 You have just intubated a seizing eclamptic woman who is 34 weeks pregnant. As she is being prepped for transfer to the OB unit for an emergent C-section your nurse asks you what medications you would like for post intubation analgesia and sedation.
You have just intubated a seizing eclamptic woman who is 34 weeks pregnant. As she is being prepped for transfer to the OB unit for an emergent C-section your nurse asks you what medications you would like for post intubation analgesia and sedation.
You have limited recollection of whether Propofol crosses the placenta, and have legitimate concerns about Fentanyl’s chances of producing a ‘floppy baby’ for the OB team on delivery.
The literature on the most appropriate post intubation analgesia / sedation package for late pregnancy patients is limited. The agents we are the most familiar with in the emergency department for post intubation sedation and analgesia are Fentanyl and Propofol. One reliable mantra for post intubation analgesia and sedation is ‘Fentanyl is the sauce, and Propofol is the oregano’, it would be great to be able to apply this mantra to the pregnant population also.
Analgesia is the primary goal for post intubation care and sedation / anxiolysis is the secondary goal. The pasta sauce analogy emphasizes the need for analgesia first, and sedation second.
A lot of the literature focuses on the best agents for use in a crash C-section where the period of post intubation sedation is anticipated to be short, we also need to know the evidence behind the use of agents for longer term sedation for pregnant patients with medical disease that will not require immediate delivery.
A recent review of general anesthesia for Cesarean section by Devroe and colleagues can provide us with some guidance on this topic. [1]
Post intubation sedation / anesthesia for 3rd term pregnant women faces two significant challenges: Decreasing incidence, and the problem of intraoperative awareness.
- The incidence of general anesthesia for C-sections is decreasing dramatically with the increase in epidurals, causing a decrease in global experience with intubated 3rd trimester patients. [1]
- The 5th National audit project (NAP5) [2] reported a high incidence of intraoperative awareness in OB anesthesia (1:670) and attributed this to several risk factors, including a brief period of time between anesthetic induction and the start of surgery. NAP5 summary of main findings and incidences
MEDICATION OPTIONS
Fentanyl
Opioids have historically only been administered after clamping of the umbilical cord in an attempt to avoid neonatal respiratory depression. There are concerns regarding maternal hypotension with large doses of Fentanyl.
In the presence of pre-eclampsia, or maternal cardiac or neurological disease the judicious use of opioids can provide hemodynamic stability during laryngoscopy and surgery, and may offer protection from abrupt blood pressure changes. [1]
Devroe strongly recommends the use of Remifentanil (Synthetic opioid like Fentanyl, but more potent) in pre-eclamptic and other high risk patients where hemodynamic fluctuations need to be avoided. The use of this agent comes with the risk of neonatal respiratory depression.
The NAP5 authors did find that omission of opioids was a risk factor for intraoperative awareness.
Fentanyl Bottom Line: The use of opiates may reduce the risk of maternal awareness and improve maternal hemodynamic stability, so Fentanyl is a good choice as part of a post intubation sedation / analgesia package for any intubated 3rd trimester patient, and remember that Fentanyl is the sauce, and Propofol is the oregano. The other benefit of Fentanyl is that a reversal agent (Naloxone) exists in the event of significant neonatal respiratory depression after delivery.
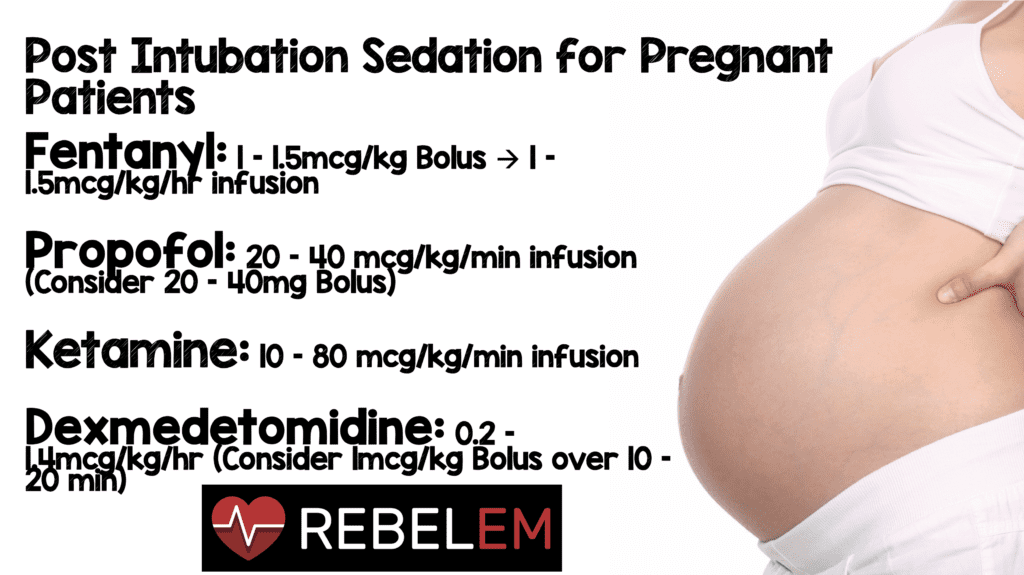
Dosing recommendation: 1-1.5 mcg/kg Fentanyl bolus, then 1-1.5 mcg/kg/hr infusion

Propofol
Expert opinion supports the use of Propofol as a standard induction agent for general anesthesia in cesarean section in healthy, non compromised patients. [1] Our sick patients in the emergency department are not healthy and if they require airway management, they are clearly compromised. Propofol in standard doses should be used with caution as an induction agent for critically ill patients, however it can be considered as part of a post intubation analgesia / sedation package.
Studies comparing Propofol with Thiopental:
- 32 women having elective C sections were openly randomized to 2.5 mg/kg of Propofol or 5 mg/kg of Thiopental, and then maintained on Nitrous oxide and Isofluorane until cord clamping. Buprenorphine was used as analgesia during surgery. Apgar scores for the neonates did not differ significantly. [3]
- 42 women having elective C sections were randomized to receive Propofol 2-2.5 mg/kg or Thiopental. They were maintained on Nitrous oxide and Isofluorane, and received 100 mcg of Fentanyl after the cord was clamped. There were no differences in 1 or 5 minute Apgar scores. [4]
These studies showed no difference in Apgar scores in the Propofol group, whereas a 1993 comparison of Thiopental, Propofol, and Midazolam showed a reduction in Apgar scores in the Propofol and Midazolam group (see Midazolam, below).
There is limited evidence for Propofol’s safety as a long term sedative for pregnant women.
Two studies exist that document the administration of several hours to days worth of Propofol sedation in an operating room / intensive care setting without adverse fetal effects.
- Hilton G, Andrzejowski JC. Prolonged Propofol Infusions in Pregnant Neurosurgical Patients. J Neurosurg Anesthesiol. Vol 19, Number 1, Jan 2007 (67-8) [5]
- 32 year old patient at 26 weeks gestation had an 11 hour anesthesia with Propofol and Remifentanil for excision of a vestibular schwannoma. Propofol was changed to Sevoflurane due to the onset of mild acidosis (pH drop from 7.5 to 7.37).
- 21 year old patient at 9 weeks gestation had a 10 hour anesthesia with Propofol and Remifentanil, also changed to Sevoflurane due to developing acidosis.
- Both mothers delivered healthy full term babies. The authors note that they would use Sevoflurane in future elective anesthesia cases.
- Bacon RC, Razis PA. The effect of Propofol sedation on neonatal condition. Anesthesia, 1994, Dec;49(12):1058-60 [6]
- 25 year old patient at 33 weeks gestation had a large intracerebral hemorrhage due to Moyamoya disease. She was sedated with 200 mg/h (approx. 40 mcg/kg/min for an 80 kg pt) of Propofol for 48 hours prior to emergent C section. Delivery was 7 minutes after Propofol infusion was stopped. Apgar scores were 3 at 1 minute and 8 at 5 minutes. The neonate developed respiratory failure 20 minutes later and was intubated for 3 days, making a full recovery.
Placental transfer of Propofol depends on placental blood flow and the concentration gradient between the mother and fetus. The induction dose, and the time from anesthesia to clamping of the umbilical cord probably have an important effect on the concentration of Propofol in the fetus. [3].
Propofol Bottom Line: For sick 3rd trimester patients, avoiding Propofol as the induction agent and aiming for a low infusion dose is a reasonable strategy for patients with anticipated long intubation to delivery times.
Dosing recommendation: 20-40 mcg/kg/min infusion, consider 20-40 mg bolus

Ketamine
In the presence of severe hemodynamic instability Ketamine (1-1.5 mg/kg) is considered an appropriate alternative for the induction of general anesthesia. [1]
Primate studies have shown both Ketamine, [1] and Propofol [7] to cause an increased rate of neuroapoptosis in newborn Macaque monkeys born to mothers that received high doses of these agents prior to delivery. It is unclear if these increased rates of neuroapoptosis are clinically significant, and the doses of Ketamine in these studies were much higher that used in clinical practice (10mg/kg induction, 10-85mg/kg/h infusion for 5 hours). For this reason (and increased airway reactivity) Ketamine is typically avoided on children <3 months of age.
In a randomized double blind study comparing Ketamine and Propofol as induction agents for elective C section [8] no difference in Apgar scores, time to perform procedure, or the need for Methergine or Oxytocin was found. Most patients were willing to have the same anesthetic technique for the next C section (81.3% propofol, 86% ketamine).
Ketamine Bottom Line: As an agent for induction of anesthesia, Ketamine is safe. There are better agents for maintenance of sedation available, however in the setting of hemodynamic compromise after a traumatic injury Ketamine would be an appropriate agent to use in this population. [1]
Dosing recommendation: 10-80 mcg/kg/min infusion (this is the same dosing range that is used for a straight Propofol strategy)

Dexmedetomidine (Precedex)
Dexmedetomidine is not an agent that every emergency physician is intimately familiar with, however its use is increasing and we need to be aware of its safety profile for use in pregnancy. Dexmedetomidine is rated category C in pregnancy. Dexmedetomidine is a selective apha 2 adrenergic receptor agonist that has both sedative and analgesic properties, with minimal respiratory depression. [9] Most studies on Dexmedetomidine have excluded pregnant patients.
There again is limited evidence for the use of Dexmedetomidine in the third trimester, mostly in the form of case reports, and brief post partum case series. Dexmedetimidine has minimal placental transfer, and can modulate the release of catecholamines, so may have a beneficial role when used with patients with eclampsia in controlling blood pressure.
Case Reports:
- Sami A. et al. Intravenous Dexmedetomidine infusion for labour analgesia in patient with preeclampsia. [10] Eur J Anaesthesiol 2009 Jan;26(1):86-7
- 32 year old woman at 38 weeks gestation with mild to moderate preeclampsia. Labor was induced, and an epidural was declined by the patient. Dexmedetomidine infusion was started without a bolus and after 3 hours a Caesarean section was performed due to late decelerations. Ramsay Sedation Scale (RSS) was 2 throughout the infusion (cooperative, oriented, tranquil). Apgars at delivery were 8 and 9.
- Machareth de Souza. Dexmedetomidine in General Anesthesia for Surgical Treatment of Cerebral Aneurysm in Pregnant Patient with Specific Hypertensive Disease of Pregnancy.[11] Rev Bras Anestesiol. 2005 Apr;55(2):212-6.
- 19 year old woman, 27 weeks gestation with a left sided deficit from a hemorrhagic stroke from an aneurysm in the posterior communicating artery, BP 170/110. Dexmedetomidine premedication at 1 mcg/kg over 20 minutes, then general anesthesia with 2.5 mg/kg Propofol, 7.5 mcg/kg Fentanyl, 1mg/kg Lidocaine, and 1.2 mg/kg Rocuronium. Anesthesia was maintained with Propofol 50 mcg/kg/min, Alfentanil 1 mcg/kg/min, and Dexmedetomidine 0.7 mcg/kg/h (decreased to 0.4 mcg/kg/h based on hemodynamic parameters) for 320 minutes. C section was performed at 37 weeks with normal delivery (no Apgars reported).
- Duan M, et al. Dexmedetomidine for Sedation in the Parturient With Respiratory Failure Requiring Noninvasive Ventilation [9] Respir Care 2012;57(11):1967-69 FREE FULL TEXT
- 16 year old woman, 31 weeks 6 days gestation in preterm labor. She developed respiratory failure with initial concern for pneumonia, and was placed on BiPAP for worsening hypoxemia. Dexmedetomidine bolus of 3 mcg/kg/h for 10 minutes, then an infusion at 0.2-0.6 mcg/kg/h was continued to allow the patient to tolerate BiPAP. On ICU day 1 she was transferred to the operating room and intubated for a forceps assisted vaginal delivery. Apgars at 1 and 5 minutes were 7 and 8. Duration of Dexmedetomidine infusion is not stated in the article.
Dexmedetomidine use AFTER delivery:
- Esmaoglu A. et al. Comparison between Dexmedetomidine and Midazolam for sedation of eclampsia patients in the intensive care unit Journal of Critical Care (2009) 24, 551-5 [12]
- 40 women randomized to Midazolam or Dexmedetomidine AFTER C section for eclampsia. Midazolam dosing was a 0.05 mg/kg bolus, then 0.1 mg/kg/h infusion. Dexmedetomidine dosing was a 1 mcg/kg bolus over 20 minutes, then a 0.7 mcg/kg/h infusion. Sedation was maintained to meet a RSS score of 2-3. Dexmedetomidine lowered heart rates at 1, 2, 3, 4, 5, 6, 12, and 24 hours more than Midazolam. It also lowered blood pressure at 5, 6, 12, and 24 hours and showed a decreased need for Nitroglycerine infusion (45% vs 90%) and Nitroprusside infusions (2/20 vs 13/20 patients). Duration of ICU stay was 83 hours for Midazolam vs 45.5 hours for the Dexmedetomidine group. There was no difference in additional Propofol or other analgesia requirements.
Dexmedetomidine Bottom Line: Dexmedetomidine is a feasible agent to use as a post intubation analgesic and sedative for those comfortable with its use in the non-pregnant patient. There is evidence to suggest its utility in the patient with ongoing severe hypertension from eclampsia, particularly in the post partum management phase in the ICU.
Dosing recommendation: infusion 0.2-1.4 mcg/kg/h (studies above used 0.7 mcg/kg/h) Consider 1 mcg/kg bolus iv over 10-20 minutes

Midazolam
Celleno, J Clin anesth. 1993, which induction agent for C section? [13]
3 groups of 30 patients received either 5mg/kg Thiopental, 2.4mg/kg Propofol or 0.3mg/kg Midazolam for induction of anesthesia. Anesthesia was maintained with Nitrous oxide and Isoflurane.
Midazolam had a slow induction time, and was associated with lower Apgar scores, and a lighter depth of anesthesia than Thiopental based on EEG pattern, and clinical signs of light plane of anesthesia: tearing, sweating, opening eyes. 50% of the Propofol group and 41% of the midazolam group were found to have a light plane of anesthesia.
Apgar scores at 1 minute were lower in the Propofol and Midazolam group than the Thiopental group. Apgar > 7 at 1 minute was 89% for Thiopental, 46% for Propofol and 51% for Midazolam, 5 min APGAR > 7 rates were 100% for all groups. Neonates whose mothers received Propofol or Midazolam as induction drugs had generalized hypotonus, and were drowsier during the first hour of life compared with the Thiopental group.
Midazolam Bottom Line: Midazolam shows no advantage over Propofol, and prolonged infusions of Midazolam are typically avoided in non pregnant patients due to its long duration of action.
For the post intubation sedation / analgesia of 3rd trimester women:
Fentanyl
- Safe
- May see some neonatal respiratory depression
- Benefits include a potential decrease in maternal awareness during delivery
Propofol
- Safe
- Preferred agent for induction in healthy non compromised patients
- Use a low infusion dose if prolonged infusion anticipated
Ketamine
- Safe
- Best reserved as sedative agent for patient with profound hemodynamic instability
- Some evidence to suggest neonatal harm in VERY large doses
Dexmedetomidine
- Safe
- Best used by providers with established experience with this agent
- Evidence supports its use for post partum management of eclamptic patients, with decreased ICU length of stay, and decreased use of antihypertensives when compared with Midazolam
Midazolam
- ‘Probably’ safe, but much better agents available for short to long term sedation (propofol)
My strategy:
- Sedation and analgesia using the same strategy I use with my other critically ill patients:
- Fentanyl bolus and drip at 1-1.5 mcg/kg/h and Propofol drip at 20-40mcg/kg/min.
- ‘Fentanyl is the sauce, Propofol is the oregano.’
References:
- Devroe S et al. General Anesthesia for Caesarean section. Curr Opin Anaesthesiol 2015. PMID: 25827280
- Pandit JJ et al. 5th National Audit Project (NAP5) on Accidental Awareness During General Anaesthesia: Summary of Main Findings and Risk Factors. Br J Anaesth 2014. PMID: 25204697
- Valtonen M et al. Comparison of Propofol and Thiopentone for Induction of Anaesthesia for Elective Caesarean Section. Anaesthesia 1989. PMID: 2802124
- Moore J et al. A Comparison Between Propofol and Thiopentone as Induction Agents in Obstetric Anaesthesia. Anaesthesia 1989. PMID: 2802123
- Hilton G et al. Prolonged Propofol Infusions in Ptregnant Neurosurgical Patients. Neurosurg Anesthesiol 2007. PMID: 17198107
- Bacon RC et al. The Effect of Propofol Sedation in Pregnancy on Neonatal Condition. Anaesthesia 1994. PMID: 7864321
- Creeley C et al. Propfol-Induced Apoptosis of Neurones and Oligodendrocytes in Fetal and Neonatal Rhesus Macaque Brain. Br J Anaesth 2013. PMID: 23722059
- Wanna O et al. A Comparison of Propofol and Ketamine as Induction Agents for Cesarean Section. J Med Assoc Thai 2004. PMID: 15521232
- Duan M et al. Dexmedetomidine for Sedation in the Parturient with Respiratory Failure Requiring Noninvasive Ventilation. Respir Care 2012. PMID: 22709960
- Abu-Halaweh SA et al. Intravenous Dexmedetomidine Infusion for Labour Analgesia in Patient with Preeclampsia. Eur J Anaesthesiol 2009. PMID: 19122562
- Souza KM et al. Dexmedetomidine in General Anesthesia for Surgical Treatment of Cerebral Aneurysm in Pregnant Patient with Specific Hypertensive Disease of Pregnancy: Case Report. Rev Bras Anestesiol 2005. PMID: 19471825
- Esmaoglu A et al. Comparison Between Dexmedetomidine and Midazolam for Sedation of Eclampsia Patients in the Intensive Care Unit. J Crit Care 2009. PMID: 19327948
- Celleno D et al. Which Induction Drug for Cesarean Section? A Comparison of thiopental Sodium, Propofol, and Midazolam. J Clin Anesth 1993. PMID: 8373604
Post Peer Reviewed By: Special Thank You to Haney Mallemat (Twitter: @CriticalCareNow) for his critique and feedback of this post.





