 Background: Out-of-hospital cardiac arrest (OHCA) occurs in the United States at a rate of nearly 300,000 individuals per year. Even more concerning is the high mortality rate which is associated with this. The majority of OHCA is due to cardiac etiology with the most common initial rhythm being ventricular fibrillation (VF). What we all know is that high-quality, limited interruption cardiopulmonary resuscitation (CPR) and early defibrillation are the hallmarks of successful neurologic outcomes in OHCA. For many who have heard me speak about ACLS, you have heard me say that these guidelines are created for the providers who do not perform resuscitation as part of their daily routine. For those of us in the trenches of the emergency department, we have to think beyond ACLS at times. Although VF typically responds very well to the standard energies of defibrillation, maybe in patients with higher body mass index or morbid obesity we need higher energies to achieve successful defibrillation.
Background: Out-of-hospital cardiac arrest (OHCA) occurs in the United States at a rate of nearly 300,000 individuals per year. Even more concerning is the high mortality rate which is associated with this. The majority of OHCA is due to cardiac etiology with the most common initial rhythm being ventricular fibrillation (VF). What we all know is that high-quality, limited interruption cardiopulmonary resuscitation (CPR) and early defibrillation are the hallmarks of successful neurologic outcomes in OHCA. For many who have heard me speak about ACLS, you have heard me say that these guidelines are created for the providers who do not perform resuscitation as part of their daily routine. For those of us in the trenches of the emergency department, we have to think beyond ACLS at times. Although VF typically responds very well to the standard energies of defibrillation, maybe in patients with higher body mass index or morbid obesity we need higher energies to achieve successful defibrillation.
What They Did:
- Describe a novel approach of “high-energy” defibrillation in a patient with intractable VF after cardiac arrest
How do you perform dual simultaneous external defibrillation?
- This procedure should only be used in refractory ventricular fibrillation after multiple attempts at defibrillation and appropriate medications have been given
- Using a second defibrillator, you can place a second set of external defibrillation pads next to each other, but ensure that the pads are not making contact with each other
- Charge both monitors (360J for monophasic and 200J for biphasic)
- Ensure everyone is clear of the patient
- Simultaneously press the shock button on both monitors
- Immediately resume CPR
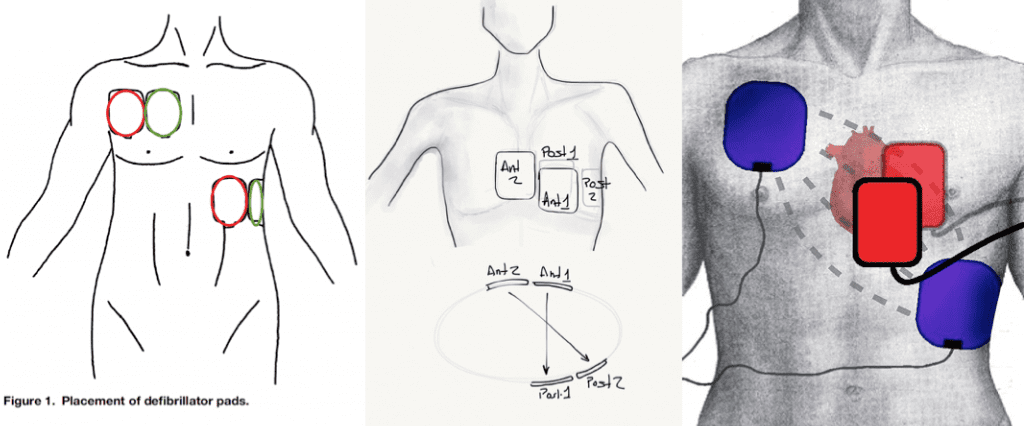
All of the above are acceptable ways to place the pads
Discussion:
 Now I get it, in the scheme of evidence based medicine, case reports are amongst one of the lowest forms of evidence, but hear me out. I am not talking about doing this on every patient with VF. I am talking about the patient who you have tried to defibrillate several times unsuccessfully; I am talking about thinking outside the box. What do you have to lose? The patient is going to die if you are not able to get a perfusing rhythm. So after high quality CPR, multiple rounds of defibrillation, and appropriate medications, if you still have refractory VF, why not just give this a try?
Now I get it, in the scheme of evidence based medicine, case reports are amongst one of the lowest forms of evidence, but hear me out. I am not talking about doing this on every patient with VF. I am talking about the patient who you have tried to defibrillate several times unsuccessfully; I am talking about thinking outside the box. What do you have to lose? The patient is going to die if you are not able to get a perfusing rhythm. So after high quality CPR, multiple rounds of defibrillation, and appropriate medications, if you still have refractory VF, why not just give this a try?- Body habitus is an important variable for successful defibrillation. Lets face it; our population is not getting thinner. Obesity is not discussed in ACLS. The amount of tissue that electricity has to get through will affect the amount of effective energy that will be delivered to the fibrillating heart. Although this was a swine model, Zhang Y et al [2] did show that there was an inverse relationship of body mass with successful defibrillation.
- There is also an older case series in JACC from 1994 [3] that describes 5 patients with cardiomyopathy or Wolff-Parkinson-White (WPW) Syndrome undergoing electrophysiology studies failing to convert out of VF after 7 – 20 shocks with monophasic energies ranging from 200 – 360J. All 5 patients finally converted after getting a double shock with a total of 720J
- There was also a recent retrospective case series by Cabanas JG et al [4] of 10 cases of refractory VF. Patients got at least 5 unsuccessful single shocks, epinephrine administration, and a dose of anti arrhythmic medication before double sequential external defibrillation (DSED) was attempted. VF broke in 7/10 (70%) of cases, only 3/10 (30%) had ROSC in the field, and 0/10 (0%) survived to discharge.
Clinical Take Home Point: Consider using high-energy, dual simultaneous defibrillation in patients with refractory VF only after high quality CPR, several attempts at defibrillation, and appropriate medications have been given.
References:
- Leacock BW. Double Simultaneous Defibrillators for Refractory Ventricular Fibrillation. JEM 2014; 46 (4): 472 – 74. PMID: 24462025
- Zhang Y et al. Body Weight is a Predictor of Biphasic Shock Success for Low Energy Transthoracic Defibrillation. Resuscitation 2002; 54: 281 – 7. PMID: 12204462
- Hoch DH et al. Double Sequential External Shocks for Refractory Ventricular fibrillation. JACC 1994; 23: 1141 – 5. PMID: 8144780
- Cabanas JG et al. Double Sequential External Defibrillation in Out-of-Hospital Refractory Ventricular Fibrillation: A Report of Ten Cases. Perhaps Emerg Care 2015; 19 (1): 126 – 130. PMID: 25243771
- Merlin MA et al. A Case Series of Double Sequence Defibrillation. Prehospital Emergency Care. 2016 Jan 29:1-4. [epub ahead of print]
- Ross EM et al. Dual Defibrillation in Out-Of-hospital Cardiac Arrest: A Retrospective Cohort Analysis. Resuscitation 2016; 106:14-7. PMID: 27344928
For More Thoughts on This Topic Checkout:
- Amal Mattu at UMEM Educational Pearls: Non-Stop VFib? Double-Down on the Defib!
- Charles Bruen at Resus Review: High Energy Defibrillation for Incessant Ventricular Fibrillation
- Thomas D at ScanCrit: The One-Two Punch
- Jess Mason at EM:RAP: Double Sequential Defibrillation
- The Resus Room: Double Sequential Defibrillation
- First10EM: Double Sequential Defibrillation (The DOSE VF Trial)
Post Peer Reviewed By: Anand Swaminathan (Twitter @EMSwami)



