 Acute severe asthma, formerly called status asthmaticus, is defined as severe asthma unresponsive to repeated courses of beta-agonist therapy or subcutaneous epinephrine. It is a medical emergency that requires immediate recognition and treatment. Recently, Anand Swaminathan (Twitter: @EMSwami) gave a lecture to the residents at the University of Texas Health Science Center at San Antonio (UTHSCSA) February 2015. This post is a summary of that lecture on how to manage the crashing asthmatic.
Acute severe asthma, formerly called status asthmaticus, is defined as severe asthma unresponsive to repeated courses of beta-agonist therapy or subcutaneous epinephrine. It is a medical emergency that requires immediate recognition and treatment. Recently, Anand Swaminathan (Twitter: @EMSwami) gave a lecture to the residents at the University of Texas Health Science Center at San Antonio (UTHSCSA) February 2015. This post is a summary of that lecture on how to manage the crashing asthmatic.
REBEL Cast Episode 11: Management of the Crashing Asthmatic
Click here for Direct Download of Podcast
Case: 45 year old male with known past medical history of asthma comes to ED via EMS with chief complaint of difficulty breathing.
Vital Signs: BP 80/57 HR 146 RR 45 O2Sat 91% on room air
EMS has already provided: Beta agonist therapy, Oxygen therapy, and IVF
Summary of Heroic Medical Measures in the Crashing Asthmatic
- The initial management in the crashing asthmatic should be breathing, circulation, airway not airway, breathing circulation (i.e. “BCA” not “ABC”). We want to try and avoid intubation if we can. Intubation of asthmatic patients was historically associated with increased morbidity/mortality.
- Pre-oxygenate your patient with high flow nasal cannula at 20 – 30 LPM [PMID: 22050948].
- I have also written about this on REBEL EM — Preoxygenation and Apneic Oxygenation
 Next consider using IM Epinephrine 0.3 – 0.5mg of 1:1000 [PMID: 3354935]. Severe asthmatics will have a hard time getting inhaled beta agonists into the small airways, but parenteral epinephrine will get into the circulation and get to where it needs to provide support.
Next consider using IM Epinephrine 0.3 – 0.5mg of 1:1000 [PMID: 3354935]. Severe asthmatics will have a hard time getting inhaled beta agonists into the small airways, but parenteral epinephrine will get into the circulation and get to where it needs to provide support.- Non-Invasive Positive Pressure Ventilation (NIPPV) can help decrease work of breathing and help push beta agonist into the smaller airways [PMID: 12684289][PMID: 7486361].
- Corticosteroids main effect is to help reduce inflammation, but these effects won’t be seen until 4 – 6 hours later. It is important however to give corticosteroids early because this helps up regulate the beta receptors in the lungs at about an hour after giving the medication.
- Give IV magnesium sulfate for its bronchodilator effect, but don’t just give 2g IV x1. Instead give 2g IV and repeat it upto 2 more times over an hour [PMID: 7781349] [PMID: 24731521].
- Give IVF at a dose of 30cc/kg because patients with acute asthma exacerbations because patients will have insensible losses. Also if you are going to intubate patients with asthma, once they are intubated due to the positive pressure ventilation they will have a decrease in preload and IVF will help maximize preload.
 Sub-dissociative dose IV Ketamine (0.1 mg/kg followed by IV infusion of .5 mg/kg/hour for 3 hours) may be helpful to facilitate use of BiPAP in a hypoxic/combative patient [PMID: 8629747]. If you have gotten to this step you should start setting up for intubation at this point in case the patient continues to deteriorate.
Sub-dissociative dose IV Ketamine (0.1 mg/kg followed by IV infusion of .5 mg/kg/hour for 3 hours) may be helpful to facilitate use of BiPAP in a hypoxic/combative patient [PMID: 8629747]. If you have gotten to this step you should start setting up for intubation at this point in case the patient continues to deteriorate.
- ADDENDUM 10/12/2020 –> New RCT advocates for 0.4mg/kg bolus which gives optimal bronchodilation [PMID: 30009223]
- Delayed Sequence Intubation is a procedural sedation to help facilitate pre-oxygenation. [PMID: 25447559].
- EMCrit — Delayed Sequence Intubation (DSI)
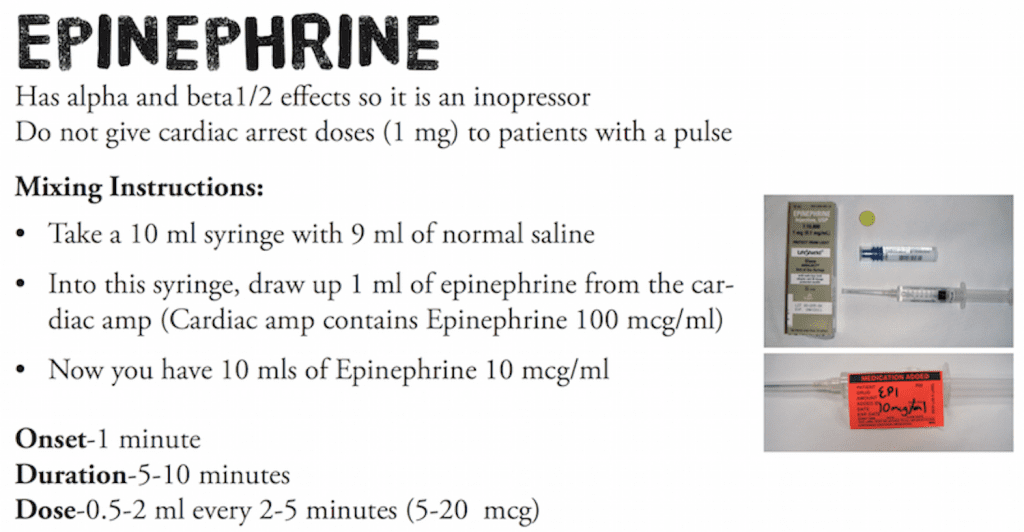
- Intravenous epinephrine can be considered as well. In hypotensive patients, it is possible that the IM epinephrine is just not circulating [PMID: 12712039] [PMID: 16713785]. REMEMBER we want to use the 1:10,000 concentration here and even think about push dose epinephrine.
- EMCrit Podcast 6 – Push Dose Pressors
Summary of Intubation in the Crashing Asthmatic
- Don’t forget NO DESAT (Nasal Oxygen During Efforts Securing A Tube). This will buy you a longer apneic period while trying to intubate.
 Ketamine 1 – 2 mg/kg IV is the ideal induction agent due to its bronchodilatory effects. Remember you already used a sub-dissociative dose in your medical management so why change to a different agent.
Ketamine 1 – 2 mg/kg IV is the ideal induction agent due to its bronchodilatory effects. Remember you already used a sub-dissociative dose in your medical management so why change to a different agent.- Rocuronium 1.2 mg/kg IV is the ideal paralytic agent as it will keep the patient paralyzed close to 90 minutes which can help with ventilator management.
Summary of Ventilation Management in the Crashing Asthmatic
- Permissive Hypercapnia allows for CO2 to rise and pH to drop in order to avoid auto-peep and barotrauma.
- Respiratory Rate of 6 – 8 breaths/min
- Tidal Volume of 6cc/kg of IDEAL BODY WEIGHT
- Peak Flow 90 – 120 L/min
- All of the above increases the expiratory time to allow patients to not auto-peep
- If still having issues be sure to trouble shoot the ventilator.
- Remember Peak Pressure is the maximum amount of pressure sensed by the ventilator in the ventilator circuit and doesn’t reflect what is going on in the lungs
- We care about Plateau Pressure which is the pressure in the lower airways. Shoot for a Plateau Pressure of <30 mmHg. (If you hit the expiratory pause button on the ventilator, this will give you the plateau pressure)
- Ventilator Asynchrony occurs due to patients being tachypneic and breathing against the ventilator and start to breath stack and develop more auto-peep. The solution for this is to keep the patient paralyzed and appropriately sedated. (Remember these patients are on high doses of steroids and critical care myopathy and long term paralysis is a real thing, so don’t keep them paralyzed for more than 2 – 3 hours).
- If Plateau pressures are still running high you can consider a couple other things as final ditch efforts:
- Inhalational Anesthetics by anesthesiology in the operating room due to their bronchodilatory effects [PMID: 25662208]
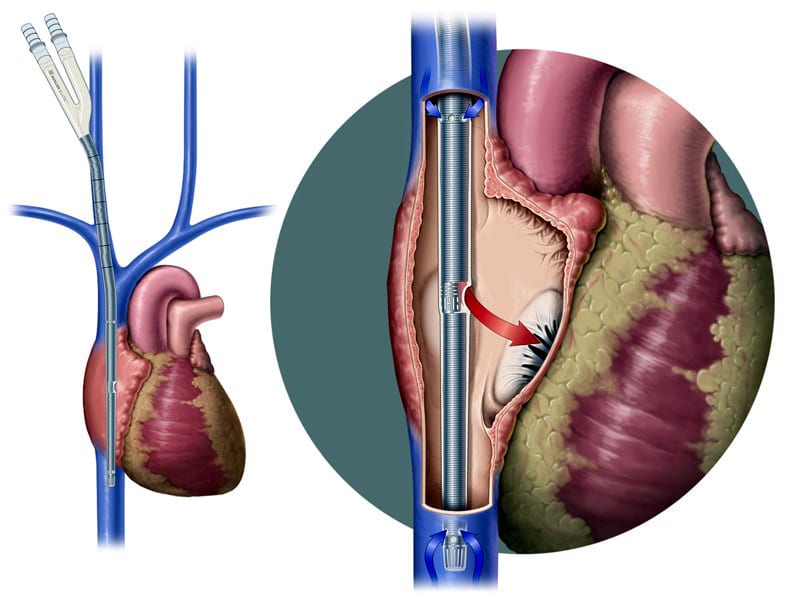 V-V ECMO will help get oxygen into the bloodstream (Checkout edecmo.org)
V-V ECMO will help get oxygen into the bloodstream (Checkout edecmo.org)
- If the patient is having hemodynamic instability, 1st disconnect them from the ventilator (removes equipment failure from the equation) and forcefully exhale the patient by pushing down on their chest softly (this can take 20 – 30 seconds), finally think about the DOPES mnemonic:
- Displacement of endotracheal tube
- Obstruction of endotracheal tube
- Pneumothorax
- Equipment Failure
- Stacked Breaths



