 Background: Vasopressors are frequently used in critically ill patients with hemodynamic instability both in the emergency department (ED) as well as intensive care units (ICUs). Typically, vasopressors are given through central venous catheters (CVCs) as opposed to peripheral intravenous (PIV) access due to the concerns about adverse events (i.e. tissue ischemia/necrosis) associated with extravasation through PIVs. In a truly hypotensive, critically ill patient the use of a PIV to administer vasopressors will allow the medication to stabilize the patient sooner and reduce the time to hemodynamic stability. The requirement to start vasopressors through a CVC may delay administration of pressors. Also, performing the insertion of a CVC in a hypotensive patient in an emergency circumstance versus an elective circumstance may increase the risk of adverse events from the procedure itself (i.e. bacteremia, pneumothorax, arterial puncture). Finally, most of the evidence cited for avoiding PIV administration of pressors is a sparse collection of case studies and expert opinion.
Background: Vasopressors are frequently used in critically ill patients with hemodynamic instability both in the emergency department (ED) as well as intensive care units (ICUs). Typically, vasopressors are given through central venous catheters (CVCs) as opposed to peripheral intravenous (PIV) access due to the concerns about adverse events (i.e. tissue ischemia/necrosis) associated with extravasation through PIVs. In a truly hypotensive, critically ill patient the use of a PIV to administer vasopressors will allow the medication to stabilize the patient sooner and reduce the time to hemodynamic stability. The requirement to start vasopressors through a CVC may delay administration of pressors. Also, performing the insertion of a CVC in a hypotensive patient in an emergency circumstance versus an elective circumstance may increase the risk of adverse events from the procedure itself (i.e. bacteremia, pneumothorax, arterial puncture). Finally, most of the evidence cited for avoiding PIV administration of pressors is a sparse collection of case studies and expert opinion.
What Study are we Reviewing in this Post?
Loubani OM et al. A systematic review of extravasation and local tissue injury from administration of vasopressors through peripheral intravenous catheters and central venous catheters. J Crit Care 2015; 30 (3): 653.e9 – 653.e17. PMID: 25669592
What They Did:
- A systematic review of Medline, Embase, and Cochrane databases from inception through January 2014 for reports of adults who received vasopressor through PIV or CVC
- Outcomes:
- Local Tissue Injury = Adverse event attributed to vasopressor administration occurring within close proximity to the infusion site
- Extravasation of vasopressor = Escape of solution containing vasopressor from vessel through which it is infused into surrounding tissue or body cavity
- Major disability = Patient unable to return to previous level of function because of severe deficits from event
Results:
- 85 articles with 270 patients and 325 separate local tissue injury and extravasation events included
- 318 events were from PIV administration
- 204 local tissue injury events (179 skin necrosis, 5 tissue necrosis, and 20 gangrene)
- 85.3% of adverse events occurred from PIVs located at sites distal to antecubital or popliteal fossae
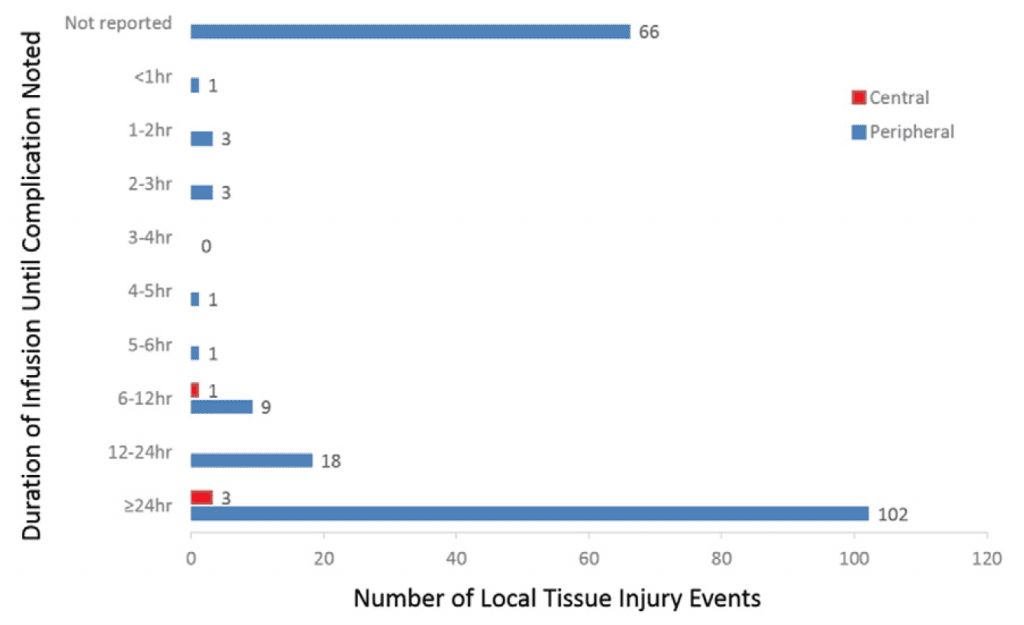
- 96.8% of adverse events occurred after 4 hrs of infusion from PIV
- Major disability and mortality in 9 (4.4%) and 4 (2.2%) of cases respectively
- 114 extravasation events
- 75.4% did not result in any tissue injury
- 75% of adverse events were distal to antecubital and popliteal fossae
- Major disability 3 cases (2.7%), and mortality 1 case (0.9%)
- 7 events were from CVC administration
- 4 local tissue injury events (3 skin necrosis & 1 gangrene)
- Long-term sequelae 3 cases and minor disability 2 cases
- Mortality in 1 case
- 3 extravasation events
- No injuries reported
- 4 local tissue injury events (3 skin necrosis & 1 gangrene)
- 204 local tissue injury events (179 skin necrosis, 5 tissue necrosis, and 20 gangrene)
Duration of Vasopressor Infusion
Strengths:
- This is the largest review to date looking at the use of vasopressors from PIVs
Limitations:
- This was a systematic review, but many of the studies had information abstracted from charts, so there may be some reporting bias (i.e. some complications may not have been documented) which would underestimate complications
- This review was only for complications from administration of vasopressor, and not a review of frequency of complications (i.e. instances where no complications occurred)
- There was a large inconsistency of reporting among the published studies reviewed. Critical information to analyze the outcomes of interest were missing in a lot of published reports.
Discussion:
- Currently administration of vasopressors via peripheral IVs is considered to be unsafe and often discouraged by some due to the concern of local tissue injury from extravasation, but this systematic review found only observational reports of complications of vasopressor infusion from PIVs.
- There were 204 local tissue injury events from vasopressor infusion from PIVs, but most (85.3%) of the complications occurred from PIVs distal to the antecubital or popliteal fossae and infusions running >4 hours (96.8%).
- Only one event was identified where local tissue injury occurred with infusion of vasopressor via PIV from <1 hour, which was a case of septic shock and an infusion of phenylephrine of unspecified dose via the saphenous vein of the left leg.
- There was one RCT comparing complication rates from vasopressor administration of CVC vs PIVs by Ricard et al, which reported increased complication rates from peripheral IVs, but details of the location of the catheters, the nature of the vasopressor, and the duration of infusion were not reported.
- The data from this review was derived mostly from case reports and case series and therefore may not be representative or typical of clinical practice, therefore no definitive conclusions can be drawn from this review about safety of PIV administration of vasopressors.
Study Conclusion:
Published data on tissue injury or extravasation from vasopressor administration via peripheral IVs are derived mainly from case reports and further study is warranted to clarify the safety of vasopressor administration via PIVs.
Clinical Take Home Point:
In critically ill patients, with hemodynamic instability, vasopressor infusion through a proximal PIV (antecubital fossa or external jugular vein), for <4hours of duration is unlikely to result in tissue injury and will reduce the time it takes to achieve hemodynamic stability.
References:
- Loubani OM et al. A systematic review of extravasation and local tissue injury from administration of vasopressors through peripheral intravenous catheters and central venous catheters. J Crit Care 2015; 30 (3): 653.e9 – 653.e17. PMID: 25669592
- Ricard JD et l. Central or peripheral catheters for initial venous access of ICU patients: a randomized controlled trial. Crit Care Med 2013; 41: 2108 – 15. PMID: 23782969
- Cardenas-Garcia J et al. Safety of Peripheral Intravenous Administration of Vasoactive Medication. J Hosp Med 2015. [Epub ahead of print]. PMID: 26014852
For More on This Topic Checkout:
- Scott Weingart at EMCrit: Podcast 107 – Peripheral Vasopressor Infusions and Extravasation
- Casey Parker at Broome Docs: PODCAST – Pushing Pressors in the Periphery
- Thomas D at Scancrit: Peripheral Noradrenaline
- Duncan Chambler at The Bottom Line: Loubani – A Systematic Review of Extravasation and Local Tissue Injury From Administration of Vasopressors Through Peripheral Intravenous Catheters and Central Venous Catheters
- Jeremy Faust & Lauren Westafer at FOAMCast: Episode 31 – Vasopressors
- Haney Mallemat at Resuscitation: Episode 42 – Vasopressors via Peripheral IV
- Justin Morgenstern at First 10 in EM: Peripheral Vasopressors – The Myth and the Evidence
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)



