Background: A patient presents to the emergency department (ED) for medical treatment. After comprehensive evaluation and management, the patient’s condition improves and you prepare to discharge the patient home. The nurse notifies you the blood pressure (BP) is 185/105 and asks if you are comfortable discharging the patient in light of the abnormal vital signs.
Background: A patient presents to the emergency department (ED) for medical treatment. After comprehensive evaluation and management, the patient’s condition improves and you prepare to discharge the patient home. The nurse notifies you the blood pressure (BP) is 185/105 and asks if you are comfortable discharging the patient in light of the abnormal vital signs.
This clinical scenario happens regularly in the ED. Our training in emergency medicine has always been: “We do not treat asymptomatic hypertension in the ED.” In fact, ACEP’s 2013 Clinical Policy statement recommends referring patients with asymptomatic hypertension for outpatient follow-up and NOT starting antihypertensive therapy in the ED. However, this tends to be a controversial topic with various clinical opinions and practices. Ask ten emergency medicine physicians: What BP value would make you uncomfortable when discharging a patient? You may get ten different answers.
Patient safety is paramount. Furthermore, individual physicians have varying levels of risk tolerance and aversion which contribute to treatment decisions. This paper attempts to address concerns in patients with elevated blood pressure readings in the ED.
Paper: McAlister FA et al. Elevated Blood Pressures Are Common in the Emergency Department but Are They Important? A Retrospective Cohort Study of 30,278 Adults. Ann Emerg Med 2021. PMID: 33579586
Clinical Question: Is there an association between ED blood pressure levels and cardiovascular events in the subsequent 2 years?
What They Did:
- A retrospective cohort study using electronic medical records (EMR) for all adults treated and discharged from the University of Alberta Hospital
- Tertiary Care ED
- 75,000 visits annually
- Patient visits linked to administrative records for all health care encounters in the province 2 years before and after ED visit
- Interrogated national database linked to the hospital for one year (January 1 – December 31, 2016)
- Determine the distribution of triage BPs
- Split into 3 groups based on BP
- (140–159)/(90–99)
- (160–179/(100–109)
- ≥ 180/110
Inclusion / Exclusion:
- Included all adult patients ≥ 18 years of age
- Excluded patients with diagnosis:
- Acute Stroke
- Cerebral Contusion
- Intracerebral Hemorrhage
- Anaphylaxis
- Excluded Dispositions:
- Died in ED
- Left against medical advice
- Admitted
- Transferred to another hospital
- Only first visits for patients with multiple visits
Outcomes:
- Primary: Any hospitalization in subsequent 2 years for:
- Composite outcome of stroke, transient ischemic attack (TIA), heart failure, acute coronary syndrome, death
- Secondary:
- Composite of death, stroke, or TIA
- Acute coronary syndrome
- New heart failure
Results:
- 30,278 patient data analyzed:
- 14,717 (48.6%) had elevated BP readings
- 10,732 (72.9%) did not have a prior diagnosis of hypertension
- Patient with BP ≥ 140/90 more likely:
- Older
- Men
- Lower acuity in Canadian Triage and Acuity Scale (less urgent complaints)
- Prior history of hypertension, diabetes, or CAD
All Patients with elevated BP (14,717)
- 70.4% were treated in outpatient follow up within one month
- 31.4% were prescribed antihypertensive medications within 90 d of discharge
Patients without history of hypertension with elevated BP (10,732)
- 65.8% were treated in outpatient follow up within one month
- 13.9% were prescribed a new antihypertensive medications within 90 d of discharge
In patients with BP ≥160/100
- 67.5% were treated in outpatient follow up within one month
- 25.0% were prescribed a new antihypertensive medication within 90d of discharge
- 26.1% were diagnosed with chronic hypertension or prescribed antihypertensive therapy in other clinical settings within 2 years
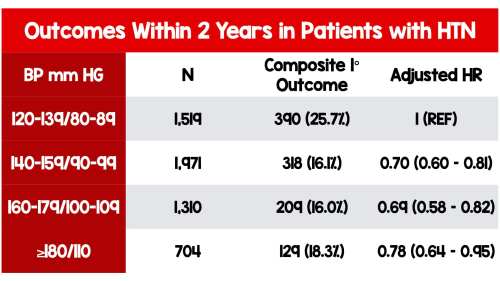
- More likely than BP group (120–139)/(80–89) to meet composite outcome of stroke, transient ischemic attack (TIA), heart failure, acute coronary syndrome, death:
- Subsequent 1 year: 3.3% vs 2.5%
- Subsequent 2 years: 5.9% vs 3.8%
- NO STATISTICALLY SIGNIFICANT ELEVATION IN RISK when adjusted for age, sex, diabetes, atrial fibrillation, and prior cardiovascular disease

Patients with history of hypertension with elevated BP
- Higher rates of death stroke, acute coronary syndrome, and heart failure in all groups than patients without a diagnosis of hypertension who presented in the same BP range
- NO STATISTICALLY SIGNIFICANT ELEVATION IN RISK when adjusted for age, sex, diabetes, atrial fibrillation, and prior cardiovascular disease
Strengths:
- Large heterogeneous group of ED patients
- Used a reliable comprehensive national data registry to obtain data
- Primary and secondary outcomes were patient-oriented
- Inclusion criteria were broad
Limitations:
- Single-center, urban, tertiary care ED, Canadian study
- Canada has universal healthcare not present in the US and therefore may not reflect all clinical practice
- Used single BP reading taken at triage which may not account for false readings both high and low
- Primary endpoint was a composite
- All components are not equal and the spectrum is broad
- Death is not equal to angina or TIA
- All components are not equal and the spectrum is broad
- Excluded admitted patients (17,176)
- Why were these patients admitted?
- It’s possible physicians admitted patients who were “really high” beyond the physician’s risk threshold or those without follow up and comorbidities
- If patient’s at risk for bad outcome (determined by gestalt) were admitted this could bias the results
- Did not mention patient’s lost to follow up
- We don’t know how many patients who did not follow up in 30 days never followed up at all
- We assume that if there was a major cardiovascular event that these patients would have been captured in the database, but this doesn’t account for patients who may have moved, died in another country or died as a “John Doe” probably a small number but worth mentioning
- This is an observational study that cannot account for all confounders
- Did not include data on antihypertensive medication
- Did not assess medical advice and lifestyle modification recommendations
Discussion:
- Though this was a single-center study in Canada, the wide inclusion criteria and large sample size render this study broadly applicable
- We are compelled to mention universal healthcare coverage in Canada. Access to medications and outpatient follow-up may not reflect all clinical practice.
- This is important because it’s easier to discharge patients with elevated blood pressure (even markedly elevated) if we believe they will have access to proper follow-up and long term care
- We are more cautious with patients who are under-insured and uninsured than in comparable groups of patients with good insurance and good outpatient follow up
- This paper adds to the growing body of evidence on the topic and demonstrated concretely there was no short term increase risk in cardiovascular events in patients with elevated BP in the ED
Author’s Conclusion: “Although elevated BP at triage is associated with poorer cardiovascular outcomes in the subsequent 2 years, that excess risk appears to be due patients’ age, sex, and comorbidities, and there is no independent association between BP readings and short-term prognosis.”
Clinical Bottom Line:
We agree with the author’s conclusion and also support the ACEP position. In patients presenting to the ED found to have asymptomatic hypertension, focus efforts on timely outpatient referral and follow-up; not on acute lowering of their blood pressure.
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)