- We should get ABGs instead of VBGs
- After Intravenous Fluids (IVF), Insulin is the Next Step
- Once pH <7.1, Patients Need Bicarbonate Therapy
- We Should Bolus Insulin before starting the infusion
DKA Myths
Case: 25 y/o female with PMH of Type I DM who presents via EMS with AMS. Per EMS report, the patient ran out of her insulin 3 days ago…..
- Vital Signs: BP 86/52 HR 136 RR 30 O2Sat 97% on room air Temp 99.1
- Accucheck: CRITICAL HIGH
- EMS was not able to establish IV access, so decided to just bring her to the ED due to how sick she looks.
- Your nurses are on point today and get you two large bore 18G IVs and start to draw blood work to send to the lab. You state I need a blood gas, and the nurse turns to you and asks do you need an ABG or VBG?
Myth #1: We should get ABGs instead of VBGs in DKA
So you do a literature review and come across two studies that specifically look at ABG vs VBG in an ED population:
Study #1: Kelly AM et al. Review Article – Can Venous Blood Gas Analysis Replace Arterial in Emergency Medical Care. Emery Med Australas 2010; 22: 493 – 498. PMID: 21143397
- For pH, 3 studies of patients with DKA (265 patients) were reviewed showing a weighted mean difference of 0.02 pH units. Only one study, which was the largest study (200 patients) reported 95% limits of agreement of pH that were -0.009 – 0.02 pH units.
- For bicarbonate, 7 studies with just over 900 patients were reviewed showing a weighted mean difference of -1.41 mmol/L. Only 2 studies (246 patients and 95 patients) reported 95% limits of agreement which ranged from -5.8 to +5.3 mmol/L.
Study #2: Ma OJ et al. Arterial Blood Gas Results Rarely Influence Emergency Physician Management of Patients with Suspected Diabetic Ketoacidosis. Acad Emerg Med Aug 2003; 10(8): 836 – 41. PMID: 12896883
- ABG analysis changed ED physicians diagnosis in 1% (95% CI 0.3 – 3.6%) of patients
- ABG analysis changed ED physicians treatment in 3.5% (95% CI 0.3 – 3.6%) of patients (Change from SQ to IV insulin or vice versa)
- ABG analysis changed patient disposition in 2.5% (95% CI 1.1% – 5.7%) of patients
- Venous pH correlated well with arterial pH with difference of -0.015 +/- 0.006 pH units
Other Reasons ABGs may not be preferred
- Although rare, ABGs can cause radial artery spasm, infarct, and/or aneurysms
- ABGs are painful to patients, even more so than IV access
- By the way, when is the last time you checked a Modified Allen’s Test before doing a radial ABG?
- Block off Radial and Ulnar Artery for 30 seconds
- Have pt make fist
- Let go of ulnar artery and should have color return in <10seconds
- If no color return or delayed…then pt DOES NOT have collateral blood flow (i.e. – Allen’s Test)
Myth#1 Busted: VBG can be used in place of ABGs
Your VBG comes back and shows the following results:
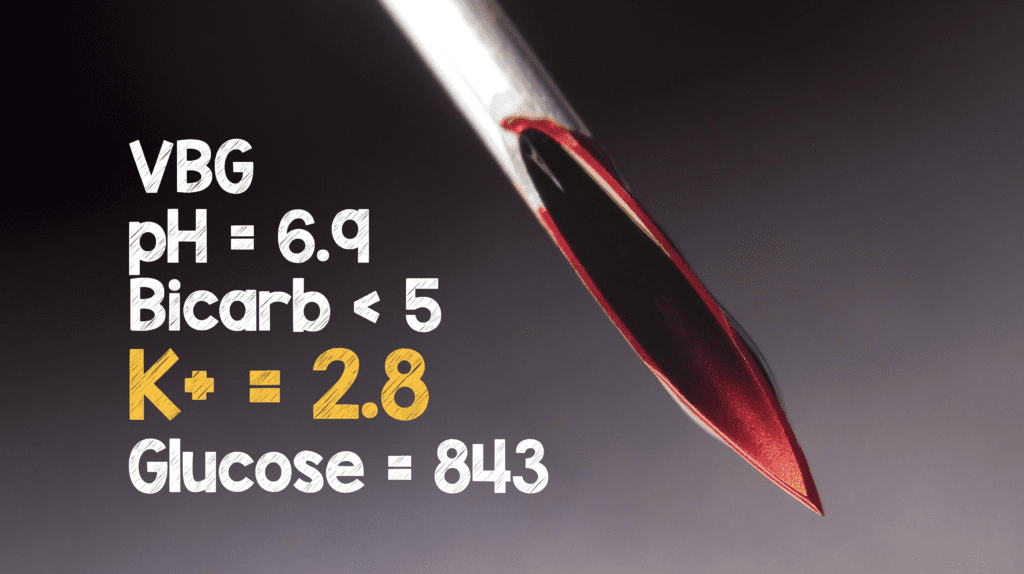
You start IVFs and want to initiate insulin therapy next….
Myth #2: After Intravenous Fluids (IVF), Insulin is the Next Step
Patients with DKA will have total body potassium depletion from osmotic diuresis and electrolyte losses. Measured levels of serum potassium may be falsely normal or elevated due to extracellular shifts of potassium from secondary acidosis. The American Diabetes Association (ADA) actually recommends obtaining a a serum potassium level before initiating insulin, but this is based on anecdotal evidence. That being said, according to Arora et al, approximately 5% of patients with DKA will have hypokalemia.
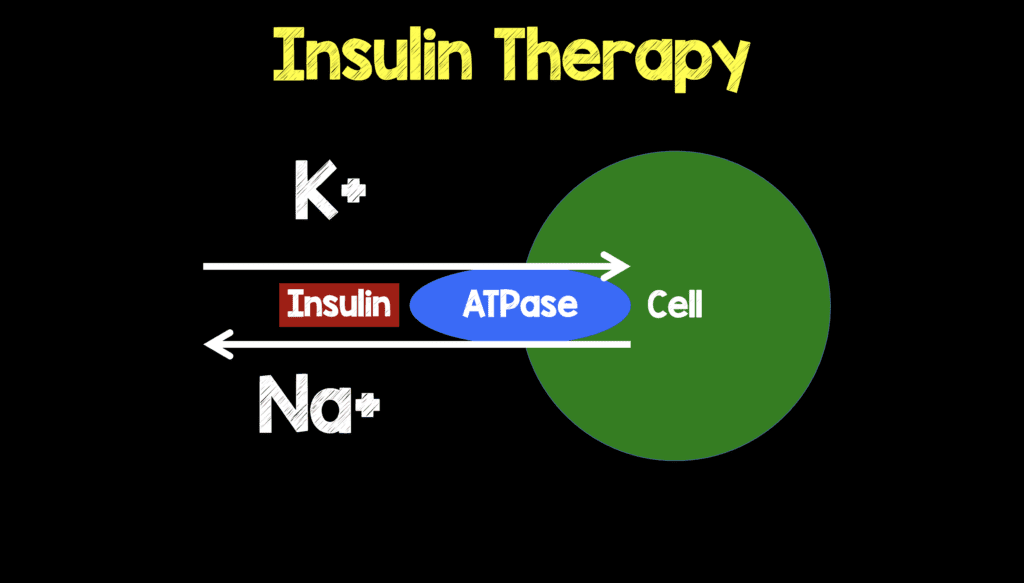
If you look back to your VBG you will see your K+ is 2.8. If you start insulin therapy before electrolyte replacement you you will worsen hypokalemia which is a very real cause of morbidity and mortality from cardiac arrhythmias and respiratory muscle weakness. Don’t forget that insulin will activate your Sodium-Potassium ATPase which will shift potassium intracellular and worsen your hypokalemia.
So the next real question is how should K+ be replaced? An oversimplified and general rule of thumb is that for every 10mEq of K+ given the serum K+ should rise by 0.1mEq, but at extremely low potassium levels this rule is not exactly true. I would also remember a few other things:
- Place ALL patients on monitor for continuous ECG monitoring
- Maximum Concentration for Peripheral IV administration = 10mEq/50mL
- Maximum Concentration for Central IV administration = 20mEq/50mL
Every institution will have its own protocols for what is the acceptable rate of IV potassium repletion, but the first thing I would say is that if the Oral or Enteral route is available, use it. Below I will try and describe how I replace potassium, but certainly other ways are acceptable, and every patient is different, but in general….
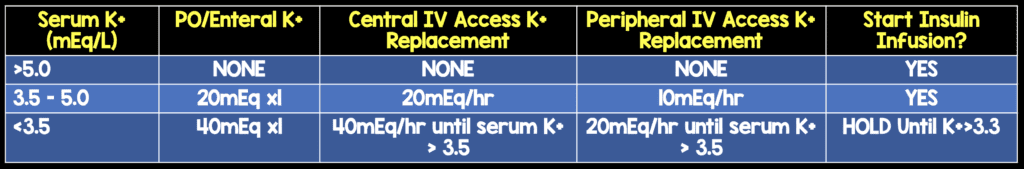
Clinical Bottom Line: After starting IVF, the next step in DKA management is electrolyte replacement, NOT Insulin.
Your nurse now approaches you and says that the patients pH is 6.9 so we need to give the patient sodium bicarbonate…
Myth #3: Once pH <7.1, Patients Need Bicarbonate Therapy
Consensus guidelines for the management of DKA recommended administering sodium bicarbonate to DKA patients who present with an initial blood gas pH of < 7.0. That recommendation was updated and changed in 2009 to limit sodium bicarbonate use to DKA patients with blood gas pH of < 6.9.
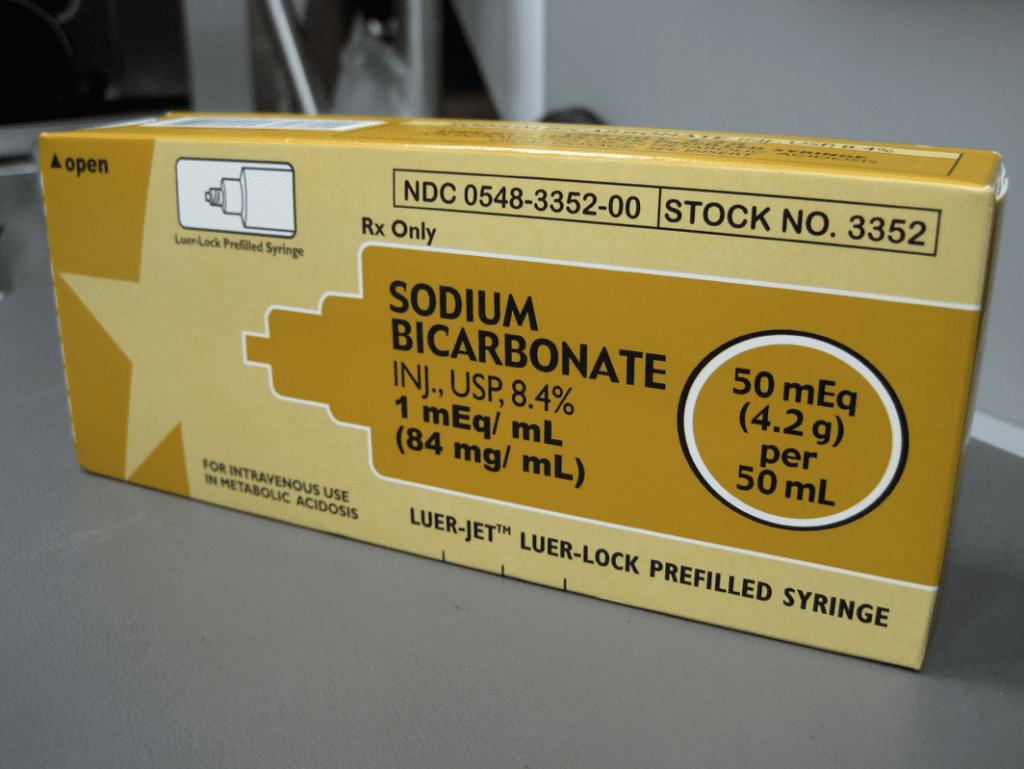
Guidelines are nice, but they don’t keep up with research….Since the 2009 DKA guideline….2 more studies have come out evaluating the usefulness of sodium bicarbonate in DKA. There has been a systematic review published in 2011 and the largest retrospective analysis ever published in 2013. We have covered both of these before on REBEL EM: Any Benefit to Sodium Bicarbonate in DKA?. To summarize:
Study #1: Chua et al. Bicarbonate in Diabetic Ketoacidosis – A Systematic Review. Ann Intensive Care 2011; 1 (23). PMID: 21906367
- 44 studies of DKA patients reviewed which showed:
- Transient improvement in metabolic acidosis
- No improved glycemic control
- Risk of cerebral edema in pediatric patients
- No studies with pH <6.85
Study #2: Duhon et al. Intravenous Sodium Bicarbonate Therapy in Severely Acidotic Diabetic Ketoacidosis. Ann Pharmacother 2013. 47(7 – 8): 970 – 5. PMID: 23737516
- Retrospective study of 86 patients with DKA which showed:
- No difference in: Time to resolution of acidemia, time to hospital discharge, time on IV insulin, potassium requirement in 1st 24hrs
- Subgroup Analysis of pH < 6.9 (n = 20) showed no statistical difference in time to resolution of acidemia
Clinical Bottom Line: Intravenous bicarbonate therapy may transiently make acidemia better, but there is no improvement of glycemic control, time on insulin, time to hospital discharge, and in kids can worsen cerebral edema.
So after potassium replacement your potassium is finally at an acceptable level so that you may start insulin therapy. Your nurse asks you would you like to bolus the insulin before you start the infusion?
Myth #4: We Should Bolus Insulin Before Starting the Infusion
Again we have covered this on REBEL EM: Is There Any Benefit to an Initial Insulin Bolus in Diabetic Ketoacidosis? Again, I will summarize the key study here:
Goyal et al. Utility of Initial Bolus Insulin in the Treatment of Diabetic Ketoacidosis. J Emerg Med 2010; 38(4): 422 – 7. PMID: 18514472
- Prospective, Observational Study of 157 patients with DKA:
- Insulin bolus at the start of an insulin infusion IS EQUIVALENT to no insulin bolus at the start of an insulin infusion in several endpoints including:
- Decrease normalization of glucose
- Affect the rate of change of anion gap
- Reduce ED or hospital length of stay
- Insulin bolus at the start of an insulin infusion DOES:
- Increase hypoglycemic events by 6 fold (6% vs 1%) [NOT Statistically Significant]
- Insulin bolus at the start of an insulin infusion IS EQUIVALENT to no insulin bolus at the start of an insulin infusion in several endpoints including:
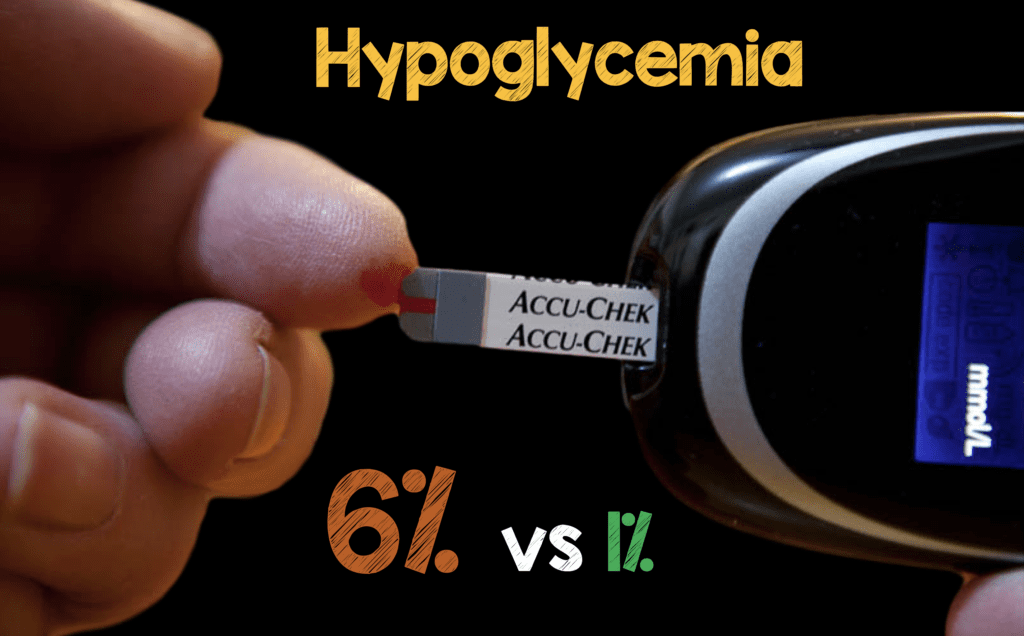
I generally just start my insulin drips at 0.05 – 0.14 U/kg/hr, only after electrolytes have been replaced.
Clinical Bottom Line: Insulin boluses increase hypoglycemic events without other clinical benefits in the treatment of DKA.

Clinical Bottom Line in DKA Management:
- VBG can be used in place of ABGs
- After starting IVF, the next step in DKA management is electrolyte replacement, NOT Insulin.
- Intravenous bicarbonate therapy may transiently make acidemia better, but there is no improvement of glycemic control, time on insulin, time to hospital discharge, and in kids can worsen cerebral edema.
- Insulin boluses increase hypoglycemic events without other clinical benefits in the treatment of DKA.
For More on this Topic Checkout:
- Anand Swaminathan at EMDocs: Myths in DKA Management
- Darrel Hughes at REBEL EM: Any Benefit to Sodium Bicarbonate in DKA?
- Darrel Hughes at REBEL EM: Is There Any Benefit to an Initial Insulin Bolus in Diabetic Ketoacidosis?
- Anand Swaminathan at EMRAP: DKA Myths
- Josh Farkas on PulmCrit(EMCrit): Blood Gas Measurements in DKA – Are We Searching for a Unicorn?
- Josh Farkas on PulmCrit(EMCrit): Dominating the Acidosis in DKA



