Background: Syncope and presyncope are common presenting complaints to the Emergency Department. Orthostatic vital signs are often included in the ED evaluation of syncope to assess for volume depletion despite their poor performance characteristics as previously discussed. In particular, it is important to understand that older adults often have abnormal orthostatic vitals at baseline, due to numerous causes including medications, despite having a normal physiologic state (Ooi 1997, Aronow 1988). In spite of the evidence, orthostatic vital signs measurements continue to be recommended by the AHA/ACC/HRS guidelines (Shen 2017) and occupy valuable provider and nursing time.
Article: White JL et al. Orthostatic vital signs do not predict 30-day serious outcomes in older emergency department patients with syncope: A multicenter observational study. Am J Emerg Med 2019. PMID: 30928476
Clinical Question: Are the presence of abnormal orthostatic vital signs associated with 30-day serious outcomes in older adults presenting with syncope?
Population: Patients with syncope or near-syncope presenting to 11 academic EDs in the US who were > 60 years of age.
Outcomes:
- Primary: Composite endpoint of 30-day serious events (Significant Dysrhythmia (VF, VT, Sick Sinus Syndrome, Sinus pause > 30 seconds, Mobitz II Heart Block, Complete Heart Block, Symptomatic SVT, Symptomatic Bradycardia), MI, Cardiac Intervention, New Diagnosis of Structural Heart Disease, Stroke, PE, Aortic Dissection, SAH, CPR, Internal Hemorrhage/Anemia Requiring Transfusion, Recurrent Syncope/Fall Resulting in Major Traumatic Injury or Death)
- Secondary: Short-term serious events (occurring during ED or hospital course prior to discharge)
Orthostatic Vital Signs: Defined as systolic blood pressure drop of 20 mm Hg after two minutes of standing OR 10 mm Hg upon standing OR symptoms of dizziness or lightheadedness upon standing
Design: Secondary analysis of a prospective, observational cohort study designed to describe serious outcomes after unexplained syncope
Excluded: Intoxication, medical or electrical intervention to restore consciousness and inability or unwillingness to provide informed consent or follow-up information. Patients with presumptive causes of LOC due to seizure, stroke or TIA and hypoglycemia as well as those that did not have orthostatic vital signs obtained or documented were excluded. The group also excluded patients lost to follow up.
Primary Results:
- Mean Age: 72.1
- Subjects meeting eligibility criteria: n = 6930
- Subjects enrolled: n = 3686 (53.2%)
- Subjects enrolled who had orthostatic vital signs performed: n = 1974 (53.6%)
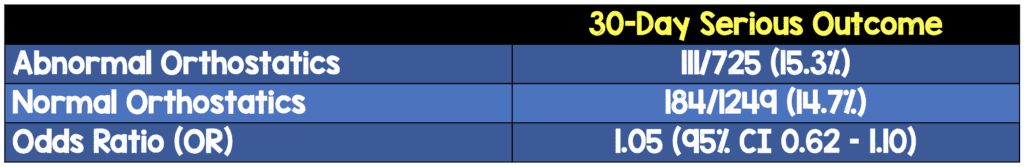
Critical Findings:
- No statistically significant difference in overall adverse outcomes or short-term adverse outcomes
- 30-day mortality: 0.6% (abnormal orthostatics) vs. 0.2% (normal orthostatics) – not significantly different
- Of the 20 different serious outcomes investigated, only 2 were more common in the abnormal orthostatics group:
- GI hemorrhage/anemia: 4.4% vs 2.2%
- Stroke: 1.2% vs 0.4%
Strengths:
- 30-day follow up included: review of the EMR after index visit and phone call assessment of all participants. If phone call revealed a subsequent visit to an outside ED/hospital, those medical charts were obtained and reviewed
- Multivariable logistic regression of composite 30-day serious events was based on pre-specified adjustments of variables based on prior literature suggesting those factors to be important predictors of serious outcomes in patients with syncope
- Research assistants who assessed for 30-day adverse outcomes were blinded to initial clinical course
- The normal vs abnormal orthostatic vital signs groups were well balanced at baseline with the exception of hypotension and an abnormal ECG which were both more common in the abnormal orthostatic vitals group
Limitations:
- The primary goal of this data collection was not to assess outcomes around orthostatic vital signs
- Only 53% of patients who met eligibility were enrolled and only 28% of all eligible patients had orthostatic vital signs measured
- It is unclear if orthostatics were reliably measured by all providers (i.e. did measurements occur after the proper amount of time)
- Patients lost to follow up were excluded from analysis (as opposed to assuming adverse outcome in data analysis)
- Primary outcome was a composite of many outcomes which are not all equal in severity (i.e. death is worse than cardiac intervention)
- Many of the individual outcomes were rare (< 0.5%) making it difficult to tell if there were significant differences
- Serial ECGs were not considered in the evaluation (only the 1st ECG was considered)
- Results of this trial cannot be applied to younger patients or patients excluded from the study
Discussion:
- Attempting to determine which patients are at risk for a 30-day serious outcome is important and may guide clinician management and disposition. However, it should be noted that determining who is at risk isn’t useful unless we know what to do to modify that risk or avoid the outcome. Once we know that a patient is at higher risk, we have to understand what we can offer that patient.
- A substantial number of patients (~ 56%) did not have orthostatic vitals performed
- This group was older, more likely to have CAD, CHF, dyspnea or an abnormal ECG
- Reasons for not obtaining orthostatic vital signs: too symptomatic at baseline (35%), unable to stand (27%), provider determined not indicate (15%), patient refused (11%)
- The absence of obtaining orthostatic vitals may have led to a selection bias and excluded both extremes – those who were too sick to get orthostatics on and those who were too well to need them
Authors Conclusions:
“In a cohort of older adult patients presenting with syncope who were able to have orthostatic vital signs evaluated, abnormal orthostatic vital signs did not independently predict composite 30-day serious outcomes.”
Our Conclusions: Abnormal orthostatic vital signs or symptoms are not associated with an increased risk of adverse outcomes at 30-days.
Potential to Impact Current Practice: This is another study demonstrating the disutility of orthostatic vital sign measurements in the ED. Not only are the performance characteristics poor for predicting mild to moderate volume loss, but they also cannot be used to risk stratify for bad outcomes. While there may be select patients that can benefit from obtaining orthostatic vital signs, they should not be routine for elderly patients presenting with syncope or near-syncope.
Bottom Line: In this secondary analysis of patients aged ≥ 60 years, abnormal orthostatic vital signs do not predict serious 30-day outcomes and should not be used as a routine assessment in syncope.
For More on This Topic Checkout:
- REBEL EM: (Dis)utility of Orthostatic in Volume Depletion
- LITFL: The Futility of Orthostatic Measurements
- REBEL EM: 30-Day Outcomes in Syncope vs Near-Syncope
References:
- Ooi WL et al. Patterns of orthostatic blood pressure change and the clinical correlates in a frail, elderly population. JAMA 1997; 277: 1299-1304. PMID: 9109468
- Aronow WS et al. Prevalence of postural hypotension in elderly patients in a long-term health care facility. Am J Cardiology 1988; 62(4): 336-7. PMID: 3135742
- Shen WK et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. Circulation 2017; 136(5): e25-59. PMID: 28280232
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)



