 Background: Intravenous morphine use has been reported in nearly one of seven patients hospitalized with acute decompensated heart failure (ADHF). I have anecdotally, even seen physicians giving morphine as a “first-line” agent: Nitroglycerine, Non-Invasive Positive Pressure Ventilation (NIPPV), and Morphine. There is surprisingly little evidence supporting routine use of morphine in ADHF, and no major American cardiology or emergency medicine society has really endorsed or published any recommendations on the treatment of ADHF with morphine.
Background: Intravenous morphine use has been reported in nearly one of seven patients hospitalized with acute decompensated heart failure (ADHF). I have anecdotally, even seen physicians giving morphine as a “first-line” agent: Nitroglycerine, Non-Invasive Positive Pressure Ventilation (NIPPV), and Morphine. There is surprisingly little evidence supporting routine use of morphine in ADHF, and no major American cardiology or emergency medicine society has really endorsed or published any recommendations on the treatment of ADHF with morphine.
Most of us were taught the acronym “MONA,” Morphine, Oxygen, Nitroglycerin, and Aspirin for treatment of acute pulmonary edema and commonly, quoted physiologic/clinical beliefs for the use of morphine in ADHF are: beneficial hemodynamic effects, managing anxiety/agitation in air hunger, reduction in preload, and maybe to a lesser extent, afterload, and finally, decreasing heart rate. We should also consider the use of morphine in a framework of risk and benefit. For example intravenous morphine can also have some deleterious effects like causing central nervous system suppression, ventilatory depression, and hypotension.
The Acute Decompensated Heart Failure National Registry (ADHERE) is a large multicenter registry that records data from patients hospitalized with ADHF with more than 175,000 hospitalizations from over 250 hospitals across America. To be included in this registry patients must be >18years of age, admitted to an acute care hospital and receive a discharge diagnosis of ADHF. Data for this registry are collected by retrospective chart review and entered via an electronic web-based case report form for all consecutive eligible patients.
What Study are we Discussing?
Peacock WF et al. Morphine and Outcomes in Acute Decompensated Heart Failure: An ADHERE Analysis. Emerg Med J 2008; 25: 205 – 209. PMID: 18356349
What They Did:
- Retrospective analysis of the ADHERE Registry
- Patients stratified into 2 cohorts: Whether or not they received intravenous morphine
Outcomes:
- Need for Mechanical Ventilation
- Use of Inotropes and Vasodilators
- Median Hospitalization (Days)
- Need for ICU Admission
- Mortality
Results:
- 147,362 patient cases were in the ADHERE registry at December 2004
- 20,782 (14.1%) received IV morphine
- 126,580 (85.9%) did not receive IV morphine
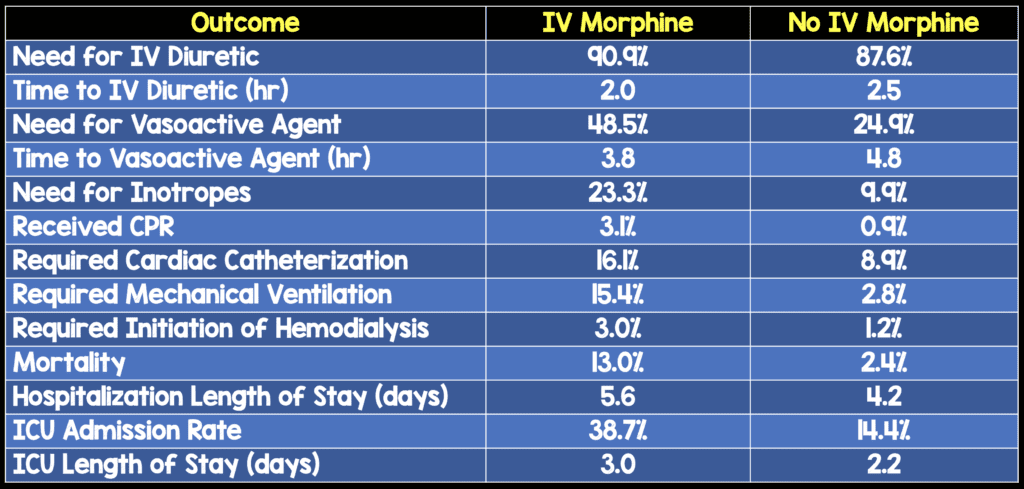
- IV Morphine vs No Morphine in ADHF
Strengths:
- The authors controlled for factors such as BUN, systolic BP, age, creatinine, dyspnea at rest, chronic dialysis, heart rate, inotrope or vasodilator use, elevated troponin, ejection fraction, use of morphine as adjunct for endotracheal intubation, and across all risk groups the use of morphine was associated with markedly increased mortality that was statistically significant
- Also, to control for the fact that repeat hospitalizations vs unique patients could have occurred, the mortality analysis was repeated looking at unique patients which made for a smaller final analysis of 30,276 patients and the increased mortality associated with morphine use in ADHF remained statistically significant.
Limitations:
- This was a retrospective study and therefore limits the findings of this study to that of hypothesis generation and not definitive evidence that morphine causes an increased risk of harm in ADHF. This study shows an increased association of mortality risk and should raise concern about the use of morphine in the armamentarium of medical therapy for the management of ADHF. There are no large randomized controlled trials demonstrating safety or efficacy for morphine in ADHF, but this study can only show association between the use of morphine and mortality and not causation.
- The morphine group had some baseline differences vs the non-morphine group: Higher prevalence of rest dyspnea, congestion on CXR, rales, and raised troponin. This could imply that patients receiving morphine represent a cohort with more severe illness and baseline and therefore would be predicted to have a greater mortality. However, even after extensive risk adjustment there was still a statistically significant relationship between increased mortality and morphine as evidenced by high odds ratios and significant p values.
- There was an increase in the association between mechanical ventilation and morphine use, but due to the constraints of the study, one cannot determine if morphine resulted in endotracheal intubation or if it was used as a sedative during the procedure (i.e. the timing of morphine use was not collected in ADHERE).
- The registry only recorded if patients received morphine, but the total dose used, the timing of its administration, and the precise temporal relationships to adverse events could not be determined
- There was no long-term follow-up in this study with findings being limited to in-hospital complications only. Consequences, such as rehospitalization after hospital discharge cannot be determined.
Discussion:
- Decreasing filling pressures are an important goal in the early treatment of ADHF and it is commonly assumed that morphine provides benefit in ADHF by decreasing venous tone and pressure, therefore increasing peripheral venous pooling, all of which decrease cardiac filling pressure. There has been a very small study however by Timmis AD et al [2], that showed the administration of morphine results in decline in both systemic blood pressure and heart rate, but left ventricular filling pressures were unchanged.
- Approximately 80% of patients with ADHF initially present to the emergency department and many arrive by ambulance. There are not that many studies examining the use of prehospital morphine early in the treatment of ADHF. There is one study by Sacchetti et al [3] that did report an increase in intubation rates and longer stays in the ICU if morphine was used.
Author Conclusion:
In this preliminary registry analysis of ADHF, the use of morphine was associated with a longer stay in the hospital, more frequent and longer ICU admissions, and a greater risk of in-hospital mortality.
Clinical Take Home Point:
The use of IV morphine in ADHF is associated with increased morbidity and mortality and should be abandoned completely as a “first-line” medical therapy. If you want to decrease diastolic filling pressures in ADHF from venous pooling just use nitroglycerin.
References:
- Peacock WF et al. Morphine and Outcomes in Acute Decompensated Heart Failure: An ADHERE Analysis. Emerg Med J 2008; 25: 205 – 209. PMID: 18356349
- Timmis AD et al. Haemodynamic Effects of Intravenous Morphine in Patients with acute Myocardial Infarction Complicated by Severe Left Ventricular Failure. BMJ 1980; 980 – 2. PMID: 7417767
- Sacchetti A et al. Effect of ED Management on ICU use in Acute Pulmonary Edema. AM J Emerg Med 1999; 17: 571 – 4. PMID: 10530536
For More Myths on This Topic Checkout:
- Anand Swaminathan at EMDocs: Furosemide in the Treatment of Acute Pulmonary Edema
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)



