“In IHCA, the combination of Vasopressin, Epinephrine, and Methylprednisolone and post-arrest Hydrocortisone as described by Mentzelopoulos et al. maybe considered; however, further studies are needed before recommending the routine use of this strategy (Class IIb, LOE C-LD)”
Mentzelopoulos et al. [2][3] have published two separate randomized, double-blind, placebo-controlled studies out of Greece examining the role of this Vasopressin, Steroid, and Epinephrine (VSE) cocktail. These studies looked at in-hospital cardiac arrest for patients and enrolled patients immediately with non-shockable rhythms or patients in refractory VFib/VTach. The first study included 100 patients from a single center, while the second study included 268 patients from multiple centers.
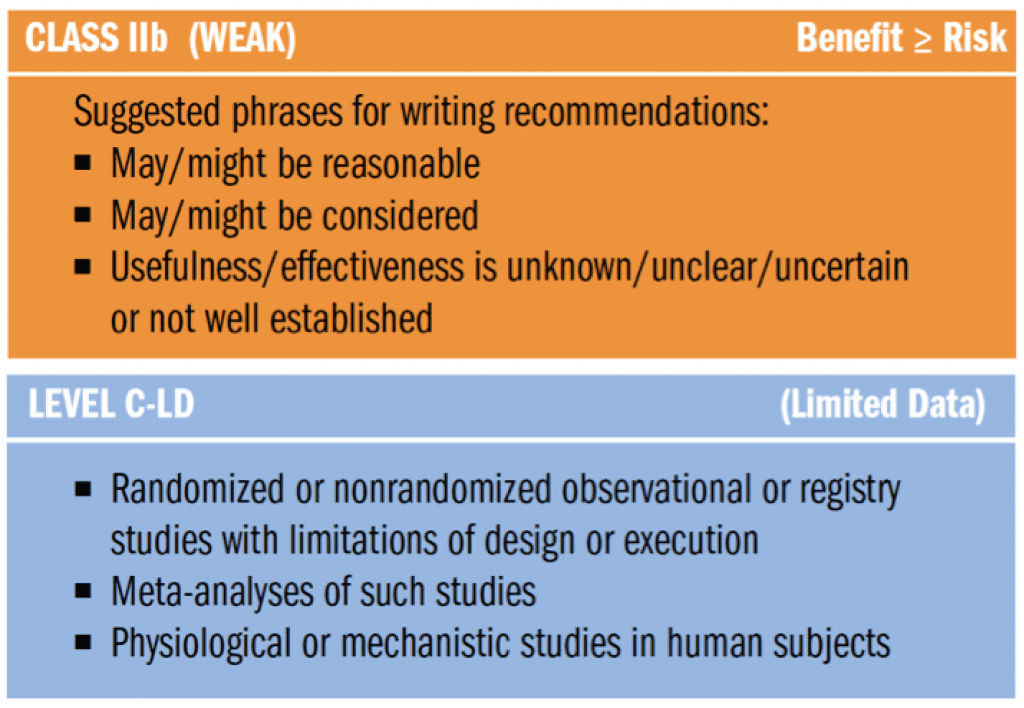
First, What does ClassIIb, LOE C-LD Mean in the New 2015 AHA Guidelines?
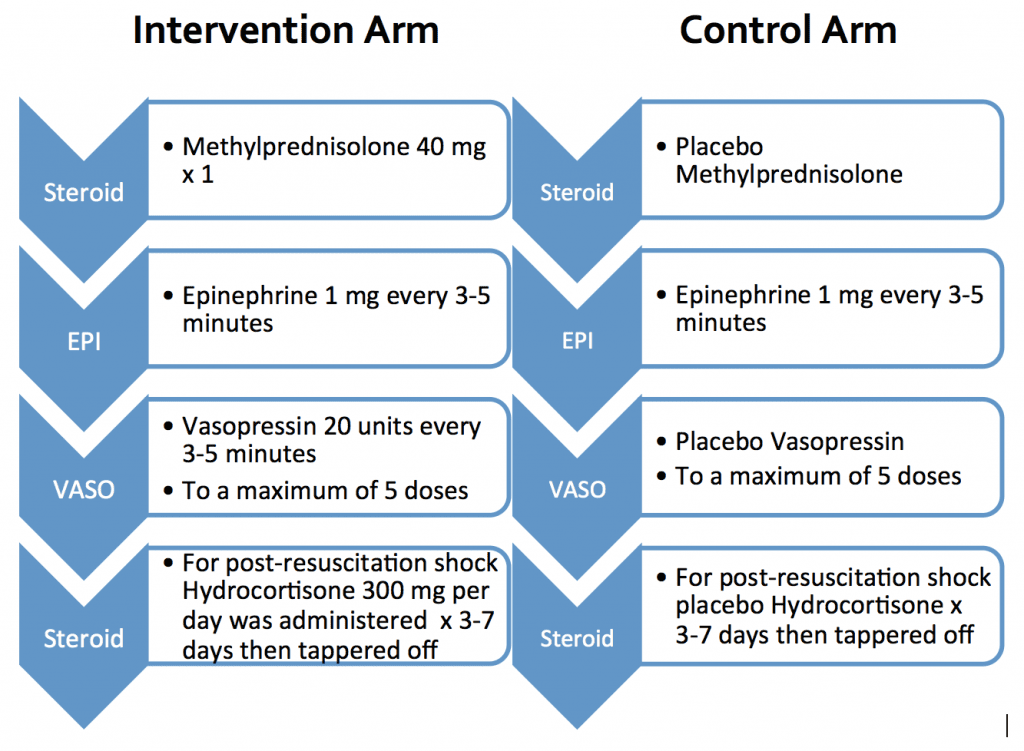
What Were the Intervention & Control Arms?
The results demonstrate an increase in Return of Spontaneous Circulation (ROSC), an increase in survival to hospital discharge with a NNT = 7 [2], and an increase in neurologically favorable survival to hospital discharge with a NNT = 12 [3].
More Detailed Results:
Mentzelopoulos et al. 2009 [2]
- VSE
- n=100
- Increase ROSC: 39/48 (81%) vs. 27/52 (52%) p=0.003
- Increase Survival to Discharge: 9/48 (19%) vs. 2/52 (4%) p=0.02
- Following ROSC: Increase MAP, Decrease Vasopressor Requirements, Decrease Cytokine Levels, Increase Central Venous Oxygen Saturation, Decrease Lactate, Increase Renal-Failure Free Days
- Stress Dose Steroids
- Increase Hospital Discharge 8/27 (30%) vs. 0/15 (0%) p=0.02
- Increase Organ Failure Free Days
- No Difference in Incidence of Adverse Effects due to Steroids Noted
Mentzelopoulos et al. 2013 [3]
- VSE
- n=268
- Increase ROSC: 109/130 (84%) vs. 91/138 (66%) p=0.005
- Increase Discharge with CPC Score 1 or 2: 18/130 (14%) vs. 7/138 (5%) p=0.02
- Decrease Duration ACLS, Total Epinephrine Dose, and Organ Dysfunction
- Increase Hemodynamics, Central Venous Oxygen Saturation, Cerebral Perfusion Pressure, and Renal-, Neurologic-, Ventilator-Failure Free Days
- Similar Adverse Effects
- Stress Dose Steroids:
- Increase Discharge with CPC Score of 1 or 2: 16/76 (21%) vs. 6/73 (8%) p=0.02
- 15 Epi Patients Received Hydrocortisone
- Increase Circulatory-, Renal-, Hepatic-, Coagulation-, Respiratory-Failure Free Days
- No Difference in Incidence of Adverse Effects due to Steroids Noted
Physiologic Rationale Behind VSE
Benefits in ROSC are likely due to the combination of Vasopressin and Epinephrine

Combination of Vasopressin and Epinephrine
- Has not shown a survival benefit overall
- Studies were all conducted in the out-of-hospital cardiac arrest setting
- Have many inherent limitations including delays in initiation of basic life support and delays in time to vasopressor therapy
- Largest Epinephrine and Vasopressin Combination Study [4] was associated with:
- Time to arrival of emergency medical technicians was ~7 minutes
- Time to arrival of the advanced cardiac life support team was ~16 minutes
- Time to the first vasopressor administration was ~21 minutes
- Delays in administration of vasopressors (specifically epinephrine) have been associated with worse outcomes

Epinephrine and Vasopressin Alone
- Have both been associated with increased rates of ROSC
- Vasopressin is an endogenous peptide and antidiuretic hormone which increases peripheral vascular resistance through stimulation of smooth muscle V1 receptors
- Increase in coronary perfusion pressure, cerebral vasodilation, minimal effects on pulmonary vasculature, a longer half-life and duration of effect than epinephrine
- Potentiates release of cortisol and has a greater stability in acidic environments compared to catecholamines
- Epinephrine is a potent catecholamine with alpha and beta agonist effects:
- Alpha effects result in vasoconstriction
- Increased coronary perfusion pressure which may be responsible for the increased ROSC rates
- Increased cerebral perfusion pressure
- Animal data suggests this may not be as beneficial as previously thought due to a decrease in microcirculatory cerebral blood flow and ischemia during CPR
- Beta effects are more controversial
- Increased myocardial work, oxygen and ATP consumption, lactic acid production, secondary VFib, pulmonary arteriovenous shunting resulting in transient hypoxemia, and post ROSC myocardial dysfunction
- Alpha effects result in vasoconstriction

Neurologically Favorable Survival
- Likely due to steroid attenuation of post-resuscitation complications
- Adrenal Insufficiency of Cardiac Arrest
- Adrenal gland ischemia
- Associated with increased mortality, hemodynamic instability, and diminished response to catecholamines
- Inflammatory Mediated Ischemic/Reperfusion Injury
- Activation of the inflammatory cascade after cardiac arrest due to injury from ischemia
- Further damages ischemic organs and can compound neurologic damage
- Physiologic response to cytokines is release of cortisol
- Blunted due to adrenal insufficiency
- Elevated cytokine levels have been associated with increased mortality and unfavorable neurologic outcomes
- Post-Resuscitation Shock
- Associated with myocardial stunning and decreased cardiac index
- May lead to multi-system organ dysfunction (may also decrease cerebral blood flow and compound neurologic damage) and may progress to mortality
- Risk factors associated with post-resuscitation shock include: >15 minute duration of code, more frequent doses of epinephrine, greater number of defibrillation attempts
- Associated with myocardial stunning and decreased cardiac index
- Steroids Attenuate Post-Resuscitation Complications
- Steroids help decrease inflammatory response and regulate homeostasis by regulating gene expression
- Physiologic effects include: positive inotropy, anti-inflammatory effects which counter ischemic reperfusion injury (decrease neurologic damage), decrease vascular permeability/increase vascular reactivity to catecholamines and angiotensin II which increase systemic vascular resistance (increased cerebral perfusion), supplements cortisol which may not be sufficiently produced due to adrenal insufficiency
- Takes ~30 minutes to a few hours to produce physiologic effects
- Potential side effects include electrolyte disturbances, risk of infections, and negative regulation on the HPA axis
- Not demonstrated in studies; however, not powered to determine difference
- Higher cortisol plasma concentrations have been associated with increased neurologically intact survival
- Steroids help decrease inflammatory response and regulate homeostasis by regulating gene expression
Clinical Bottom Line
- The VSE cocktail increases neurologically favorable survival to hospital discharge for IHCA with a NNT = 12
- Prior investigations of vasopressin and epinephrine should be interpreted cautiously due to delays in initiation to basic life support and time to vasopressor therapy
- Early administration of steroids attenuates complications of post-resuscitation care such as inflammatory mediated ischemic/reperfusion injury, post-resuscitation shock, and adrenal insufficiency
Guest Post By:
Hannah Davis, PharmD
PGY2 Emergency Medicine Pharmacy Resident
University of Texas Health Science Center at San Antonio/University Health Systems
References
- Link M, Berkow L, Kudenchuk P, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015;132:S444-644. [Table of Contents]
- Mentzelopoulos S, Zakynthinos S, Tzoufi M, et al. Vasopressin, epinephrine, and corticosteroids for in-hospital cardiac arrest. Arch Intern Med 2009;169:15-24. PMID: 19139319
- Mentzelopoulos S, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: a randomized clinical trial. JAMA. 2013;310(3):270-9. PMID: 19139319
- Gueugniaud P, David J, Chanzy E, et al. Vasopressin and epinephrine vs. epinephrine alone in cardiopulmonary resuscitation. New Engl J Med. 2008;359(1):21-30. PMID: 23860985
- Varvarousi G, Stefaniotou A, Varavaroussis D, et al. Glucocorticoids as an emergency pharmacologic agent for cardiopulmonary resuscitation. Cardiovasc Drugs Ther. 2014;28:477-88. PMCID: PMC4163188
For More on This Topic Checkout:
- David Slessor at The Bottom Line: VSE – Vasopressin, Steroids, and Epinephrine and Neurologically Favorable Survival After In-Hospital Cardiac Arrest A Randomized Clinical Trial
- Thomas D at ScanCrit: CPR on Steroids
- Josh Farkas at PulmCrit: 2015 ACLS Guidelines – What Happened to VSE?
- Craig Cocchio at Emergency Medicine PharmD: Vanishing Vasopressin
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)