- Classically, herpes zoster will present with rash and pain in a dermatomal distribution
- Immunocompromised patients are at greater risk for significant complications of zoster, including visceral dissemination and zoster ophthalmicus
- Appropriate therapy includes antiviral therapy within 72 hours of onset of symptoms and analgesia for acute neuritis
- Disseminated zoster and zoster ophthalmicus threatening sight should be treated with IV antivirals
REBEL Core Cast 78.0 – Herpes Zoster
Click here for Direct Download of the Podcast
Definition: Reactivation of the varicella zoster virus (VZV) within sensory ganglia
- Simple herpes zoster: lesions in single dermatome without crossing the midline
- Herpes zoster ophthalmicus: Reactivation of VZV in CN V1 (ophthalmic division).
- Presents with dermatomal distribution on the face, roughly 50% of cases involve the eye (Liesegang 2008)
- Disseminated Zoster
- Rash in multiple dermatomes
- Rash crosses the midline
Epidemiology
- Affects nearly 1,000,000 people annually in U.S (Yawn 2007)
- > 30% of the U.S population will experience zoster (Harpaz 2008)
- 50% of people who live to age 85 will have an episode of Herpes zoster (Schmader 2001)
- Rates of herpes zoster have been increasing
- 1949: 0.76 per 1000 person years (Kawai 2016)
- Estimates as high as 5.2 episodes per 1000 person years in 2007 (Rimland 2010)
- More prevalent in females, incidence increases with age in both sexes (Kawai 2016)
- Risk Factors
- Age
- Immunocompromised status – including transplant patients, HIV infected patients, and those with underlying malignancy
- Physical Trauma
- Chronic lung or kidney disease
Pathophysiology
- Reactivation of latent varicella-zoster virus (VZV) in dorsal root ganglia
- Reactivation of VZV results in inflammation of dorsal spinal ganglia, resulting in dermatomal distribution of pain and vesicular rash
Presentation
- History
- Previous diagnosis of chickenpox
- Dermatomal pain and pruritus up to 5 days prior to the development of skin lesions
-
-
- Pain quality may be variable in presentation – aching, burning, or stab-like
-
-
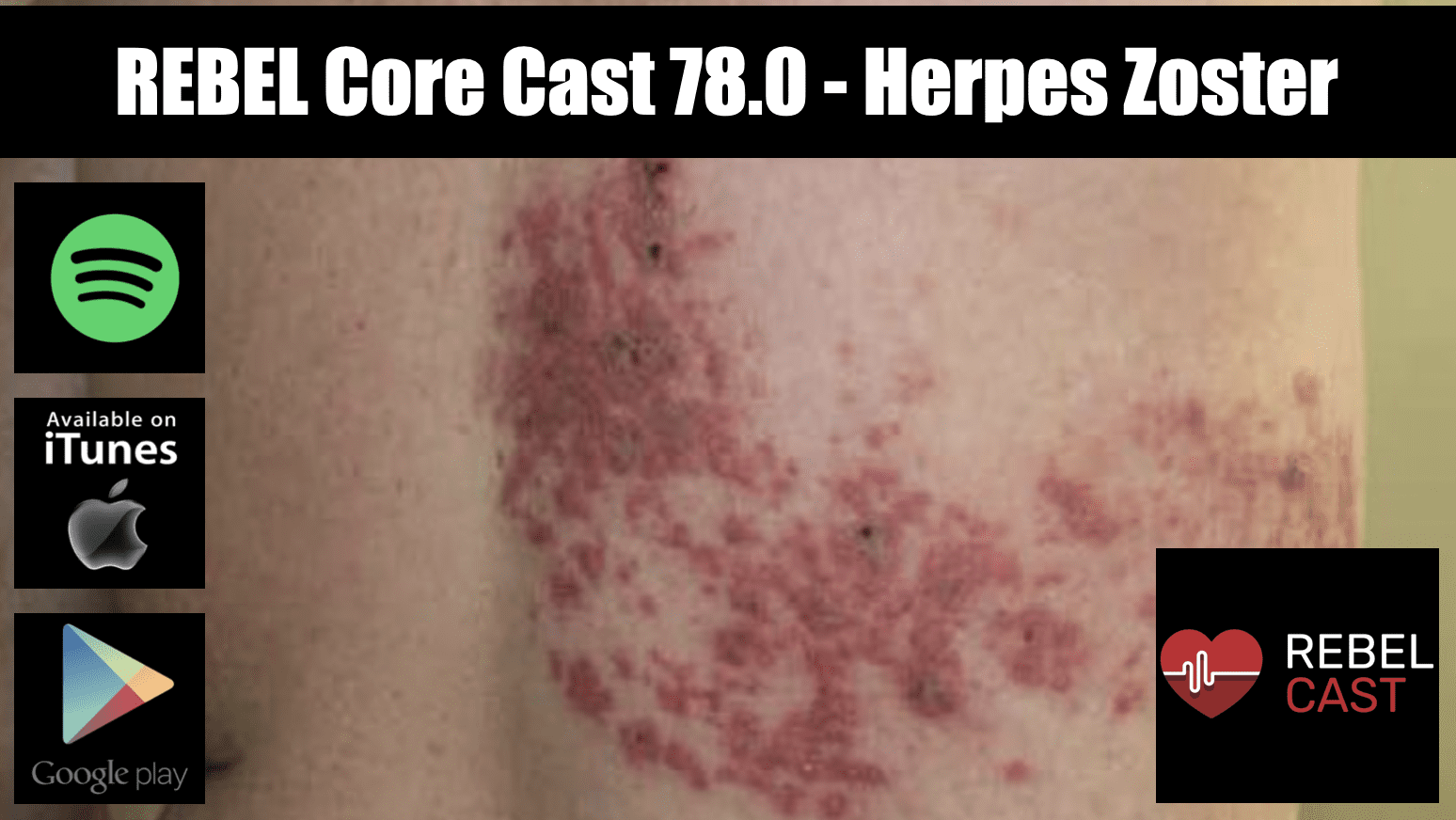
- Physical Exam
- Rash in dermatomal pattern, typically on trunk
- Rash is erythematous, typically with a macular base and clear vesicles that progress to scab and crust formation.
- Formation of scabs takes 10-12 days
- Heals within 2-4 weeks
- Other physical exam findings such as lung crackles, hepatomegaly, and neurologic deficits may indicate visceral involvement following cutaneous dissemination
Differential
- Primary varicella infection
- Herpes simplex infection
- Burn
- Contact Dermatitis
- Insect bites
- Impetigo
- Dermatitis herpetiformis
Management of herpes zoster
- Initiation of antiviral therapy should occur within 72 hours of onset
- Antiviral therapy
- Increased rate of healing of skin lesions
- May reduce acute neuritis
- May help prevent postherpetic neuralgia
- If new lesions continue to appear antiviral therapy is recommended, even past 72 hours from onset
- Choice of antiviral therapy
- Valaciclovir 1000mg PO Q8 x 7 days
- Famciclovir 500mg PO Q8 x 7 days
- Acyclovir 800mg PO five times daily x 7 days
- Intravenous therapy indicated for:
- Disseminated zoster
- Zoster ophthalmicus with ocular involvement
- Inability to tolerate oral medications
- Antiviral therapy
- Analgesia may be needed for the management of acute neuritis
- First line choices include NSAIDs and acetaminophen
- For moderate to severe pain, opioid analgesic may be needed
- Treatment for immunocompromised patient
- Should be treated regardless of time from onset of lesions
- If disseminated or involves more than one dermatome IV acyclovir should be used for treatment
- Patients with active lesions should be counseled to avoid patients who are immunocompromised and pregnant women to avoid transmission
Complications
- Postherpetic neuralgia – most common complication and occurs in up to 15% of patients. Incidence increases with age
- Bacterial skin infection – secondary infection due to open skin lesion
- Ocular complications, including keratitis and vision loss
- Disseminated herpes zoster – herpes zoster that is not confined to dorsal root ganglia
- More common in immunocompromised patients
- Cutaneous dissemination may progress to visceral organ involvement, resulting in pneumonia, hepatitis, or encephalitis. Visceral dissemination may be life threatening
Disposition
- Most patients are suitable for outpatient management with oral antiviral agents and analgesia
- Indications for admission:
- Disseminated zoster
- Immunosuppressed state (HIV, diabetes, chemotherapy)
- Zoster requiring IV antiviral therapy or analgesic control
Take Home Points
- Classically, herpes zoster will present with rash and pain in a dermatomal distribution
- Immunocompromised patients are at greater risk for significant complications of zoster, including visceral dissemination and zoster ophthalmicus
- Appropriate therapy includes antiviral therapy within 72 hours of onset of symptoms and analgesia for acute neuritis
- Disseminated zoster and zoster ophthalmicus threatening sight should be treated with IV antivirals
Read More
- Emergency Medicine Ireland: Tasty Morsels of EM 073: FRCEM Varicella
- Life in the Fast Lane: Herpes zoster ophthalmicus
- Up to Date: Treatment of herpes zoster in the immunocompetent host
- Concise Review for Clinicians – Herpes Zoster (Shingles) and Postherpetic Neuralgia
- Marco CA: Dermatologic Presentations, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 110: p 1430-1454.
References
- Liesegang TJ. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology. 2008 Feb;115(2 Suppl):S3-12. PMID: 18243930
- Yawn BP et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007; 82(11): 1341-9. PMID: 17976353
- Harpaz R et al. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008 Jun 6;57(RR-5):1-30; quiz CE2-4. PMID: 18528318
- Schmader K. Herpes zoster in older adults. Clin Infect Dis. 2001 May 15;32(10):1481-6. PMID: 11317250
- Kawai et al. Increasing incidence of herpes zoster over a 60-year period from a population-based study. Clin Infect Dis. 2016 Jul 15;63(2):221-6. PMID: 27161774
- Rimland et al. Increasing incidence of herpes zoster among Veterans. Clin Infect Dis. 2010 Apr 1;50(7):1000-5. PMID: 20178416
Post Created By: Alex Estrella, MD
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
Cite this article as: Anand Swaminathan, "REBEL Core Cast 78.0 – Herpes Zoster", REBEL EM blog, April 6, 2022. Available at: https://rebelem.com/rebel-core-cast-78-0-herpes-zoster/.