What are Some Other Options for Benzodiazepine-Refractory Alcohol Withdrawal?
What is the Evidence for Each of These Medications?
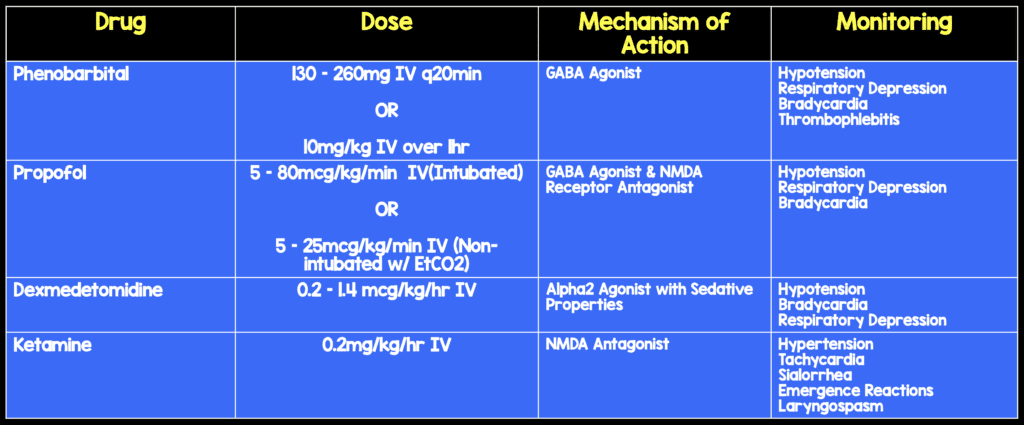
Phenobarbital
- 296 Patients
- 1 Prospective Trial [1]
- One prospective RCT with phenobarbital 10mg/kg vs placebo (+symptom-triggered lorazepam for both groups) showed significant decrease in both ICU admission rate and continuous lorazepam infusion use (1 single center trial, results have not been duplicated)
- 1 Retrospective Trial [2]
Propofol
- 225 Patients
- 5 Retrospective Trials [3 – 7]
- 1 Case Series [8]
- 3 Case Reports [9 – 11]
Dexmedetomidine
- 6 Retrospective Trials [6 – 7; 12 – 15]
- 4 Case Reports/Case Series [16 – 19]
- 1 Prospective Trial [20]
- Dexemedetomidine does not protect against withdrawal seizures and should not be used as monotherapy
Ketamine
- 1 Retrospective Review [21]
Clinical Bottom Line
- Phenobarbital, propofol, and dexmedetomidine have been shown to reduce benzodiazepine requirements in AWS
- Nothing has proven to shorten AWS duration or ICU LOS
- Dexmedetomidine does not protect against withdrawal seizures and should not be used as monotherapy
References:
- Rosenson J et al. Phenobarbital for acute alcohol withdrawal: a prospective randomized double-blind placebo-controlled study. J Emerg Med. 2013;44:592-598.e2. PMID: 22999778
- Michaelsen IH et al. Phenobarbital versus diazepam for delirium tremens: a retrospective study. Dan Med Bull. 2010; 57 (8) A4169. PMID: 20682133
- Sohraby R et al. Use of propofol-containing versus benzodiazepine regimens for alcohol withdrawal requiring mechanical ventilation. Ann Pharmacother. 2014;48:456-461. PMID: 24436457
- Lorentzen K et al. Use of propofol infusion in alcohol withdrawal-induced refractory delirium tremens. Dan Med J. 2014;61:A4807. PMID: 24814732
- Wong A et al. Management of benzodiazepine-resistant alcohol withdrawal across a healthcare system: benzodiazepine dose escalation with or without propofol. Drug Alcohol Depend. 2015;154:296-299. PMID: 2605315
- Lizotte RJ et al. Evaluating the effects of dexmedetomidine compared to propofol as adjunctive therapy in patients with alcohol withdrawal. Clin Pharmacol. 2014;6:171-177. PMID: 25382987
- Ludtke K et al. Retrospective review of critically ill patients experiencing alcohol withdrawal: dexmedetomidine versus propofol and/or lorazepam continuous infusions. Hosp Pharm. 2015;50:208-213. PMID: 26405310
- McCowan C, Marik P. Refractory delirium tremens treatedwith propofol: a case series. Crit Care Med. 2000;28:1781-1784. PMID: 10890619
- Hughes DW et al. Propofol for benzodiazepine-refractory alcohol withdrawal in a non-mechanically ventilated patient. Am J Emerg Med. 2014;32:112.e3-112.e4. PMID: 24075805
- Coomes TR, Smith SW. Successful use of propofol in refractory delirium tremens. Ann Emerg Med. 1997;30:825-828. PMID: 9398785
- Mahajan R et al. Use of propofol as adjuvant therapy in refractory delirium tremens. Ind Psychiatry J. 2010;19:58-59. PMCID: PMC3105562
- Crispo AL et al. Comparison of clinical outcomes in nonintubated patients with severe alcohol withdrawal syndrome treated with continuous-infusion sedatives: dexmedetomidine versus benzodiazepines. Pharmacotherapy. 2014;34:910-917. PMID: 24898418
- Frazee EN et al. Influence of dexmedetomidine therapy on the management of severe alcohol withdrawal syndrome in critically ill patients. J Crit Care. 2014;29:298-302. PMID: 24360597
- Rayner SG et al. Dexmedetomidine as adjunct treatment for severe alcohol withdrawal in the ICU. Ann Intensive Care. 2012;2:12. PMID: 22620986
- VanderWeide LA et al. Evaluation of early dexmedetomidine addition to the standard of care for severe alcohol withdrawal in the ICU: a retrospective controlled cohort study. J Intensive Care Med 2016; 31(3): 198 – 204). PMID: 25326428
- Baddigam K et al. Dexmedetomidine in the treatment of withdrawal syndromes in cardiothoracic surgery patients. J Intensive Care Med. 2005;20:118-123. PMID: 15855224
- Darrouj J et al. Dexmedetomidine infusion as adjunctive therapy to benzodiazepines for acute alcohol withdrawal. Ann Pharmacother. 2008;42:1703-1705. PMID: 18780809
- Muzyk AJ et al. The use of dexmedetomidine in alcohol withdrawal. J Neuropsychiatry Clin Neurosci. 2012; 24: E45-E46. PMID: 23037682
- Rovasalo A et al. Dexmedetomidine as an adjuvant in the treatment of alcohol withdrawal delirium: a case report. Gen Hosp Psychiatry. 2006;28:362-363. PMID: 16814639
- Mueller SW et al. A randomized, double-blind, placebo-controlled dose range study of dexmedetomidine as adjunctive therapy for alcohol withdrawal. Crit Care Med. 2014;42:1131-1139. PMID: 24351375
- Wong A et al. Evaluation of adjunctive ketamine to benzodiazepines for management of alcohol withdrawal syndrome. Ann Pharmacother. 2015;49:14-19. PMID: 25325907
For More on This Topic Checkout:
- Justin Morgenstern at First 10 in EM: Management of Delirium Tremens
- Josh Farkas at Pulmcrit/EMCrit: Phenobarbital Monotherapy for Alcohol Withdrawal – Simplicity and Power
- Bryan Hayes at ALiEM: Ketamine for Severe Ethanol Withdrawal – A New Hope?
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)



