Topic #1: Intravascular Complications of Central Venous Catheter (CVC) Access
Topic #2: US vs Landmark Technique for Peripheral IV Access
REBEL Cast Episode 19: All Vascular Access
Click here for Direct Download of Podcast
Topic #1: Intravascular Complications of Central Venous Catheter (CVC) Access
Article:
- Parienti J.J et al. Intravascular Complications of Central Venous Catheterization by Insertion Site.N Engl J Med September 2015; 373:1220-1229.PMID: 26398070
Background:
Three anatomical sites are commonly used to insert central venous catheters, but insertion at each site has the potential for complications including infection, thrombosis and mechanical dysfunction (pneumothorax, hematoma). The authors’ previous research led them to believe that these complications will differ according to the site of insertion.
Clinical Question: Do major complications of central venous catheters differ by site of insertion (central, subclavian and femoral).
Population:
Patients age 18 and older who were admitted to an ICU setting and requiring non tunneled central venous vascular access and had at least two of the three sites appropriate for cannulation. Study was conducted in France in a total of ten different ICUs (4 university affiliated hospitals and 5 general hospitals).
Outcome (Primary):
- Incidence of major catheter-related complications (catheter related blood stream infections and symptomatic deep vein thrombosis – whichever came first) from the time of catheter insertion to 48 hours after catheter removal
Outcome (Secondary):
- Time to catheter-tip colonization and time to total deep – vein thrombosis after catheter removal.
- Rate of major mechanical complications during insertion of the central venous catheter and follow-up (arterial injury, hematoma, pneumothorax or other)
Design: Multi-center randomized comparative adverse outcomes trial
Excluded:
- If only one catheter site was available
Results:
- A total of 3471 catheters were inserted in 3027 patients.
- There were catheter related complications (blood stream infections and symptomatic deep vein thrombosis) in 8 of the subclavian, 20 of the jugular and 22 of the femoral groups respectively (1.5, 3.6, and 4.6 per 1000 catheter-days; P=0.02).
- In a pairwise comparison:
- Risk of catheter related complications were significantly higher in the femoral group than in the subclavian group (hazard ratio, 3.5; 95% confidence interval [CI], 1.5 to 7.8; P=0.003)
- Risk of catheter related complications were significantly higher in the jugular group than the subclavian group (hazard ratio, 2.1; 95% CI, 1.0 to 4.3; P=0.04)
- Risk of catheter related complications were similar in the femoral and the jugular groups (hazard ratio, 1.3; 95% CI, 0.8 to 2.1; P=0.30).
- In the three-choice comparison: pneumothorax requiring chest-tube insertion occurred in association with 13 (1.5%) of the subclavian vein insertions and 4 (0.5%) of the jugular-vein insertions.
Critical Findings
- The femoral site had the fewest mechanical complications, but the most thrombosis (1.4%).
- The subclavian site had the fewest infections (0.5%) and thrombotic events (0.5%), but the most mechanical complications (2.1%).
- The jugular site was essentially a middle ground between the two, although, had the greatest infection rate (1.4%).
Strengths:
- Large, multicenter trial
- Study asked a clear clinical question that was patient centered
- Only one exclusion criteria increasing applicability
Limitations:
- Ultrasound was not mandated which may have contributed to the high rates of mechanical complications in IJ lines
- No specific antibiotic dressings used regularly
- There was a high rate of failure and crossover in the subclavian arm (14.7%)
- The number of complications for each site was measured in the near-single digits, while 469 patients died before catheter removal – a large enough number of potentially unmeasured events to significantly affect the primary outcome.
- Only symptomatic patients were screened for thrombosis – again, leaving many patients with potentially missed outcomes
Other Issues:
- Selection bias: There was not 1:1:1 randomization for all patients – if the clinician elected to (they could choose to opt out of one site and enter into the 1:1 randomization). This issue could have decreased the complication rate in the subclavian group which was the most commonly excluded site.
Authors Conclusions: “Subclavian-vein catheterization was associated with a lower risk of bloodstream infection and symptomatic thrombosis and a higher risk of pneumothorax than jugular-vein or femoral-vein catheterization.”
Our Conclusions: A skilled or ultrasound guided subclavian is an ideal option but should be avoided if the operator is uncomfortable with he procedure. Based on the low rates of complications (including infectious complications) a femoral line is an excellent option when clinically indicated.
Potential impact to clinical practice: A subclavian central line should be considered first line in patients in whom infection of the line is the major concern but either an IJ or femoral line may be used if the patient is not a good candidate for a subclavian.
Bottom line: Although Subclavian lines appear to have a lower infection rate there is the tradeoff of more mechanical complications; ultimately the clinician should decide which site is the most appropriate on a patient to patient basis.
Read More
- EM Literature of Note: Central Line Showdown
- EM Nerd: The Case of the Blind Allocator
- The Bottom Line: Intravascular Complications of Central Venous Catheterization by Insertion Site
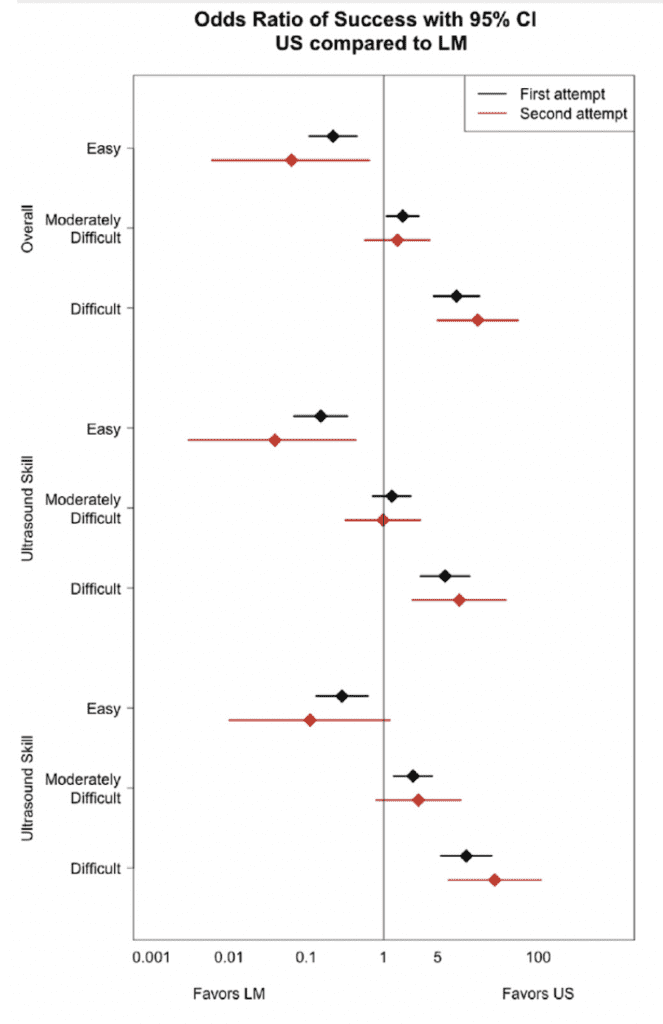
Topic #2: US vs Landmark Technique for Peripheral Intravenous (PIV) Cannulation
Background: One of the most common procedures performed in the ED is peripheral IV (PIV) access. Visual inspection and palpation to identify the vein has been the traditional means of gaining PIV access. The failure rate on first attempt ranges from 12 – 26% amongst adults, but can be even higher than this in “difficult access” patients. Ultrasound has gained lots of popularity in the past years and its use could potentially increase first attempt success rate, therefore decreases multiple attempts and therefore decreases pain for patients and delay in care. Looking at the CVC literature the use of ultrasound, if not already, should be standard care in placing central access. It has decreased number of attempts, time to cannulation, infection, as well as other complications commonly associated with CVC placement. The use of US in PIV access however is a little more inconsistent, due to prior small studies and heterogeneous patient populations. Currently, there just aren’t a lot of large randomized clinical trials having looked to answer this question of US vs landmark for PIV access, until now.
What Study Are We Discussing?
McCarthy ML et al. Ultrasonography Versus Landmark for Peripheral Intravenous Cannulation: A Randomized Controlled Trial.Ann Emerg Med 2015. [epub ahead of print] PMID: 26475248
What Question Are we Trying To Answer?
Does an Ultrasound-Guided technique or a Traditional Landmark technique for peripheral IV access have a higher 1stattempt success rate for peripheral IV cannulation?
What They Did:
- 2-Group, Parallel, Randomized, Controlled Trial of 1,189 Adult ED Patients from a single center
- Randomized to Landmark vs Ultrasonography
- Patients also stratified by difficulty of access: Difficult, Moderately Difficult, and Easy
- If 1stattempt failed, randomized subjects a 2ndtime
- Exclusion Criteria: All High-acuity patients (Triage level 1 – 2 patients)
Definitions:
- Difficult Access= No visualization or ability to palpate a vein in either upper extremity
- Moderately Difficult Access= Visualization or ability to palpate at least 1 vein, but anticipation of difficulty using landmark technique
- Easy Access= Visualization or palpation of at least 1 vein and anticipation of easy access using landmark technique
- Successful Cannulation = infusion of fluid without infiltration
Outcomes:
- Primary:1stand 2ndattempt success or failure rate of cannulation of peripheral vein
- Secondary: Occurrence of complications, patient-reported pain (0 = no pain and 10 = extremely painful), and duration of 1stattempt
Results:
- 33 out of 36 Technicians Participated
- Enrolled a median of 26 subjects (Interquartile range 9 – 55)
- 39% of technicians reported placing 5 or more US PIV lines
- Patient Population:
- Mean Age: 45.5 Years
- 63% Women
- 37% Classified as Obese
- 76% of PIV lines were placed in antecubital fossa
- Initial Cannulation Success Rate was 81% overall
- 1stattempt success rate for US PIV line placement = 82 – 86% regardless of difficulty
- 1stattempt success rate for landmark line placement = 35 – 97% by difficulty of IV access
- Overall Success 1stAttempt Success Rate:
- Difficult Access Patients: US 0 more successes per 100 tries vs Landmark
- Moderately Difficult Access Patients: US 10.2 more successes per 100 tries vs Landmark
- Easy Access Patients: Landmark 10.6 more successes per 100 tries vs US
- More Skilled Technicians had Higher Success Rates with US vs Less Skilled Technicians:
- Difficult Access Patients: US 9.4 more successes per 100 attempts
- Moderately Difficult Access Patients: US 9.7 more successes per 100 attempts
- Easy Access: US 7.9 more successes per 100 attempts
- Failed 1stAttempt Access:
- 197 patients randomized a 2ndtime
- Overall 69% success rate of PIV insertion on 2ndattempt
- Difficult Access: US 59.9 more successes per 100 attempts vs Landmark
- Moderately Difficult Access: US 8.8 more successes per 100 attempts vs Landmark
- Easy Access: Landmark 31.8 more successes per 100 attempts vs US
- 2nd attempt success rates were also higher with US among technicians with more US PIV skill
- Time of Procedure:
- Procedure took almost twice as long with US vs landmark (Range of median difference 79 – 97 seconds longer with US)
- Median Pain Rating
- US PIV was 1 point higher vs Landmark regardless of difficulty of IV access
- Difficult Access: 2 vs 1
- Moderately Difficult Access: 3 vs 2
- Easy Access: 3 vs 2
- Complications:
- No statistically significant difference in complication rates by procedural method
- IV infiltration was the most common complication
- Difficult access: US 0% vs LM 3.4%
- Moderately Difficult Access: US 4.6% vs LM 8.7%
- Easy Access: US 14.3% vs LM 0%
Strengths:
- This is the largest RCT to date evaluating use of US vs Landmark for PIV access in adult ED patients.
- Statisticians were blinded to procedural assignments
- The trial examined the influence of technician skill on success based on number of ultrasonographic PIV lines placed during a typical shift (i.e. <5 vs ≥5)
- 33 out of 36 technicians (92%) that worked in the ED participated in the study
Limitations:
- This was a convenience sample of adult patients from 9am – 9pm, which limits generalizability of the study. 9 other research studies were ongoing during this particular research study, which could have served as a particular distraction. US PIV takes longer to perform, and in many EDs the staffing is typically trimmed down to a “skeleton” crew overnight, making it more difficult to dedicate the time to this procedure. Also, there may also be a difference in types of patients that present during the day vs overnight (i.e. intoxicated), which may limit cooperation. Finally, children were not enrolled in this study, and these findings may not extrapolate to a pediatric population.
- This trial was not powered to test for a significant interaction effect between treatment method and operator.
Discussion:
- Typically PIV cannulation is the responsibility of nursing, however in this study ED technicians performed the PIV cannulations as well as classified subjects as difficult, moderately difficult, or easy access according to visible or palpable veins and perception of difficulty. It is important to note that even though technicians were used, that is the standard procedure for this ED. In this study all technicians complete training of ultrasonographic PIV cannulation (i.e. 2hr lecture and hands-on demonstration + 10 successful ultrasonographic PIV procedures under preceptor supervision). Also, 82% of the technicians who participated at 1 or more years of experience placing ultrasonographic PIV lines.
- This study was only able to detect a 10% or greater difference between techniques in the first attempt groups with easy access, 20% or greater difference in the moderately difficult and difficult access groups. This means that smaller differences may not have been detected in this study.
- There is no universally accepted definition of difficulty of access with several other studies using failed intravenous access, clinician suspicion of difficult access, or absence of visible or palpable vein.
- In patients who are anticipated to have easy peripheral IV access, traditional landmark techniques have a better 1stand 2ndsuccess rate vs ultrasound-guided techniques.However, in patients who are anticipated to have more difficult peripheral IV access, the ultrasound-guided technique has a better 1stand 2ndsuccess rate vs the traditional landmark technique. I would also argue that if a patient has difficult IV access you will probably get IV access faster with US guided IV, as opposed to waiting for your nurses or technicians to attempt multiple times before asking for the ultrasound guided IV.
Author Conclusion: “Ultrasonographic peripheral intravenous cannulation is advantageous among patients with difficult or moderately difficult intravenous access but is disadvantageous among patients anticipated to have easy access.”
Clinical Take Home Point: If a patient needs peripheral IV access and has visible and/or palpable veins, stick with the traditional landmark technique of IV access as this is quicker and has a better 1stand 2ndattempt rate vs ultrasound guided techniques. However, if you have a patient that has peripheral veins that are not visible and/or palpable consider jumping to ultrasound guided peripheral IVs.
References:
- McCarthy ML et al. Ultrasonography Versus Landmark for Peripheral Intravenous Cannulation: A Randomized Controlled Trial. Ann Emerg Med 2015. [epub ahead of print] PMID: 26475248
For more on what others thought on these topics checkout:
CVC Access
- EM Literature of Note: Central Line Showdown
- EM Nerd: The Case of the Blind Allocator
- The Bottom Line: Intravascular Complications of Central Venous Catheterization by Insertion Site
- Vibha Gupta at CORE EM: Intravascular Complications of Central Line by Insertion Site
US Guided Peripheral IV Access
- Jacob Avila at 5 Minute Sono Blog: Who Gets an US-Guided IV?
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)



