 Background: IV access is one the most important interventions that must be performed in effectively managing patients in the Emergency Department. It is part of “Circulation” in the ABCs acronym and is even first in the “IV, O2, Monitor” phrase that we have become accustom to hearing. Although experienced ED nurses can obtain access quickly and without much difficulty in most patients, there remain a handful of patients that will present to the ED where standard peripheral access is unable to be obtained after multiple attempts. What is the next step? Peripheral placement of an IV using ultrasound can be a great next step if timing permits, but this too can be troublesome in patients who are difficult to access, especially if dehydration is present. IOs have become more popular but are painful when medications are given through them, thus making management more difficult in patients who are alert. Also IOs are limited in regards to what lab testing can be performed. Central lines are not worth the risk if IV access does not need to be central or if access is only needed temporarily. External Juglar IV placement can have similar difficulties as traditional peripheral access especially, in patients with a large body habitus or who have had repeated EJ cannulations. What if a peripheral IV was placed into the internal jugular vein (Easy IJ)? It is an easily visualized structure on ultrasound and cannulating it is a skill that is familiar to most Emergency physicians. Is this a safe approach?
Background: IV access is one the most important interventions that must be performed in effectively managing patients in the Emergency Department. It is part of “Circulation” in the ABCs acronym and is even first in the “IV, O2, Monitor” phrase that we have become accustom to hearing. Although experienced ED nurses can obtain access quickly and without much difficulty in most patients, there remain a handful of patients that will present to the ED where standard peripheral access is unable to be obtained after multiple attempts. What is the next step? Peripheral placement of an IV using ultrasound can be a great next step if timing permits, but this too can be troublesome in patients who are difficult to access, especially if dehydration is present. IOs have become more popular but are painful when medications are given through them, thus making management more difficult in patients who are alert. Also IOs are limited in regards to what lab testing can be performed. Central lines are not worth the risk if IV access does not need to be central or if access is only needed temporarily. External Juglar IV placement can have similar difficulties as traditional peripheral access especially, in patients with a large body habitus or who have had repeated EJ cannulations. What if a peripheral IV was placed into the internal jugular vein (Easy IJ)? It is an easily visualized structure on ultrasound and cannulating it is a skill that is familiar to most Emergency physicians. Is this a safe approach?
Clinical question: Is placement of peripheral IV catheters into the Internal jugular vein a safe means of access in patients where IV access is unable to be obtained?
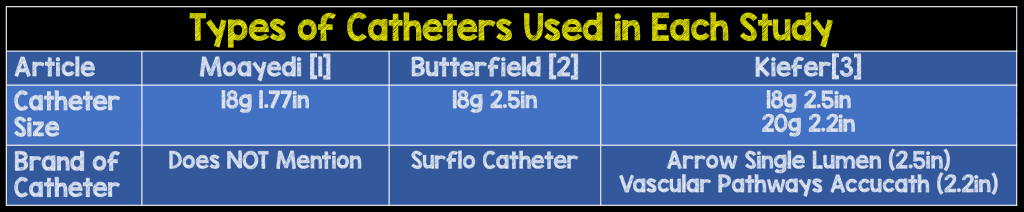
Moayedi S et al. Safety and Efficacy of the “Easy Internal Jugular (IJ)”: An Approach to Difficult Intravenous Access. J Emerg Med 51(6): 636 – 642. PMID: 27658558 [1]:
What They Did:
- Multicenter non-comparative trial at resident affiliated hospital and 2 tertiary care urban academic centers.
- Inclusion criteria: ED patients where peripheral or external jugular vein cannulation failed (included ultrasound guided attempts); IJ dilatation with Valsalva; Ability to sign written consent.
- Exclusion criteria: hemodynamic instability (HR >150 or MAP <60); Untreated Pneumothorax; Need for triple lumen catheter.
- Catheters were placed by physician with a minimum of 5 previous successful IJ vein cannulations using seldinger technique and 5 previous peripheral ultrasound guided vein cannulations.
- Procedure: Skin was prepped with chlorhexidine. High frequency probe was used along with Sterile probe cover. The patient performed valsalva. 18g 4.5 cm catheter was placed. Catheters remain in place at a max of 24 hours.
- Data was recorded by research team member who observed each procedure. Time from skin prep to confirmation of IV access (aspiration of blood and injection of 10 ml fo saline) was recorded.
Outcomes:
- Assessed for patency of catheter post placement, pneumothorax, arterial puncture, and hematoma
Results:
- 83 attempts in 74 patients. Four patients underwent more than 1 attempt in the same day
- Initial success rate was 88%. Ten catheters failed at initial insertion and 10 lost patency. The remaining 63 were effective until taken out.
- BMI was statistically similar between those who failed insertion (28.8 kg/m2), those with post insertion loss of patency (30.3 kg/m2), and those with preserved patency (28.1 kg/m2)
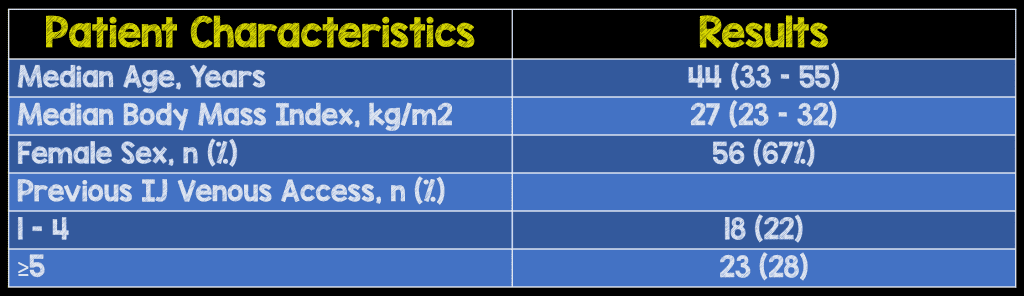
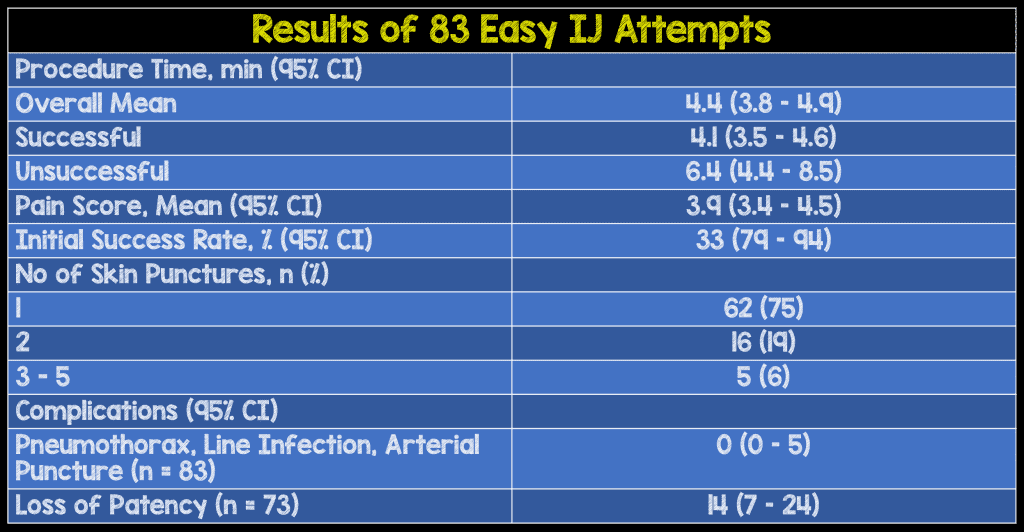
- Mean procedure time was 4.4 min (range 1-10.5 mins)
- Line infection and complications were evaluated by home contact after d/c (10 patients), 48 hour hospital visit (18 patients) and chart review (55 patients)
Strengths:
- Multicenter study
- Independent research team members observed procedure and recorded the procedure start/stop time and assessed for any immediate complications
- Large study population when compared to previous studies on this topic
Limitations:
- Majority of attempts were made by experienced physicians and there may be more complications with inexperienced providers.
- The catheters were only placed in stable patients who could consent so the article is unable to comment on safety in more ill patients
- Dwell time was limited to 24 hours so safety beyond then could not be determined by this study
- Most of the patients were followed up using chart review which limits the ability to follow up patients who may have been discharged.
Butterfield M et al. Using Ultrasound-Guided Peripheral Catheterization of the Internal Jugular Vein in Patients with Difficult Peripheral Access. Am J Ther 2015. PMID 26469683 [2]:
What They Did:
- Prospective observational study in consecutive patients admitted to ICU or medical ward with difficult IV access (defined as 2 or more failed attempts).
- Inclusion Criteria: Two or more failed attempts at peripheral access by experienced nurses
- Exclusion Criteria: None
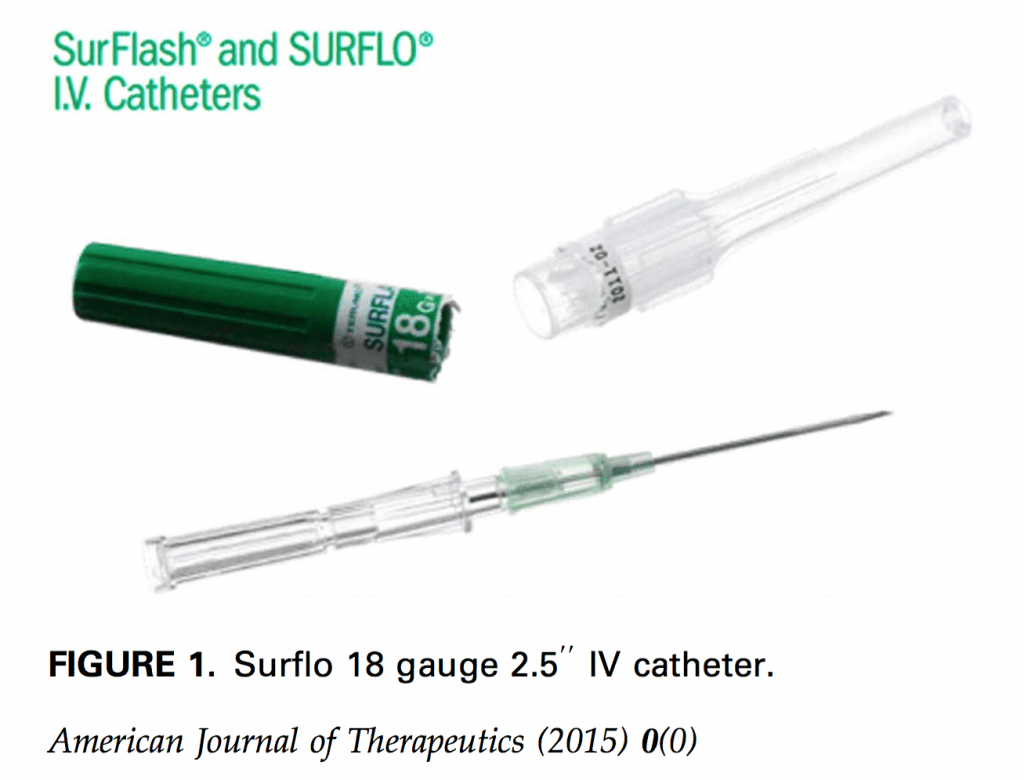
- Procedure: high frequency linear ultrasound probe with sterile probe cover, sterile gel, Lidocaine, chlorhexidine for cleaning, and bio-occlusive dressing were used. 2.5in 18g catheter was placed. Max amount of time that the catheters were placed was 7 days.
- Patient monitored daily for complications.
Outcomes:
- Assessed for complications such as line infection, hematoma, pneumothorax, neck pain/stiffness
Results:
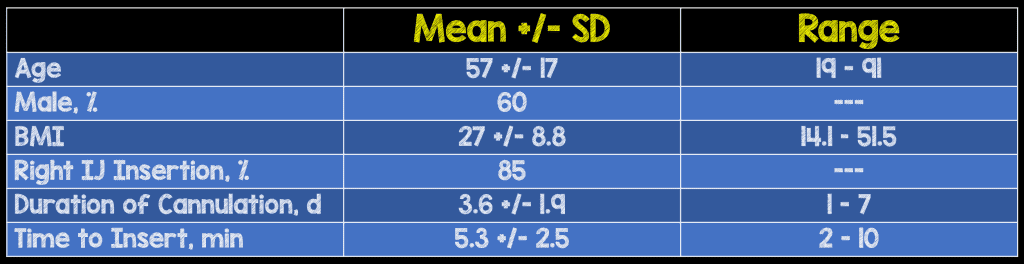
- 20 catheters were placed in 19 patients (one patient had one catheter exchanged for another after 7 days). Mean BMI was 26 (14.1-51.5).
- 16 were placed on the 1st attempt and the remaining 4 were placed successfully on the 2nd attempt.
- Average duration for catheter placement was 3.2 days (1-7 days). Average time to place was 5.3 mins (2-10 mins).
- There were no signs of fever, neck pain/stiffness, or hematoma on follow up. There were no immediate complications noticed.
- One patient with nephrotic syndrome developed right IJ DVT but this was attributed to the patient’s hypercoagulable state as the patient was also found to have right cephalic, right radial, and left cephalic vein clots.
Strengths:
- The studied population consisted of wide range of patient demographics with age ranging from 19-91 and BMI from 14.1-51.5.
- Patients were inpatient and were observed every day for signs of complications
Limitations:
- Small sample size with only 19 patients being studied
- The time to placement of catheter was documented but there is no mention on when the timer was started or stopped. Did the timer start when the physician saw the patient or did it start when the decision was made to place the catheter?
- Lack of independent observer for signs of immediate complications or later complications
Kiefer D et al. Prospective evaluation of ultrasound-guided short catheter placement in internal jugular veins of difficult venous access patients. Am J Emerg Med 2016; 34(3): 571 – 81. PMID: 26776533 [3]:
What They Did:
- Prospective convenience study in 2 urban academic centers
- Inclusion Criteria: Age greater than 18, failed IV placement and no EJ site was identified, no indication clinically for CVL.
- Exclusion Criteria: Overlying skin infection
- Procedure: High frequency linear ultrasound probe along with sterile probe cover, chlorhexadine for cleaning, and bio-occlusive dressing was used. Two types of catheters were used [18g 6.36 cm (2.5 in) catheter and a 20g 5.7 cm (2.2 in.) catheter].
- Complications were assessed at the time of procedure, 1 week after via chart review, and 6 weeks after via chart review.
Outcomes:
- Assessed for complications such as local neck abnormality, pneumothorax, bleeding, infection, or intravascular clot formation
Results:
- 33 patients received catheters.
- 3 catheters failed due to becoming dislodged.
- The median number of catheter placement attempts was 1 and the maximum number of attempts was 3.
- Median time for placement was 4 minutes.
- Seven patients were discharged from ED and 26 were admitted.
- No immediate complications were observed. There was no documented evidence or clinical suspicion for complication of line placement at 6 week follow up.
- One patient had a positive blood culture for Staph Aureus at 1 week follow up but this patient was admitted for sepsis.
- There were 3 deaths reported but 2 of these deaths were in hospice patients and one was from pneumonia.
Strengths:
- The studied population consisted of a wide variety of pathology (DM, ESRD on HD, IV drug use, HTN, HPLD, PVD, CAD, Chronic pain, Cirrhosis, Metastatic Cancer)
- Follow up chart review at 1 week and 6 weeks was performed by independent physicians.
Limitations:
- Convenience sample was used which introduces more bias.
- Two different catheter lengths were used and there is no mention on whether the shorter or longer catheter failed in the 3 failed attempts.
- Complications were assessed by chart review instead of being observed.
- Immediate complications were assessed by Emergency physician and not an independent observer.
- Patients with complications who were discharged could have sought care at another facility where the investigators did not have access to records which means that some complications could have potentially been lost.
Authors’ Conclusion:
All three authors found that the peripheral IJ was a relatively easy and quick procedure that resulted in no major complications in patients that did not require central venous access.
Discussion:
Peripheral IJ placement has a place in the Emergency Department. Although more expansive studies would help assure safety, there were no major complications seen in these three studies. Accessing the internal jugular vein is a familiar procedure for emergency physicians so these can be placed relatively quickly and easily. They have benefits over IOs in that they are less painful and blood can be obtained for a wider range of testing. The technique described in literature uses sterile gloves, lidocaine, and sterile towels. Full sterile draping typically used in CVL placement is not required which is an added bonus. As placement of these are not currently a widespread practice, discussion with inpatient services about using peripheral IJ catheters may be beneficial. If these are placed, the inpatient team likely should be notified where and why it was placed.
Clinical Take Home Point:
Next time you have a patient with difficult peripheral access and the patient does not need a CVL, consider an ultrasound guided peripheral IJ.
Guest Contributor
Name: Rodrick Darnell Johnson
Title: PGY-3 Emergency Medicine Resident
Hospital: Univerisity of Arkansas for Medical Sciences
City/State: Little Rock, AR
References:
- Moayedi S et al. Safety and Efficacy of the “Easy Internal Jugular (IJ)”: An Approach to Difficult Intravenous Access. J Emerg Med 51(6): 636 – 642. PMID: 27658558
- Butterfield M et al. Using Ultrasound-Guided Peripheral Catheterization of the Internal Jugular Vein in Patients with Difficult Peripheral Access. Am J Ther 2015. PMID 26469683
- Kiefer D et al. Prospective evaluation of ultrasound-guided short catheter placement in internal jugular veins of difficult venous access patients. Am J Emerg Med 2016; 34(3): 571 – 81. PMID: 26776533
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie) & Anand Swaminathan (Twitter: @EMSwami)



