 Background: As with all medications in cardiac arrest (i.e. epinephrine, amiodarone) the benefits of sodium bicarbonate administration have been discussed and debated for decades. While it is clear that sodium bicarbonate can play a role in resuscitation of arrest due to hyperkalemia, it’s role in patients with acidemia resulting from or causing arrest is unclear. In theory, raising the pH may be beneficial but the use of bicarbonate increases serum CO2 which may be deleterious as it creates a respiratory acidosis. Despite the absence of good evidence, sodium bicarbonate continues to be used in non-hyperkalemic cardiac arrest management.
Background: As with all medications in cardiac arrest (i.e. epinephrine, amiodarone) the benefits of sodium bicarbonate administration have been discussed and debated for decades. While it is clear that sodium bicarbonate can play a role in resuscitation of arrest due to hyperkalemia, it’s role in patients with acidemia resulting from or causing arrest is unclear. In theory, raising the pH may be beneficial but the use of bicarbonate increases serum CO2 which may be deleterious as it creates a respiratory acidosis. Despite the absence of good evidence, sodium bicarbonate continues to be used in non-hyperkalemic cardiac arrest management.
Article: Ahn, S et al. Sodium bicarbonate on severe metabolic acidosis during prolonged cardiopulmonary resuscitation: a double-blind, randomized, placebo-controlled pilot study. J Thorac Dis 2018; 104(4): 2295-2302. [Epub Ahead of Print]
Clinical Question:
In patients with prolonged, non-traumatic, cardiac arrest resulting in acidosis, does the administration of sodium bicarbonate lead to a higher rate of sustained ROSC?
Population: Patients that failed to achieve ROSC after 10 minutes of standard ACLS and a femoral ABG demonstrating pH < 7.1 or bicarbonate < 10 mEq/L
Intervention: Sodium Bicarbonate (NaHCO3) 50 mEq/L
Control: Normal Saline (NS) 50 ml
Outcomes:
- Primary: Sustained ROSC (palpable pulse > 20 minutes) and change in pH (abstract states sustained ROSC, methods section states change in pH)
- Secondary: Survival to hospital admission, good neurologic survival at 1 and 6 months (CPC 1 – 2)
Design: Prospective, double-blind, randomized, placebo-controlled, single-center pilot trial
Excluded: Patients with DNR orders, ROSC within 10 minutes, unavailable ABG at 10 minutes, no severe acidosis on 10 minute ABG or eCPR started.
Primary Results:
- 157 patients presented during the enrollment period with cardiac arrest
- 50 patients were randomized to NaHCO3 or NS
- 107 were excluded for the reasons noted above
- Sustained ROSC (> 20 minutes): 10%
- No patients survived at 6 months (this was a very sick subset of cardiac arrest patients)
- Baseline characteristics were similar between groups
Critical Results:
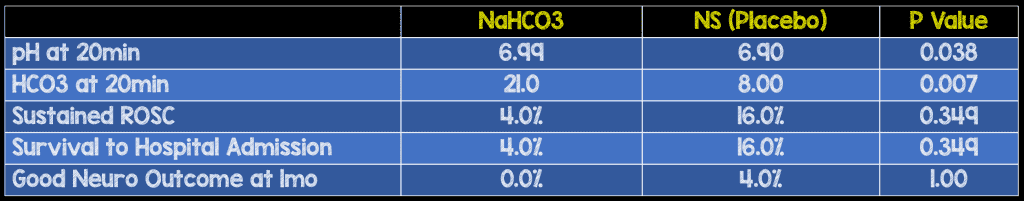
- Change in acidosis
- Statistically significant difference in both pH and HCO3 between groups
- pH at 20 minutes 6.99 (NaHCO3) vs 6.90 (NS) p = 0.038
- HCO3 21.0 (NaHCO3) vs 8.00 (NS) p = 0.007
- Sustained ROSC
- No statistically significant difference
- 4.0% (NaHCO3) vs 16% (NS) p = 0.349
- Survival to hospital admission
- No statistically significant difference
- 4.0% (NaHCO3) vs 16% (NS) p = 0.349
- Good neurologic outcome at 1 month
- No statistically significant difference
- 0.0% (NaHCO3) vs 4% (NS)
Strengths:
- Sound methodology to attempt to answer the question: randomized, double-blinded, placebo-controlled
- Adds information to a question with limited previous research
- Incorporated intervention to balance out accumulation of CO2 secondary to bicarbonate use (increasing ventilation to 20 breaths/minute after administration)
Limitations:
- Small, single center study
- Unclear what the primary endpoint was (stated as sustained ROSC in the abstract but as change in acid-base status in body of study)
- Neither primary endpoint was patient centered. Would prefer to see good neurologic outcome as the primary outcome in subsequent studies
- Bicarbonate dose was fixed instead of weight based. This may have led to both under and over-dosing of bicarbonate. A dose of 1-2 mEq/kg may have been more appropriate.
- Blood samples for 10 minute analysis may have been venous instead of arterial which may depress the pH and bicarbonate values
- Hyperventilation may have benefited group receiving NaHCO3 (by countering respiratory alkalosis) but may have harmed group receiving NS
- Quality of CPR, and time to defibrillation not included, both of which can be confounding factors
- ROSC definition was a palpable pulse. Would argue this is not the gold standard: TTE, TEE, A-Line, EtCO2 much more sensitive and some profound shock patients may have erroneously been included in the no ROSC group
- Although not mentioned as statistically significant..more patients in the placebo arm had a shockable rhythm than patients in the bicarb arm (8.0% – 2pts vs 0% – 0pts)
Other Issues:
- All patients ventilatory rate was increased from 10 to 20 breaths per minute for 2 minutes after administration of NaHCO3 or NS to counteract the increase CO2 produced by NaHCO3
Author’s Conclusions:
“The use of sodium bicarbonate improved acid-base status, but did not improve the rate of ROSC and good neurologic survival. We could not draw a conclusion, but our pilot data could be used to design a larger trial to verify the efficacy of sodium bicarbonate.”
Our Conclusion:
We agree with the authors conclusions. While the use of NaHCO3 improved the surrogate endpoint of acid-base status, there was no patient centered improvement seen in this study.
Potential to Impact Current Practice:
This small pilot study should not change clinical practice. Indiscriminate use of NaHCO3 in cardiac arrest should not be performed. However, providers should continue to use their judgement as to which patients with arrest may benefit from NaHCO3.
Bottom Line:
The use of NaHCO3 does not appear to improve clinically meaningful outcomes. A larger study should be undertaken to further evaluate this clinical question.
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)



