 Background: Respiratory tract infections and pneumonia are the 3rd leading cause of death worldwide. Although morbidity and mortality has improved slightly with the advent of antibiotics, there is still a significant long-term morbidity and mortality associated with this disorder. It is well known that in pneumonia, there is an excess release of circulating inflammatory cytokines which cause further pulmonary dysfunction. Maybe the use of systemic corticosteroids, which have anti-inflammatory effects, could help attenuate this systemic inflammatory process and thus improve outcomes. So is there any benefit to adjunct prednisone therapy in community acquired pneumonia?
Background: Respiratory tract infections and pneumonia are the 3rd leading cause of death worldwide. Although morbidity and mortality has improved slightly with the advent of antibiotics, there is still a significant long-term morbidity and mortality associated with this disorder. It is well known that in pneumonia, there is an excess release of circulating inflammatory cytokines which cause further pulmonary dysfunction. Maybe the use of systemic corticosteroids, which have anti-inflammatory effects, could help attenuate this systemic inflammatory process and thus improve outcomes. So is there any benefit to adjunct prednisone therapy in community acquired pneumonia?
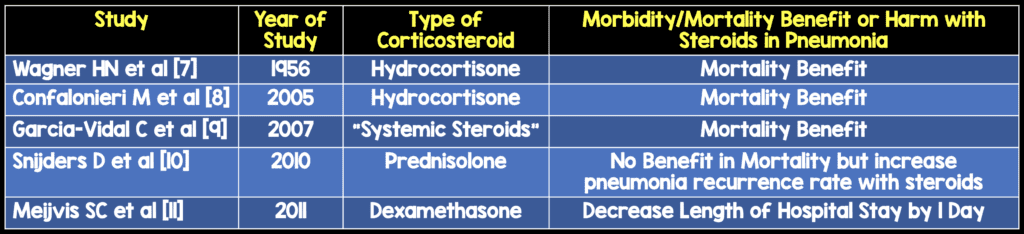
Are there studies evaluating the use of steroids in pneumonia?
Are there larger studies or reviews evaluating the use of steroids in pneumonia?
Systematic Reviews:
- Siempos II et al (2008) [1]
- Chen Y et al (2011) [2]
Meta-Analyses:
- Nie W et al (2012) [3]
- Shafiq M et al (2013) [4]
- Lamontagne F et al (2013) [5]
Conclusion of all larger trials: Adjunct corticosteroids in community acquired pneumonia might be beneficial, but a large, adequately powered randomized trial is warranted

What is the most recent literature evaluating adjunct corticosteroids in community acquired pneumonia?
Blum CA et al (January 2015) [6]
Methods:
- Largest, Double-Blind, Multicenter, Randomized, Placebo Controlled Trial
- 785 Patients from 7 Hospitals in Switzerland
- Augmentin or Rocephin Alone for Community Acquired Pneumonia + Clarithromycin if Concern for ICU/Legionella
- Prednisone 50mg PO qDay vs Placebo PO qDay x7days
Outcomes:
- Primary Outcome – Time to clinical stability (Days until stable vital signs x24hours)
- Secondary Outcome – Hospital Length of Stay, IV Antibiotics
Results:
- Median Time to Clinical Stability: 3 days (prednisone) vs 4.4 days (placebo)
- Hospital Length of Stay: 6 days (prednisone) vs 7 days (placebo)
- Need for IV Antibiotics: 4 days (prednisone) vs 5 days (placebo)
- Incidence of Hyperglycemia Requiring Insulin Tx: 19% (prednisone) vs 11% (placebo)
Limitations:
- Only admitted patients, therefore we don’t know how this works in patients treated as outpatients
- The study was not powered for mortality
- The primary endpoint is a combined endpoint of several vital signs
- Asthma patients not teased out in this study
- Prednisone has a bitter taste and therefore may have unblinded patients
- Hyperglycemic events may have unblinded researchers
Conclusion of Study: Prednisone treatment for 7 days in patients with community-acquired pneumonia shortens time to clinical stability without an increase in complications
Although this study certainly showed some benefit in patient centered outcomes and hospital costs/efficiency, there was an increase in hyperglycemia and the study was not powered to show mortality benefit. We are still lacking a large, adequately powered randomized trial and therefore the use of systemic steroids should not be adopted into clinical practice at this time
References:
- Siempos II et al. Adjunctive Therapies for Community-Acquired Pneumonia: A Systematic Review. J Antimicrob Chemother 2008. PMID: 18641037
- Chen Y et al. Corticosteroids for Pneumonia. Cochrane Database Syst Rev 2011. PMID: 21412908
- Nie W et al. Corticosteroids in the Treatment of Community-Acquired Pneumonia in Adults: A Meta-Analysis. PLoS One 2012. PMID: 23112872
- Shafiq M et al. Adjuvant Steroid Therapy in Community-Acquired Pneumonia: A systematic Review and Meta-Analysis. J Hosp Med 2013. PMID: 23184813
- Lamontagne F et al. Corticosteroid use in the Intensive Care Unit: A Survey of Intensivists. Can J Anaesth 2013. PMID: 23606231
- Blum CA et al. Adjunct Prednisone therapy for Patients with Community-Acquired Pneumonia: A Multicentre, Double-Blind, Randomised, Placebo-Controlled Trial. Lancet 2015. PMID: 25608756
- Wagner HN et al. The Effect of Hydrocortisone Upon the course of Pneumococcal Pneumonia Treated with Penicillin. Bull Johns Hopkins Hosp 1956. PMID: 13304518
- Confalonieri M et al. Hydrocortisone Infusion for Severe community-Acquired Pneumonia: A Preliminary Randomized Study. Am J Respirated Crit Care Med 2005. PMID: 15557131
- Garcia-Vidal C et al. Effects of Systemic Steroids in Patients with Severe Community-Acquired Pneumonia. Our Respir J 2007. PMID: 17690125
- Snijders D et al. Efficacy of Corticosteroids in Community-Acquired Pneumonia: A Randomized Double-Blinded Clinical Trial. Am J Respir Crit Care Med 2010. PMID: 20133929
- Meijvis SC et al. Dexamethasone and Length of Hospital Stay in Patients with Community-Acquired Pneumonia: A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2011. PMID: 21636122
Other Blog Posts on the Topic:
- Ryan Radecki at Emergency Medicine Literature of Note



