 Patients with pulseless electrical activity (PEA) account for almost 1/3 of cardiac arrest and even more troublesome is that the survival rate is significantly worse than patients with shockable rhythms. Both the European and American ACLS guidelines stress the importance of quickly finding and addressing the cause of PEA. This is traditionally done with recalling the 5 to 6 H’s and T’s, but during cardiopulmonary resuscitation it is difficult to recall all 13 causes of PEA by trying to recall this list. In 2014 a review article was published that was developed by several departments from the Carolinas Medical Center in Charlotte, NC that tried to simplify the diagnostic approach to PEA.
Patients with pulseless electrical activity (PEA) account for almost 1/3 of cardiac arrest and even more troublesome is that the survival rate is significantly worse than patients with shockable rhythms. Both the European and American ACLS guidelines stress the importance of quickly finding and addressing the cause of PEA. This is traditionally done with recalling the 5 to 6 H’s and T’s, but during cardiopulmonary resuscitation it is difficult to recall all 13 causes of PEA by trying to recall this list. In 2014 a review article was published that was developed by several departments from the Carolinas Medical Center in Charlotte, NC that tried to simplify the diagnostic approach to PEA.
A New Simplified and Structured Method in the Evaluation and Management of Pulseless Electrical Activity
What are the traditionally taught H’s and T’s of PEA?
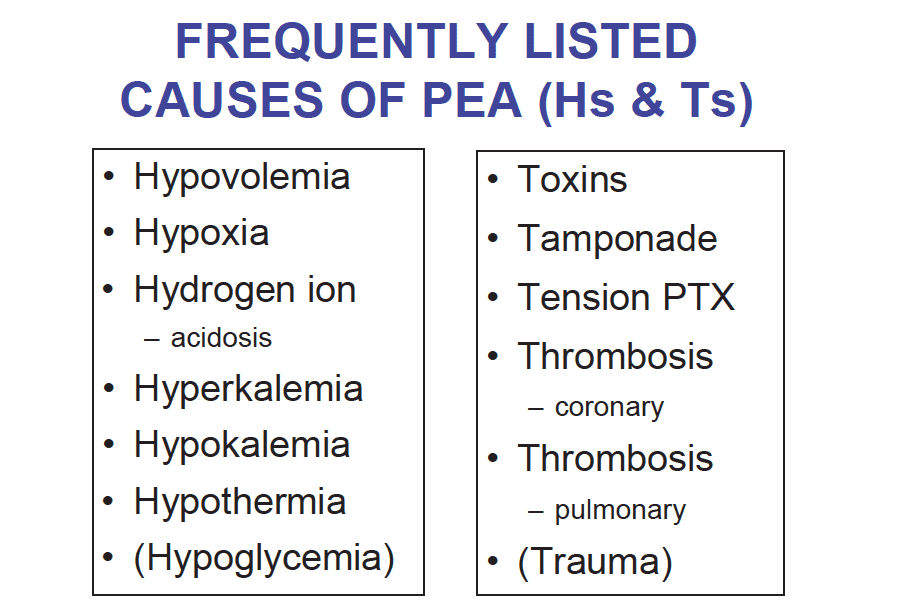
*Hypoglycemia and trauma have been removed from the most recent ACLS guidelines.
What is the new diagnostic classification of PEA?
- Step 1: Determine if the PEA is narrow (QRS duration <0.12) or wide (QRS duration ≥0.12) simply by looking at the telemetry monitor
- Step 2: Narrow-complex PEA is generally due to mechanical problems caused by right ventricular inflow or outflow obstruction
- Step 3: Wide-complex PEA is typically due to metabolic problems, or ischemia and left ventricular failure
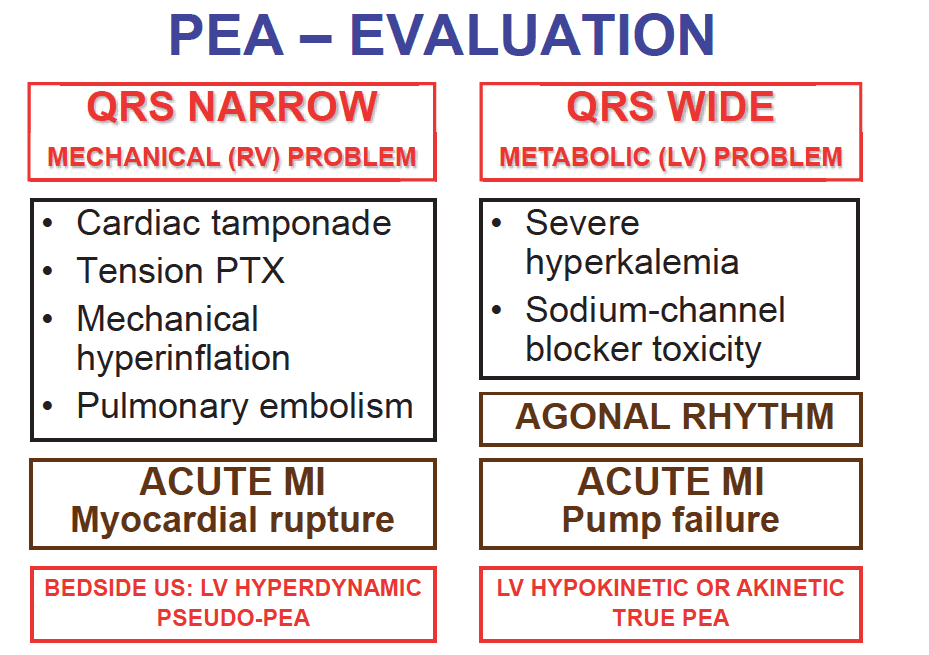
Narrow-Complex PEA
Point of care ultrasound (POCUS) can quickly aid in identification of mechanical causes of PEA. A collapsed right ventricle suggests an inflow obstruction (i.e tamponade, pneumothorax, or hyperinflation) whereas a dilated right ventricle indicates outflow obstruction (i.e. Pulmonary emobolism).
Most Common Causes:
- Cardiac Tamponade
- Tension Pneumothorax
- Mechanical Hyperinflation
- Pulmonary Embolism
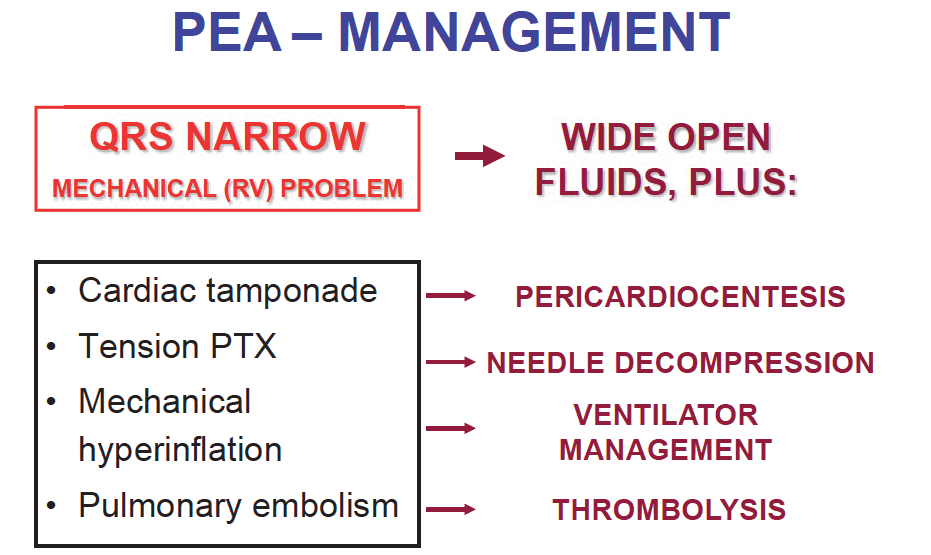
Treatment:
- Aggressive intravenous fluid administration
- Cardiac Tamponade –> Pericardiocentesis
- Tension Pneumothorax –> Needle decompression
- Mechanical Hyperinflation –> Adjust ventilator
- Pulmonary Embolism –> Thrombolytic therapy
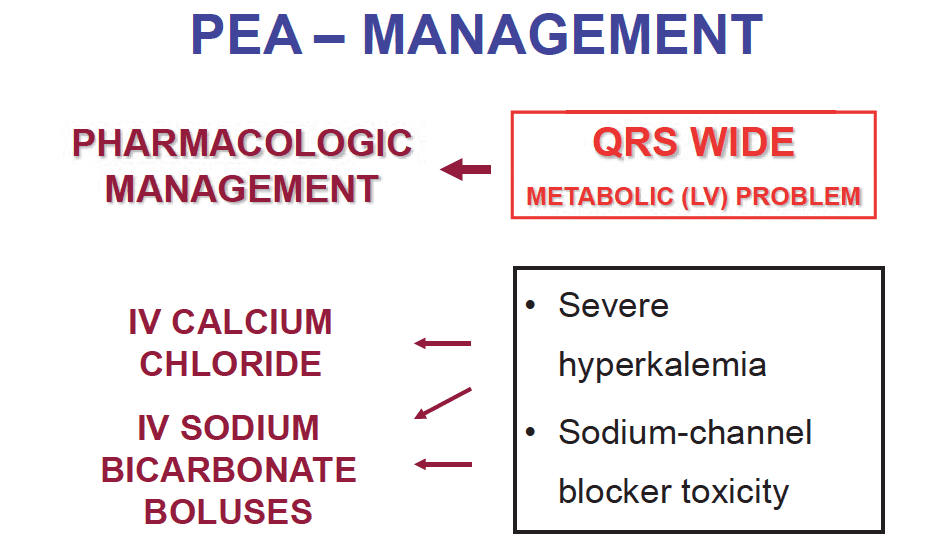
Wide-Complex PEA
This typically suggests a metabolic or toxic ingestion problem. Hyperkalemia and/or sodium channel blocker toxicity.
Treatment:
- Hyperkalemia –> Intravenous calcium chloride or gluconate
- Hyperkalemia or Sodium Channel Blocker Toxicity –> Sodium bicarbonate
Discussion:
This new classification system of PEA has 3 potential benefits compared to the traditional ACLS 5 H’s and 5 T’s
- Rather than randomly listing 10 – 13 causes of PEA by memorizing the H’s and T’s, this new algorithm categorizes the possible causes of PEA based on the easy finding of QRS complexes being narrow or wide.
- Within each category there is a marked decrease in the etiologies one has to remember and is based on the etiologies with the highest likelihood and clinical relevance.
- This algorithm also provides specific treatment recommendations that are based on the initial QRS morphology.
What are the limitations of this classification system?
- This algorithm does not apply to the trauma setting
- This algorithm has not been systematically tested for inclusiveness or resuscitation outcomes
- Narrow-complex PEA almost always indicates a mechanical cause, but occasionally mechanical causes can present with wide-complex PEA. (i.e. pre-existing bundle branch blocks, massive PE causing RBBB, and acute MI causing new LBBB)
Conclusion: Using the new classification system of PEA simplifies the working differential and initial treatment approach in conjunction with bedside ultrasound, however this strategy has not been tested systematically, tested for resuscitation outcomes, and caution should be used before implementing this algorithm until further studies are performed in the clinical setting.
For More on This Topic Checkout:
- Rory Spiegel at EM NERD: The Case of the Indiscriminate Waveform
References:
- Littmann et al. A Simplified And Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014; 23: 1 – 6. PMID: 23949188
Post Peer Reviewed by: Anand Swaminathan, MD (Twitter: @EMSwami)



