 Background: The two most important things that we can do in cardiac arrest to improve survival and neurologically intact outcomes is high quality CPR, with limited interruptions and early defibrillation. In the case of the former, the 2015 AHA/ACC CPR updates recommended a compression rate of 100 -120/min, a depth of 2 – 2.4in, allowing full recoil, and minimizing pauses. This is a lot to remember during a stressful code situation and one way many providers are offloading themselves cognitively is by the use of mechancical CPR (mCPR) devices. In theory these devices compress at a fixed rate, and depth, with the added benefit that the machine simply does not tire out. Additionally, use of this device allows another provider to be available for other procedures and interventions. A recent systematic review and meta-analysis in looked at five randomized clinical trials with over 10,000 patients with out-of-hospital cardiac arrest (OHCA) (Gates 2015). They concluded that there was no difference in ROSC, survival or survival with good neurological outcomes with the use of these devices compared to manual CPR. It is important to state that none of these studies showed increased harm either. A new paper just published in Circulation however, argues that mCPR during OHCA was associated with lower neurologically intact survival.
Background: The two most important things that we can do in cardiac arrest to improve survival and neurologically intact outcomes is high quality CPR, with limited interruptions and early defibrillation. In the case of the former, the 2015 AHA/ACC CPR updates recommended a compression rate of 100 -120/min, a depth of 2 – 2.4in, allowing full recoil, and minimizing pauses. This is a lot to remember during a stressful code situation and one way many providers are offloading themselves cognitively is by the use of mechancical CPR (mCPR) devices. In theory these devices compress at a fixed rate, and depth, with the added benefit that the machine simply does not tire out. Additionally, use of this device allows another provider to be available for other procedures and interventions. A recent systematic review and meta-analysis in looked at five randomized clinical trials with over 10,000 patients with out-of-hospital cardiac arrest (OHCA) (Gates 2015). They concluded that there was no difference in ROSC, survival or survival with good neurological outcomes with the use of these devices compared to manual CPR. It is important to state that none of these studies showed increased harm either. A new paper just published in Circulation however, argues that mCPR during OHCA was associated with lower neurologically intact survival.
Episode 34: The Death of Mechanical CPR (mCPR)?
Click here for Direct Download of Podcast
Article:
- Buckler DG et al. Association of mechanical cardiopulmonary resuscitation device use with cardiac arrest outcomes: a population-based study using the CARES registry (Cardiac Arrest Registry to Enhance Survival). Circulation 2016; 134: 2131-33. PMID: 27994028
Clinical Question: How does mCPR effect outcomes in OHCA?
What They Did:
- Cardiac Arrest Registry to Enhance Survival (CARES) is a US national registry of OHCA
- This registry was analyzed for adults with non-traumatic OHCA
- Compared patients treated with mCPR vs manual CPR
Outcomes:
- Primary: Neurologically favorable survival at hospital discharge (Defined as Cerebral Performance Category of 1 or 2)
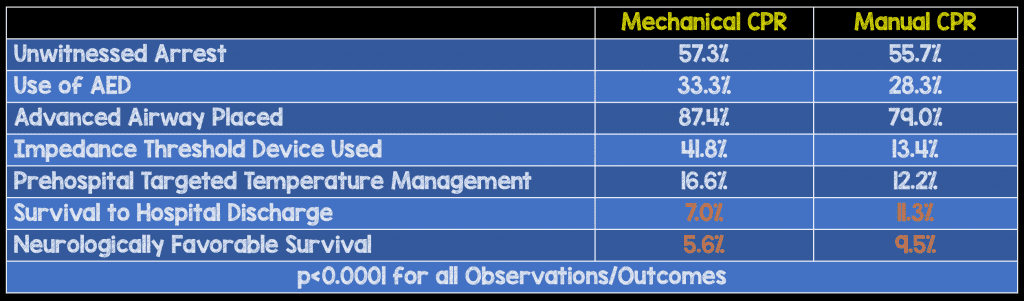
Results:
- 80,861 patients were included in the analysis
- Median age was 62 years
- 1% received bystander CPR
Strengths:
- Used a multivariable logistic regression model to control for arrest characteristics (Including: age, arrest location, bystander CPR, AED use, witnessed arrest status, initial rhythm, post arrest targeted temperature management, successful advanced airway placement, and impedance threshold device use)
- Large, real life look at the use of mCPR in OHCA as opposed to prior work that was done in research setting
- Primary outcome is clinically important and patient centered
Limitations:
- Retrospective secondary analysis
- Time of arrest, time of first CPR, and timing of interventions were not reliably reported
- Interventions aside from mCPR not detailed here (with the exception of advanced airway and ITD)
- Large variations in use of mCPR use by various EMS services (Ranged from 21.7% to >75% of OHCA cases)
Author Conclusion: “In conclusion, the use of mCPR during out-of-hospital cardiac arrest was associated with lower neurologically favorable survival within emergency medical services agencies participating in CARES. Although the use of mCPR devices increased during the study period, deployment rates remained highly variable, and the majority of agencies did not use them. Further research is required to identify circumstances in which mCPR may benefit patients with out-of hospital cardiac arrest; however our data indicate that mCPR for routine cardiac arrest care was associated with worse outcomes.”
Special Guests:
Be sure to checkout Joe’s Rant on Mechanical CPR (mCPR) on the Podcast

Joe Bellezzo, MD
Chief, Department of Emergency Medicine
ED ECMO Director
Ultrasound Director
Sharp Memorial Hospital
San Diego, CA
Blog: ED ECMO
Conference Director: Reanimate
Twitter: @edecmo
Scott Weingart Weighs In:
Retrospective registry trials shouldn’t be published after RCT data is available because they don’t provide meaningful answers. The issue with retrospective registry trials is it can only demonstrate association not causation even with multivariate analysis. There are numerous RCTs now published evaluating mCPR vs manual CPR in the prehospital setting and the best evidence is there is no evidence of harm what so ever with the use of mCPR. Additionally, the trial at hand did not evaluate in-hospital use of mCPR, especially ED use. These patients have probably had many minutes of CPR already, so the question is what is the most effective way to continue CPR?

Scott Weingart, MD
Associate Professor of Emergency Medicine
Chief of Division of Emergency Critical Care
Stony Brook School of Medicine, Stony Brook, NY
Twitter: @emcrit
Blog: emcrit.org
Clinical Take Home Point: This is not the death of mCPR, and although the authors of this paper must be commended for taking confounding variables into account in this large trial, it is retrospective and observational and therefore conclusions must be taken with a grain of salt.
For More on This Topic Checkout:
- Rory Spiegel at EMNerd (EMCrit): The Case of the Bridge to Nowhere
- Maia Dorsett at EMS Med: One Size Does Not Fit All – Should We Be Using Mechanical CPR in OHCA?
References:
- Buckler DG et al. Association of Mechanical Cardiopulmonary Resuscitation Device Use With Cardiac Arrest Outcomes: A Population-Based Study Using the CARES Registry (Cardiac Arrest Registry to Enhance Survival). Circulation 2016; 134: 2131 – 2133. PMID: 27994028
- Gates S et al. Mechanical Chest Compression for Out of Hospital Cardiac Arrest: Systematic Review and Meta-Analysis. Resuscitation 2015; 94: 91 – 7. PMID: 26190673
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)