 Definition:
Definition:
- Accidental hypothermia is an unintentional core body temperature of < 35°C when heat loss to surroundings is greater than heat generation
- Most frequent cause is environmental exposure
- Patient with impaired thermoregulation can develop hypothermia in relatively warm environments
- Elderly, underlying illness, trauma, intoxication, or malnutrition (Brown 2012)
- Elderly, underlying illness, trauma, intoxication, or malnutrition (Brown 2012)
Classification:
- Multiple classification systems have been used to delineate severity of hypothermia, some based on core body temperature and ssome based on symptoms
- Symptoms and core body temperature do not always correlated
- Management should be guided by symptoms, temperature ranges have limited clinical utility
- Core Body Temperature
- Mild: 35°C-32°C
- Moderate: 32°C-28°C
- Severe: <28°C
- Modified Staging System (Brown 2016)
- Mild (HT I)- Conscious and shivering (approximate core temperature 35°C-32°C)
- Moderate (HT II)- Impaired conscious, may or may not be shivering (approximate core temperature <32°C-28°C)
- Severe (HT III)- Unconscious, vital signs present (approximate core temperature <28°C)
- HT IV- Vital signs absent (approximate core temperature <28°C)
Presentation:
- Diagnosis is made by checking a core temperature
- Patients with any of the following should have their core temperature measured
- Depressed oral, axillary or rectal temperature
- Altered mental status
- History of exposure and altered vital signs
- Have a high degree of suspicion for hypothermia in elderly, undomiciled, and intoxicated patients
- Mild Hypothermia
- Tachycardia
- Tachypnea
- Shivering
- Nausea or ileus
- Cold diuresis: polyuria caused by vasoconstriction and a decrease in ADH production
- Ataxia, clumsiness, slowed response to stimuli, and dysarthria (Vassalo 2015)
- Moderate Hypothermia
- Bradydysrrhythmia or atrial fibrillation
- Hypotension
- Hypoventilation
- Bronchorrea
- Lethargic but responsive to verbal stimuli
- Loss of shivering
- Hyporeflexia
- Mydriasis
- Oliguria
- Coagulopathy
- Paradoxical undressing: a phenomenon in which the patient undresses despite significant hypothermia, believed to be caused by peripheral vasodilation secondary to autonomic dysfunction causing the sensation of skin warmth in combination with altered mental status. Some degree of undressing is seen in up to 30% of fatal hypothermia cases (Brändström 2012)
- Severe Hypothermia
- Responsive to noxious stimuli or unresponsive
- Bradycardia
- Ventricular dysrrhythmias
- Hypotension,
- Pulmonary edema,
- Anuria
- Areflexia
- Asystole
- Psuedorigormortis: increase in muscle tone due to a shivering like response, can lead to compartment syndrome of the extremities
Differential Diagnosis:
- Sepsis should be high on the differential for unexplained hypothermia
- Hypothermia with altered mental status can mimic, or coexist with, many other derangements
- Hypoglycemia
- Shock
- CVA
- Infection
- Intoxication
- Hypothyroidism
- Adrenal insufficiency
- Metabolic derangement
- Malnutrition
Management:
- Cooling decreases cerebral oxygen requirements allowing for neurologically intact survival after prolonged periods of hypoperfusion. Patients should be actively resuscitated to a core temperature of >32°C before termination is considered
- Basic Interventions
- Take care when moving hypothermic patients as jostling can precipitate ventricular dysrhythmias. This concern should not prohibit necessary patient care
- Large bore IV or IO access x2, Supplemental O2, Cardiac Monitor
- Continuous core temperature monitoring
- Esophageal probe: best option, falsely high with warmed air ventilation or thoracic lavage
- Rectal probe: falsely low, lags during rewarming
- Bladder probe: unreliable, not recommended
- Remove wet clothing, check for frost bite, prevent further heat loss
- Primary and secondary trauma survey if altered mental statue or unclear history
- Resuscitation
- Mild and Moderate Hypothermia
- Airway
- Monitor for bronchorrhea and depression of mental status
- Breathing
- Use warm humidified oxygen as needed
- Circulation
- IV fluids should be warmed to 40°C. They do little to warm the patient but room temperature fluids can lead to further heat loss
- Hypotensive patients should be aggressively fluid resuscitated as they are usually volume down due to hypothermic diuresis and fluid shifts
- Hypothermia induced dysrhythmia typically resolve with rewarming
- Sinus bradycardia is a normal physiologic response and should be treated with rewarming, atropine is usually not effective
- Atrial fibrillation and atrial flutter usually resolve with rewarming
- Passive and active external rewarming are the mainstays of treatment
- Airway
- Hypothermic Cardiac Arrest
- It is important to determine whether hypothermia preceded arrest. Hypothermia as the cause of arrest has positive prognostic implications while hypothermia secondary to arrest is rarely survivable
- Airway and Breathing
- Follow standard management as with any cardiac arrest
- Circulation
- Peripheral pulses are unreliable in all cardiac arrest and more so in hypothermic arrest due to vasoconstriction
- Consider ultrasound guided resuscitation to measure cardiac contractility
- Consider early arterial line placement
- Basic Life Support
- Begin continuous high quality chest compressions in patients without a pulse
- Continue compressions until the patient is warm, shows signs of life, or ROSC is achieved
- Consider the use of a mechanical compression device if available as prolonged, high quality compression may be required
- Central Venous Access
- Peripheral access preferred if can rapidly and reliably be obtained
- Irritation of the myocardium from the guide wire can result in dysrhythmias
- If central access required, consider femoral venous line placement (Danzl 2007)
- Advanced Life Support
- AHA ACLS guidelines: “It may be reasonable to consider administration of a vasopressor during cardiac arrest according to the standard ACLS algorithm concurrent with rewarming strategies (Class IIb, LOE C)” (Hoek 2010)
- There is a theoretical concern that IV medications will not be effective and will accumulate to toxic levels in the severely hypothermic patient. Some experts recommend withholding vasopressors, or limiting doses, until after the patient is warmed to > 30°C (Brown 2012)
- Ventricular dysrhythmias are often refractory to electricity when the patient is still hypothermic
- ECMO
- ECMO is the best option for severely hypothermic patients without signs of life who do not respond to initial resuscitative efforts. It has been shown to improve neurologically intact survival (48% to 63% survival with ECMO, <37% without ECMO) (Brown 2012)
- Peripheral pulses are unreliable in all cardiac arrest and more so in hypothermic arrest due to vasoconstriction
- Active internal rewarming is required; external rewarming is less effective in patients in cardiac arrest
- Active rewarming should continue until a core temperature of >32°C regardless of whether ROSC is achieved prior to this point (Zafren 2018)
- Mild and Moderate Hypothermia
- Diagnostic Testing
- Labs (think of the trauma triad of death: hypothermia, coagulopathy, and metabolic acidosis)
- Fingerstick Glucose
- Prevent hypoglycemia. Hypothermia lowers metabolic rate and makes it difficult for the patient to generate heat. Any amount of hypoglycemia will further exacerbate this
- BMP
- K > 10 mEq/L carries very poor prognosis in patients in cardiac arrest (Brown 2012)
- CBC
- Coagulation panel
- Disseminated Intravascular Coagulation (DIC) may occur from cold
- Coagulation panel may, however, be normal as blood is warmed prior to testing and factors are temperature dependent
- VBG or ABG if clinically indicated
- CK (rhabdomyolysis common)
- TSH (rule out myxedema coma)
- Consider blood cultures and cortisol level to assess for other contributing factors
- Fingerstick Glucose
 EKG
EKG
- Bradycardia is a normal physiologic response to hypothermia. Heart rate and oxygen consumption decrease by 50% at core temp of 28°C. (Danzl 2007)
- Wide QRS, prolonged PR and QT intervals
- Osborn waves (J waves)
- May be seen in other settings (Wang 2011)
- The risk for ventricular arrhythmias increases at < 32°C, and substantially increases at < 28°C
- CXR
- Look for pulmonary edema and aspiration pneumonia
- Further imaging as indicated by history of trauma
- Labs (think of the trauma triad of death: hypothermia, coagulopathy, and metabolic acidosis)
- Rewarming (Danzl 2007)
- Rewarming can be considered in three main categories. The method of rewarming is based on individual patient factors and available local resources
- Passive
- Warm environment (resuscitation bay lights) and clothing, encourage physical activity, warm drinks
- The patient must be able to generate their own body heat
- Can raise internal body temperature ~2°C per hour
- Active external and minimally invasive internal rewarming
- Warmed blankets, forced air heating (I.e. air hugger), warmed IV fluid
- Can raise internal body temperature ~2°C per hour
-
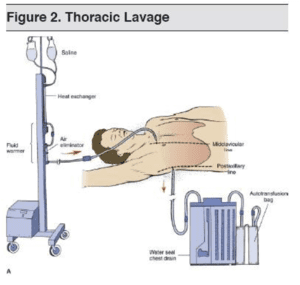
Thoracic Lavage (Auerbach 2007) Active internal rewarming (Brown 2012)
- Warmed humidified ventilation (~1.5°C per hour)
- Peritoneal dialysis (1-3°C per hour, may be high risk in the emergency setting)
- Hemodialysis (2-4°C per hour)
- Thoracic Lavage (3°C per hour)
- Endovascular warming devices (~2-3°C per hour)
- VV or VA ECMO (4-6°C per hour)
- Cardiopulmonary Bypass (9°C per hour)
- Used in any patient that is hemodynamically unstable
- Passive
- Rewarming can be considered in three main categories. The method of rewarming is based on individual patient factors and available local resources
-
- Gastric, colonic, and bladder irrigation are not recommended
- Afterdrop
- A drop in core temperature after initiation of rewarming
- May occur due to peripheral vasodilation and return of chilled blood to the core, though there is controversy whether this is a clinically significant phenomenon
- Rewarming should focus on warming the core to minimize this risk
- Hypothermic patients in cardiac arrest may benefit from standard post arrest targeted temperature management, but there is limited evidence to guide practice here
- If patient fails to rewarm 1°C/hour, consider other contributing factors or causes (ie sepsis, hypothyroidism etc)
- Termination of Resuscitation
- Survival after 6.5 hours of CPR with active internal rewarming has been reported (Lexow 1991) as has survival after a core temperature of 9°C (Vassallo 2015)
- In general, resuscitative efforts should continue until the patient has been successfully rewarmed (>32°C)
- Patients with a core temp >32°C with persistent asystole are unlikely to achieve ROSC and termination should be considered
- Termination should also be considered in patients with K > 12 mEq/L
Disposition:
- Mild hypothermia can usually be rewarmed and discharged home as long as protection from repeat exposure is guaranteed (i.e. do not discharge a homeless patient who presents with mild hypothermia unless they are going to a safe, heated environment)
- Patients with severe hypothermia or hypothermic arrest who are successful rewarmed and resuscitated should be admitted to the ICU. Many patients will develop organ failure within the first 24 hours of admission
- Pulmonary edema is the most common cause of in hospital mortality among these patients (van der Ploeg 2010)
Take Home Points:
- Hypothermia is neuroprotective and patients can survive prolonged periods of cardiac arrest. Termination of resuscitative efforts in cardiac arrest should not considered until the patient is >32°C or has a K > 12 mEq/L
- Active internal rewarming is the keystone of treatment for unstable hypothermic patients. Utilize available resources including ECMO to effectively warm your patient
- Consider alternate causes for hypothermia, especially in patients who fail to respond to warming
Guest Post By:

Lee Johnson
MS IV NYU School of Medicine
For More on This Topic Checkout:
- LITFL: Hypothermia
- EMCrit: Podcast 66 – …Until they are warm and dead: Severe Accidental Hypothermia
- EM Basic: Hypothermia
References:
- Brown DJ et al. Accidental hypothermia. NEJM 2012; 367(20): 1930-1938. PMID: 23150960
- Brown DJ. Hypothermia. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e New York, NY: McGraw-Hill; 2016. Link
- Vassallo SU et al. Thermoregulatory Principles. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e New York, NY: McGraw-Hill; 2015. Link
- Brändström H et al. Fatal hypothermia: an analysis from a sub-arctic region. Int J circumpolar health 2012; 71(1). PMC: 3417546
- Danzl, DF, 2007. Accidental Hypothermia. In P. S. Auerbach, ed. Wilderness Medicine, 7e Philadelphia, PA: Elsevier; 20070.
- Hoek TL et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122(18 suppl 3). PMID: 20956228
- Zafren K et al. Accidental Hypothermia. In Walls R, Hockberger RS, Gausche-Hill M. eds. Rosen’s Emergency Medincine: Concepts and Clinical Practice, 9e Philadelphia, PA: Elsevier; 2018. Link
- Lexow K. Severe accidental hypothermia: survival after 6 hours 30 minutes of cardiopulmonary resuscitation. Arctic Med Res 1991; 50. PMID: 1811563
- Van-der-Ploeg GJ et al.. Accidental hypothermia: rewarming treatments, complications and outcomes from one university medical centre. Resuscitation 2010;, 81(11). PMID: 20702016
- Wang D et al. The J Wave Syndromes and their role in sudden cardiac death. Card Electrophysiol Clin 2011; 3(1): 47-56. PMID: 21499517
Post Peer Reviewed By: Anand Swaminathan, MD (@EMSwami) and Salim R. Rezaie, MD (@srrezaie)
Cite this article as: Anand Swaminathan, "Accidental Hypothermia", REBEL EM blog, October 8, 2018. Available at: https://rebelem.com/accidental-hypothermia/.



