What Article are we Discussing?
Bischof JE et al. ST Depression in Lead aVL Differentiates Inferior ST-Elevation Myocardial Infarction from Pericarditis. AJEM 2015 [Epub Ahead of Print] PMID: 26542793
What They Did:
- Single Center, Retrospective Cohort Study:
- Cohort 1: Patients coded as Inferior STEMI
- Cohort 2: Patients coded as Pericarditis and chest pain + at least 0.5mm of ST-elevation in at least 1 inferior lead
- Cohort 3: Patients with subtle Inferior STEMI (<1mm STE with occluded artery on catheterization)
- Assess the sensitivity and specificity of ST depression in lead aVL in distinguishing between the diagnosis of Inferior STEMI vs Pericarditis
- Assess the incidence of ST depression in lead aVL in “subtle cases” (i.e. NO STE >1mm) in inferior leads
Outcomes:
- Primary: Presence or absence of any ST depression in lead aVL in patients with inferior STE due to STEMI vs pericarditis
- Secondary:
- Presence of T-wave inversion in aVL
- Comparisons of relative ST elevation in leads II and III
- Whether or not ECG met reperfusion criteria
- Sensitivity of any ST depression in aVL for inferior MI among those who do not meet STEMI criteria
Results:
- In Cohort 1 (Inferior STEMI Cohort):
- 154/154 (100%) had some amount of ST depression in lead aVL
- Sensitivity 100% [CI 98% – 100%]
- 154/154 (100%) had t-wave inversions in lead aVL
- Sensitivity 100% [CI 98% – 100%]
- 135/154 (88%) had RCA Occlusion
- 136/154 (88%) had ST elevation in lead III > lead II
- 154/154 (100%) had some amount of ST depression in lead aVL
- In Cohort 2 (Pericarditis Cohort):
- 49/49 (100%) had some inferior STE but NONE had any ST-segment depression lead aVL
- ST-segment elevation in lead II was ≥ lead III in 49/49 (100%) of cases [CI 93% – 100%]
- In Cohort 3 (Confirmed Inferior STEMI Cohort):
- 218 were obvious STEMIs and 54 were considered “subtle” (≤1mm of STE). In the “subtle cases,” 49/54 had some ST depression in lead aVL
- Sensitivity 98.8% [95% CI 97.3% – 99.5%]
- QTc Interval Comparison:
- Inferior STEMI groups were significantly longer than pericarditis group (Difference of 26.2msec).
- QTc >450msec had good specificity but poor sensitivity for differentiating inferior STEMI from pericarditis
- 43/154 inferior STEMI pts had QTc >450msec (sensitivity 28%)
- 2/49 pericarditis patients had values greater than 450msec (specificity 96%)
- 218 were obvious STEMIs and 54 were considered “subtle” (≤1mm of STE). In the “subtle cases,” 49/54 had some ST depression in lead aVL
Strengths:
- ECGs were evaluated by 3 authors blinded to outcome
- ECGs were evaluated manually at the J point to the nearest 0.25mm in leads II, III, aVF, and aVL for STE or depression
Limitations:
- This was a retrospective medical record chart review, therefore making the study limited by the data that was or wasn’t recorded. This may cause the true number of acute inferior MIs to be underestimated which could affect sensitivity of lead aVL for inferior MI
- In the confirmed STEMI cohort, the lack of data in the “obvious” STEMI group is a limitation to this study, not allowing evaluation of this cohort
- Incidence of confirmed pericarditis was quite low.
- Relied on ICD-9 codes for identification of subjects, which may have missed some cases of clinical pericarditis not coded as such
- Because this was not a consecutive patient study, PPV and NPV could not be calculated.
- Medical record search was for “STEMI” which would exclude those patients who “rule in” by biomarkers and have coronary occlusion on subsequent catheterization.
Discussion:
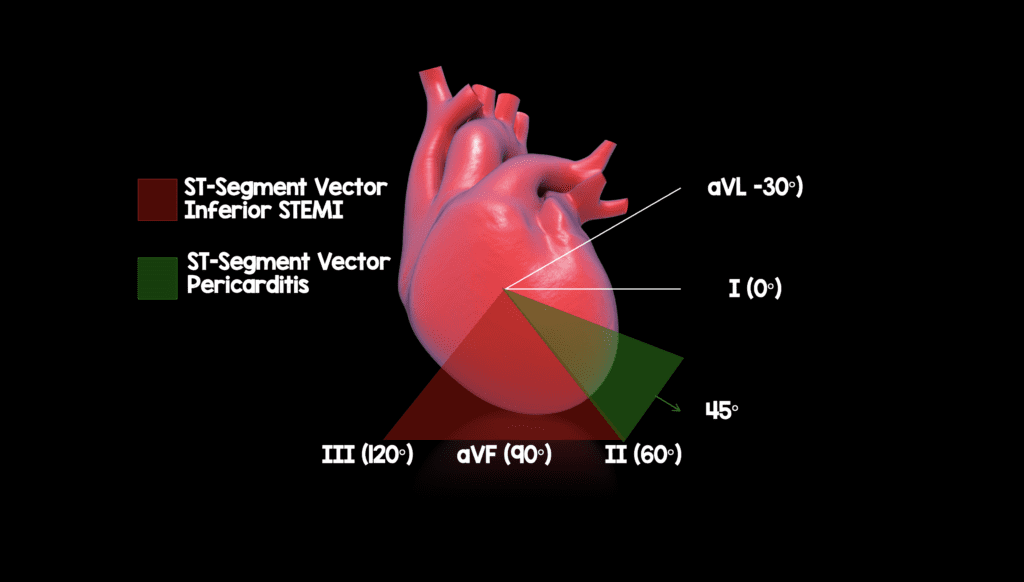
- Typically the vector of ST elevation in inferior STEMI is between 60° and 120° (between leads II and III). This is a difference of 90° to 150° from lead aVL (-30°) and should result in some reciprocal ST-segment depression in lead aVL.
- Pericarditis on the other hand is diffuse inflammation of the entire pericardium, resulting in a ST axis of approximately 45° (apex of the heart). This is a difference of 75° to lead aVL (-30°) and should not result in reciprocal ST-segment depression in lead aVL.
Author Conclusion: “When there is inferior ST-segment elevation, the presence of any ST depression in lead aVL is highly sensitive for coronary occlusion in inferior myocardial infarction and very specific for differentiating inferior myocardial infarction from pericarditis.”
Clinical Take Home Point: In the presence of inferior STE, look at lead aVL next. If there is ST depression in lead aVL, treat the patient for inferior myocardial infarction due to coronary occlusion and not as pericarditis.
References:
- Bischof JE et al. ST Depression in Lead aVL Differentiates Inferior ST-Elevation Myocardial Infarction from Pericarditis. AJEM 2015 [Epub Ahead of Print] PMID: 26542793
Post Peer Reviewed By: Matt Astin (Twitter: @mastinmd)



