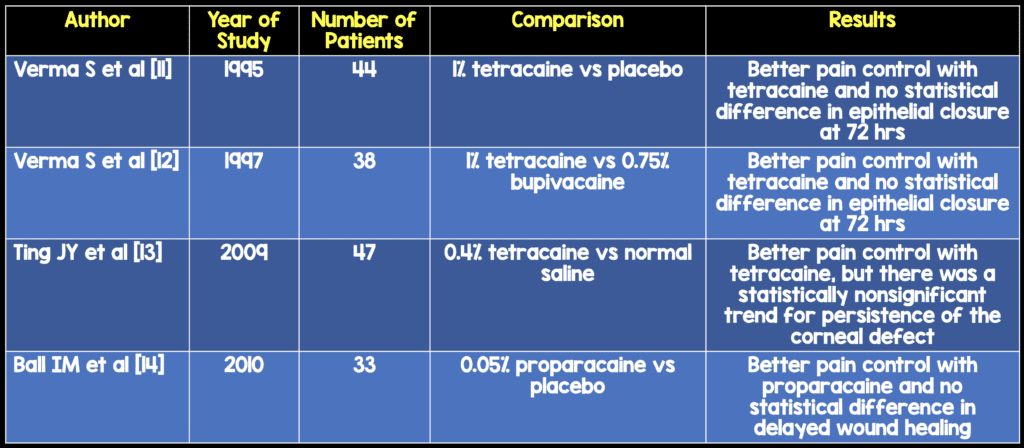
Conclusion: Topical anesthetics did a better job of controlling pain and in all but one of the studies no statistical difference in cornea epithelial healing at 72 hours.
What is the most recent trial to evaluate topical anesthetic use on corneal abrasions? [3]
What they did:
- Prospective, double-blind, randomized trial of a convenience sample of 116 patients with uncomplicated corneal abrasions
- 1% tetracaine vs saline q30 minutes prn pain for 24 hours
- Largest RCT evaluating safety of topical anesthetics with uncomplicated corneal abrasions
Exclusion Criteria:
- > 36 hours after initial injury
- < 18 years of age
- Wear contact lenses
- Injury to both eyes
- Grossly contaminated foreign body in eye
- Current herpes keratitis
- Allergy to tetracaine
- Injury requiring urgent optho evaluation
- Unable to make follow up at 48 hours
Main Safety Outcomes:
- Complications specifically attributed to topical anesthetic defined as:
- Delayed healing
- Enlarged abrasion
- Recurrent corneal ulceration
- Toxic keratitis
- surface keratopathy
- Corneal stromal infiltration
- Candida and bacterial keratitis
- Uveitis
- Hypopyon
- Persistent fluorescein uptake at 48 hours for corneal evaluation
- 1 week and 1 month telephone interviews
- Every patient had at least one follow up evaluation
Secondary Outcomes
- Pain control with a 100-mm visual analog scale (VAS)
- Overall effectiveness with a numeric rating scale (NRS) of 0 – 10
Results:
- No complications attributed to topical anesthetic (CI of 0 – 6.1%), but this is a wide CI
- No statistically significant difference in corneal healing at 48 hours (23.9% vs 21.3% with p value of 0.761)
- Retained rust ring in 23 patients: tetracaine 22.0% vs saline 17.5% (p value = 0.544)
- Fluorescein uptake at 48 hours: tetracaine 23.9% vs saline 21.3% (p value = 0.761)
- No persistent symptoms at 48 hours (21.7% vs 21.3% with p value of 0.957)
- No difference in VAS pain scores at any time between groups
- Patients rated tetracaine having a better overall effectiveness on the NRS (7.7 vs 3.9)
Limitations:
- Excluded penetrating eye injuries, large or complicated corneal abrasions, and injuries causing a significant disruption of vision
- Some patients discovered when using the tetracaine drops they experienced burning similar to the tetracaine they were treated with in the ED which may have unblinded the patient and researcher
- Patient compliance with administering the tetracaine or saline was not recorded
- The study was under powered to detect a difference in the efficacy between the two groups
- There was poor follow up at 48 hours: Tetracaine group 69.0% vs Saline Group 64%
Conclusion: Topical tetracaine used for 24 hours was safe, patients felt they had a significantly higher overall effectiveness with tetracaine, but no significant difference in the VAS pain score.

There was a commentary to this study [4] in which the author states: “Many common practices are driven by dogma, untested conventional wisdom, and opinions of both actual and self-promoted experts. Working with residents and students on a day-to-day basis is often the only thing that slows down busy clinicians long enough to consider the lack of evidence supporting many common practices.” He goes on to say that “ED physicians have been taught that topical anesthetic use is associated with poor healing, but this teaching is grounded in laboratory-based studies and case reports that describe prolonged, unsupervised use (or abuse) of topical anesthetics.” He finishes up by saying, “Whether or not to start using tetracaine routinely in the treatment of simple corneal abrasions remains up to the reader.”
How Your Pharmacist can Make a 1:10 (0.05%) Dilution From 0.5% Anesthetic
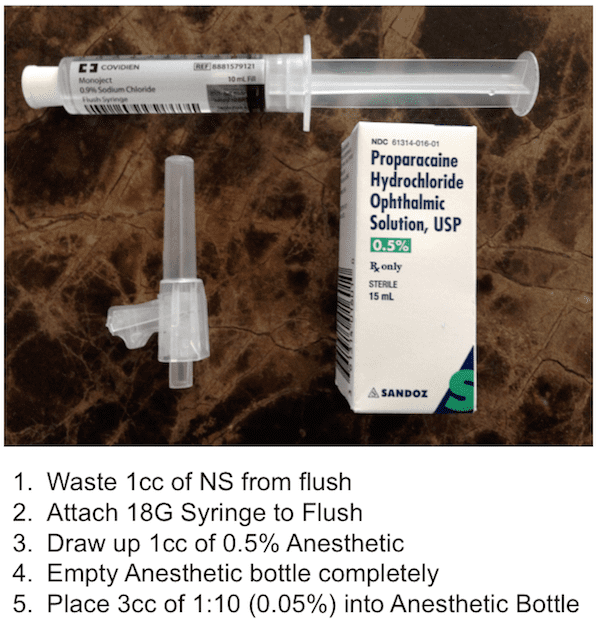

The inpatient pharmacy team should label the bottle with the following instructions for the patient:
Proparacaine 0.05% Ophthalmic
1 – 2 drops in affected eye q30 min prn pain
Disp: 2 – 3 mL
Lot#: Date of Disp:
**Not to exceed 24 – 48 hours of use
Take Home Message:
To date the only evidence that topical anesthetics in uncomplicated corneal abrasions causing more harm come from experimental animal studies, case reports, and case series. Based on available evidence, it is most likely reasonable to send patients home with dilute topical anesthetics for a period of no more than 24 – 48 hours without patients having complications, but larger studies will need to occur before this recommendation is officially made.
References:
- Bisla K et al. Concentration-Dependent Effects of Lidocaine on Cornal Epithelial Wound Healing. Invest Ophthalmol Vis Sci 1992. PMID: 1399407
- Maurice DM et al. the Absence of Corneal Toxicity with Low-Level Topical Anesthesia. Am J Ophthalmol 1985. PMID: 2409803
- Waldman N et al. Topical Tetracaine Used for 24 Hours is Safe and Rated Highly Effective by Patients for the Treatment of Pain Caused by Corneal Abrasions: A Double-Blind, Randomized Clinical Trial. Acad Emerg Med 2014. PMID: 24730399
- Ufberg JW. Dogma Challenged: Tetracaine for corneal Abrasions? Acad Emerg Med 2014. PMID: 24730412
- Waldman N et al. An Observational Study to Determine Whether Routinely Sending Patients Home With a 24-Hour Supply of Topical Tetracaine From the Emergency Department for Simple Corneal Abrasion Pain is Potentially Safe. Ann Emerg Med 2017; S0196 – 0644(17): 30195 – 6. PMID: 28483289
- Epstein DL et al. Keratitis From Misuse of Corneal Anesthetics. NEJM 1968. PMID: 4232838
- Willis WE et al. Corneal Complications of Topical Anesthetic Abuse. Can J Opthalmol 1970. PMID: 5472832
- Duffin RM et al. Tetracaine Toxicity. Ann Ophthalmol 1984. PMID: 6508100
- Chern KC et al. Corneal Anesthetic Abuse and Candida Keratitis. Ophthalmology 1996. PMID: 8628558
- Wasserman BN et al. Recurrent Corneal Ulceration as Late Complication of Toxic Keratitis. Br J Ophthalmol 2002. PMID: 11815357
- Verma S et al. A Prospective, Randomized, Double-Masked Trial to Evaluate the Role of Topical Anesthetics in Controlling Pain After Photorefractive Keratectomy. Ophthalmology 1995. PMID: 9098296
- Verma S et al. A Comparative Study of the Duration and Efficacy of Tetracaine 1% and Bupivacaine 0.75% in Controlling Pain Following Photorefractive Keratectomy (PRK). Our J Ophthalmol 1997. PMID: 9457454
- Ting JY et al. Management of Ocular Trauma in Emergency (MOTE) Trial: A Pilot Randomized Double-Blinded Trial Comparing Topical Amethocaine with Saline in the Outpatient Management of Corneal Trauma. J Emerg Trauma Shock 2009. PMID: 19561949
- Ball IM et al. Dilute Proparacaine for the Management of Acute Corneal Injuries in the Emergency Department. CJEM 2010. PMID: 20880433
For More on This Topic Checkout:
- The SGEM: Episode #83 – In Your Eyes (Topical Tetracaine for Corneal Abrasions)
- Swaminathan A et al. The Safety of Topical Anesthetics in the Treatment of Corneal Abrasions: A Review. J Emerg Med 2015 [epub ahead of print] PMID: 26281814
- Puls HA et al. Safety and Effectiveness of Topical Anesthetics in Corneal Abrasions: Systematic Review and Meta-Analysis. J Emerg Med 2015 [epub ahead of print]
- The SGEM: Episode #145 – Topical Anesthetics for ED Patients with Corneal Abrasions
- EM Lit of Note: Counterpoint – Topical Anesthetics for Corneal AbrasionsCounterpoint – Topical Anesthetics for Corneal Abrasions
- The SGEM: Episode #315: Comfortably Numb with Topical Tetracaine for Corneal Abrasions



