 A 52 year old female with a past medical history of type II diabetes mellitus and tobacco abuse presents with a chief complaint of chest pain.
A 52 year old female with a past medical history of type II diabetes mellitus and tobacco abuse presents with a chief complaint of chest pain.
According to the patient she had about 2 – 3 months of stuttering, substernal chest pain without any radiation. She described the pain as pressure-like, with activity, but that it would typically resolve after a few minutes of rest. Today she awoke with substernal chest pain that never resolved and continued in the emergency department. She quantifies her pain as 7/10 and not relieved with 2L nasal cannula of oxygen, 325mg PO aspirin, and SL NTG x3.
BP 127/89 HR 76 RR 20 O2 sat 100% on 2L NC Temp 99.3
Awake, A&Ox3, appears uncomfortable
Mild JVD on examination
RRR w/o m/r/g
CTA B
2+ pulses in her extremities, no edema
ECG is shown (No prior ECG for comparison)…..
Before reading on, try to come up with your own interpretation of this ECG before moving on to the final impression
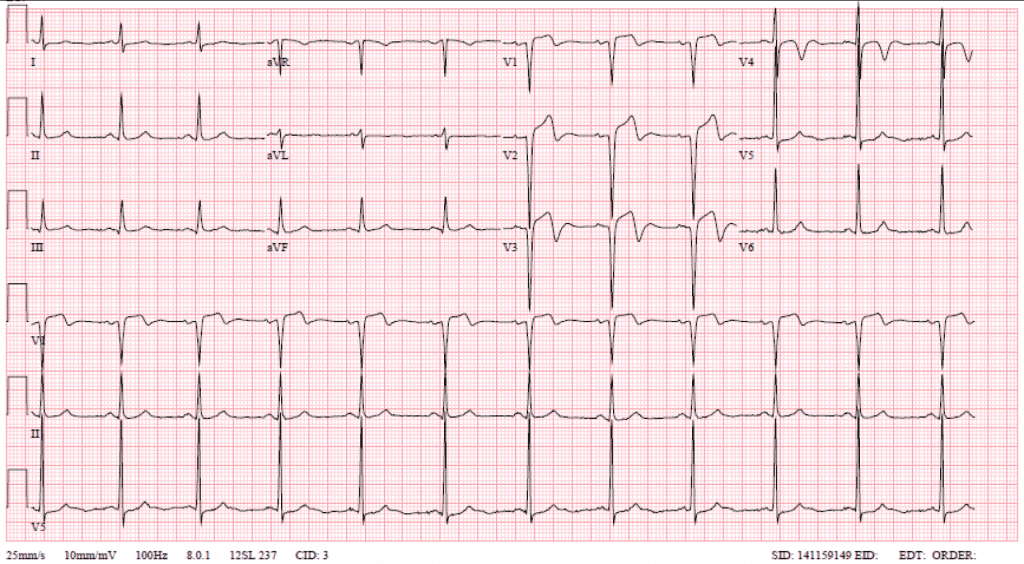
Rate: 68
Rhythm: Normal Sinus Rhythm
Axis: Normal Axis
QRS: Left Ventricular Hypertrophy
ST/T Waves: Biphasic T- Waves in Leads V1 – V4, but there is also ST Elevation in Leads V1 – V3
Final ECG Interpretation: Anterior STEMI
Although this is a case of Anterior STEMI, lets discuss Wellens’ Syndrome….
History of Wellens’ Syndrome
Wellens’ Syndrome was first described in 1982 [1] in which 75% of patients with t-wave inversions in V2 – V4 went on to have an acute myocardial infarction. This was again discussed in 1989 [2], and showed that all patients with this morphology had a > 50% LAD stenosis. In the United States, 10 – 15% of unstable angina patients admitted will have this ECG finding.
What is Wellens’ Syndrome?
- History of Angina
- ECG Changes (T-wave Inversions/Biphasic T-waves in leads V2 – V4)
- Normal to Minimally elevated Cardiac Enzymes
- No pathologic precordial q waves
- No loss of precordial R wave progression
What are the Types of Wellens’ Syndrome?
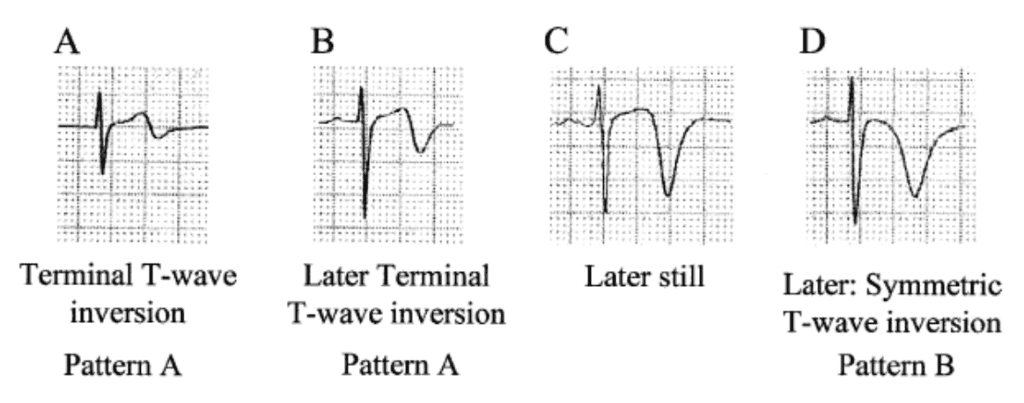
Image from Smith SW et al. Emerg Med Clin N Am 2006 [PMID: 16308113]
Why does Wellen’s Syndrome Matter? [3]
- Signifies a critical high grade proximal LAD stenosis
- Myocardial infarction occurs within a mean of 6 – 8.5 days after admission
- Myocardial infarction occurs within a mean of 21.4 days after symptoms
What is the Specificity of inverted T waves (V1 – V4) on EKG for proximal LAD stenosis?
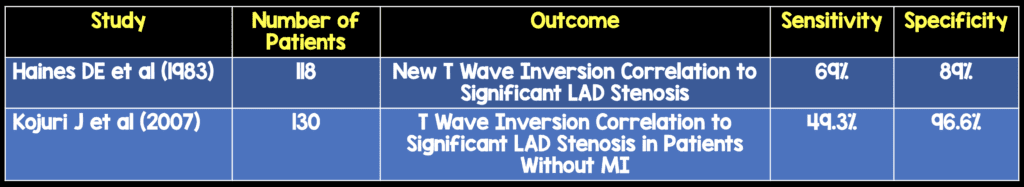
Remember: T-wave changes may be transient or resolve with medical management
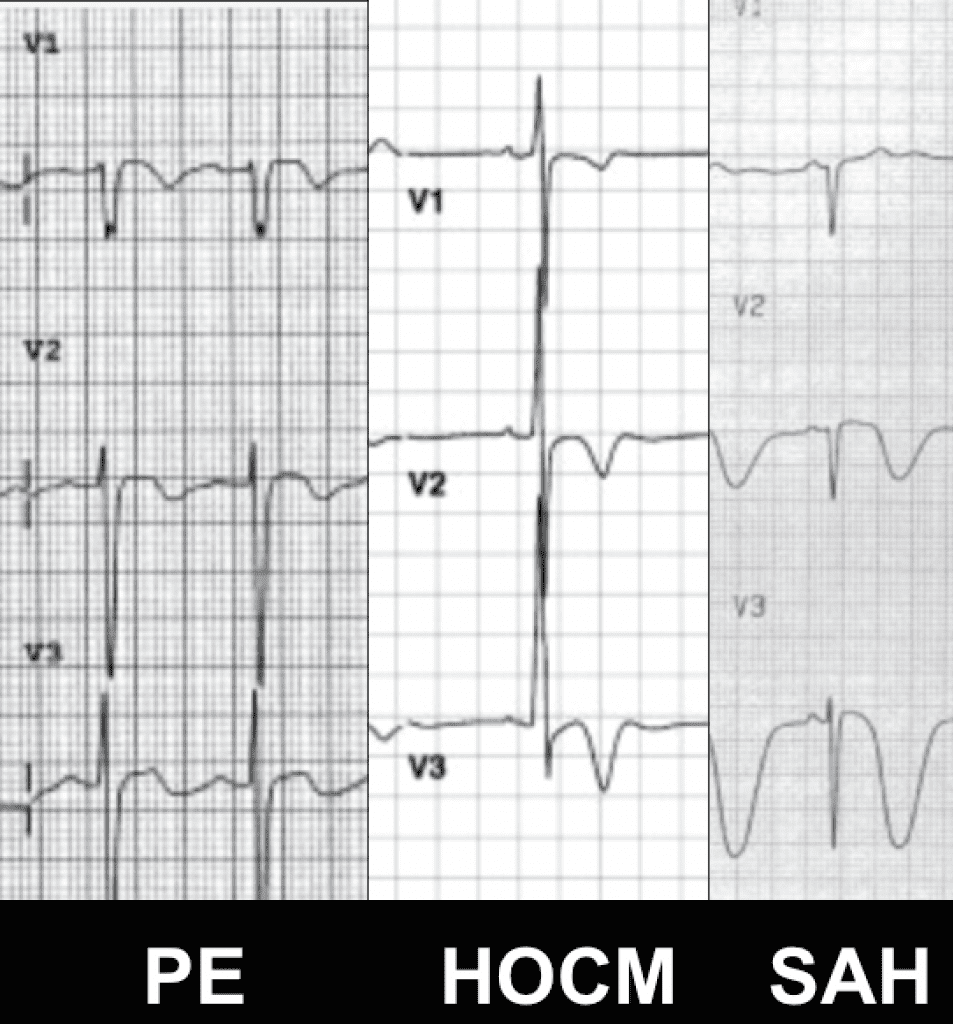
What else can cause t-wave inversions in the anterior ECG leads?
- Subarachnoid Hemorrhage
- Pericarditis
- Pulmonary Embolism
- Takotsubo Cardiomyopathy
- Electrolyte Abnormalities
- HOCM
- Pancreatitis
Why should we not perform exercise stress testing in patients with suspected Wellens’ Syndrome? [4]
The only evidence for this is case reports, not large randomized control trials, but stress testing can prove fatal as there is minimal collateral circulation to the proximal anterior myocardium (i.e. “The Widow Maker”).
How do you treat Wellens’ Syndrome? [2]
Oxygen, aspirin, nitroglycerin, and heparin or enoxaparin are the mainstay medical treatments of unstable angina, which is what Wellens’ Syndrome is, but in this specific case cardiac revascularization is also important. Specifically, how important is early revascularization vs medical management or delayed revascularization on morbidity and mortality?
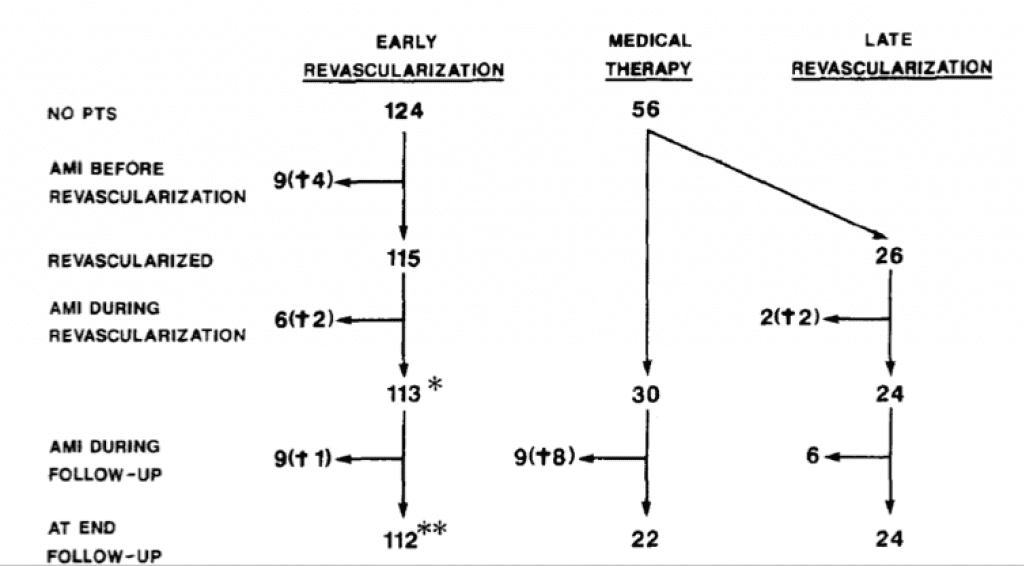
- 180 patients with Wellens’ ECG admitted and managed with either: Early Revascularization vs Medical Therapy
- Less likely to die with early revascularization vs medical therapy and/or late revascularization (2.6% vs 17.9%)
- Less likely to have AMI with early revascularization vs medical therapy and/or late revascularization (8.0% vs 30%)
Now Back to Our Patient…REBEL ECG of the Week: Wellens’ Syndrome or STEMI?
The reason our patient’s case is a STEMI and not Wellens’ Syndrome is….
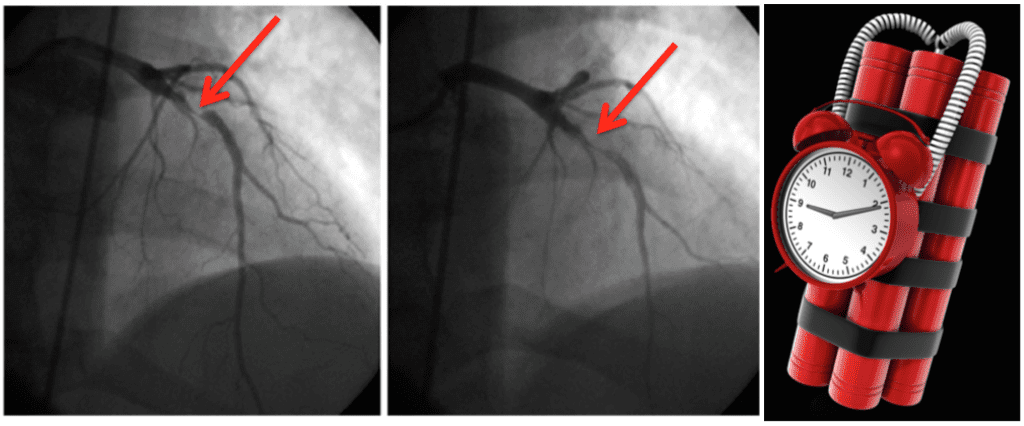
Since the patient was having active symptoms and no old ECG for comparison, we activated the cath lab and the patient was found to have a 60% Left Main (LM) Artery lesion and a 100% ostial Left Anterior Descending (LAD) Artery lesion. First troponin before heart cath was 30. This turned into an evolving STEMI….or more eloquently stated a subacute anterior STEMI.
In summary our patient has:
- Having ACTIVE Chest Pain
- ST-Segment Elevation (STE) in V1 – V3
- Sensitive Troponin I of 30 is not minimal
- Absence of R waves in precordial leads
Clinical Bottom Line for Wellens’ Syndrome:
- Wellens’ Syndrome signifies a high grade proximal LAD lesion until proven otherwise, but be sure to rule out other causes of ECG changes
- The ECG changes of Wellens’ can be transient, so you must have a high index of suspicion
- Stress testing, based on case reports, can induce a massive anterior myocardial infarction
- The treatment of choice to improve both morbidity and mortality in Wellens’ Syndrome is early heart catheterization
References:
- de Zwaan C et al. Characteristic Electrocardiographic Pattern Indicating a Critical Stenosis High in Left anterior Descending Coronary Artery in Patients Admitted Because of Impending Myocardial Infarction. Am Heart J 1982. PMID: 6121481
- de Zwaan C et al. Angiographic and Clinical Characteristics of Patients with Unstable Angina Showing an ECG Pattern Indicating Critical Narrowing of the Proximal LAD Coronary Artery. Am Heart J 1989. PMID: 2784024
- Hanna EB et al. ST-Segment Depression and T-Wave Inversion: Classification, Differential Diagnosis, and Caveats. Cleve Clin J Med 2011. PMID: 21632912
- Sowers N. Harbinger of Infarction: Wellens Syndrome Electrocardiographic Abnormalities in the Emergency Department. Can Fam Physician 2013. PMID: 23585602
For more on Wellens’ Syndrome Checkout:
- EMCurious Blog – Wellens’ Syndrome: A Case Study
- Amal Mattu’s Emergency ECG Video of the Week – Wellens Syndrome
- Dr. Smith’s ECG Blog – Wellens’ Waves Appear and Disappear Again and Again
- Life in The Fast Lane Blog – What is Wellens’ Syndrome?



