Early in the pandemic, controversy and anecdote predicated non-invasive strategies to support acute hypoxemic respiratory failure from COVID-19. The debate revolved around the fear of delaying tracheal intubation thus exacerbating lung injury through the generation of large tidal volumes (P-SILI), the risks of nosocomial infection of staff through aerosol generation, or oxygen shortages due to the amount of oxygen required for these non-invasive oxygen systems.
The lack of high-quality evidence led to variability in guidelines and local clinical practice. However, we rely on the highest quality of literature to drive patient management. As such, this is the largest randomized clinical trial to investigate different modes of non-invasive ventilation in COVID-19 patients with respiratory failure.
Paper: An Adaptive Randomized Controlled Trial of Non-Invasive Respiratory Strategies in Acute Respiratory Failure Patients with COVID-19. medRxiv pre-print 2021. [Link is here]
Clinical Question: Does continuous positive airway pressure (CPAP), high flow nasal oxygen (HFNO) therapy, or conventional oxygen therapy prevent intubation or death within 30 days in patients with respiratory failure (<95% on a FiO2 of ≥40%) due to COVID-19?
What They Did:
- Multi-center, parallel-group, open-label, three-arm, adaptive, adaptive, randomized controlled trial performed across 75 hospitals in the UK
- Randomized patients to receive CPAP, HFNO, or conventional oxygen therapy (face mask or nasal cannula) in a 1:1:1 ratio
- Clinicians could randomize to a single intervention (CPAP/HFNO) based on shortage and/or availability of medical equipment
Inclusion Criteria:
- Adult (≥18-years) patients with COVID-19 with acute respiratory failure
- Sp02 of ≤ 94% despite receiving supplemental oxygen Fi02 of at least 0.4
- Suitable for intubation if treatment escalation was needed
Exclusion Criteria:
- Patients in immediate need (<1 hour) of mechanical ventilation
- Pregnancy
- Planned withdrawal of care
- Known contraindication to intervention
Primary Outcomes:
- Composite of:
- Tracheal intubation OR
- Death within 30 days
Secondary Outcomes:
- Incidence of tracheal intubation and death at 30 days
- Time to tracheal intubation
- Duration of mechanical ventilation
- Time to death
- Mortality
- Incidence of ICU admission
- Length of stay
Results:
- 1272 patients randomized across 48 UK hospitals
- Outcome data available for 1259/1272 (99.0%) patients
- Mean age 57.4 years
- Median time from 1st COVID-19 symptoms to randomization was 9d
- Baseline SpO2 92.8%
- Baseline FiO2 0.61
- Crossover occurred in 58/350 (15.3%) of pts in the CPAP arm, 48/417 (11.5%) in the HFNO arm, and 112/475 (23.6%) in the conventional oxygen therapy arm
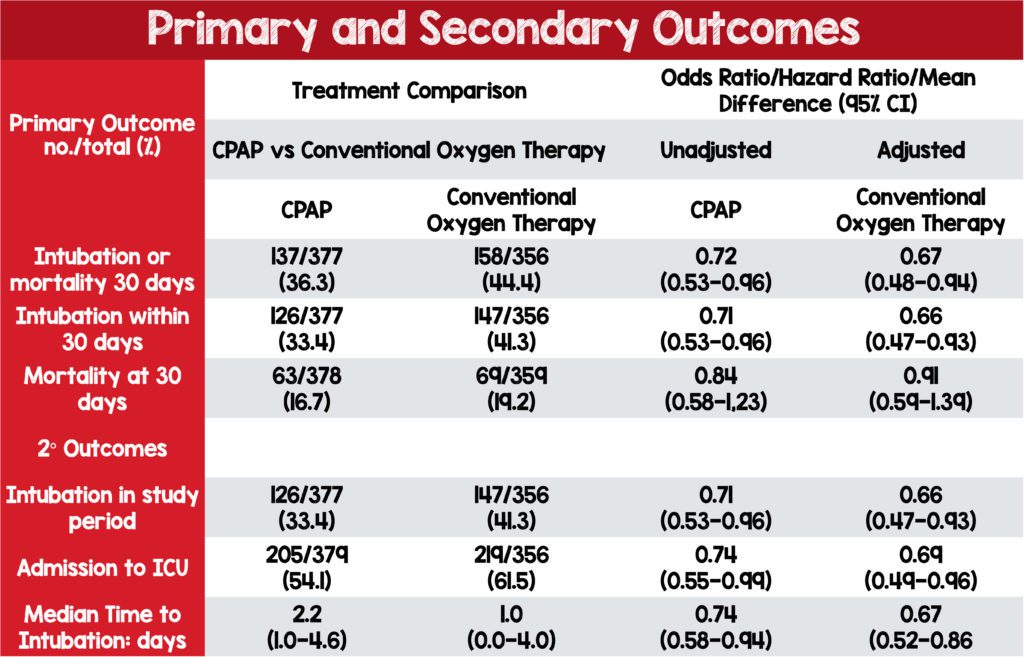
- CPAP vs. conventional oxygen:
- CPAP: 137/377 (36.3%) vs. conventional oxygen: 158/356 (44.4%) were intubated or died within 30 days
- The unadjusted odds ratio 0.72, 95% CI 0.53 to 0.96, P=0.03
- The number needed to treat (NNT) for CPAP was 12 (95% CI, 7 to 105)
- HFNO vs. conventional oxygen:
- HFNO group: 184/414 (44.4%) vs. conventional oxygen: 166/368 (45.1%) were intubated or died within 30 days
- The unadjusted odds ratio 0.97; 95% CI 0.73 to 1.29, P=0.85
- The NNT for HFNO was 151 (95% CI, number needed to treat 13 to number needed to harm 16
- No statistically significant difference in mortality at any point
- In the CPAP group fewer patients required ICU care
- In the CPAP group time to intubation was longer
Safety:
- Safety events were more common in the CPAP group (130/380 or 34.2%). Safety events in HFNO (86/417 or 20.6%) and conventional oxygen therapy (66/475 or 13.9%) p <0.001
- Most common safety events were:
- Hemodynamic instability = 8.5%
- Pneumothorax = 2.0%
- Pneumomediastinum = 1.6%
- 8 serious safety events (7 of which were in the CPAP group) were reported
Strengths:
- Largest RCT of NIV in COVID-19 to date
- Patient characteristics are similar and patients in the intervention and control groups appear to have the same prognosis
- Multi-center, randomized control trial recruited patients at 75 centers of which 45 centers participated
- Outcomes were patient-oriented
- The randomization process was concealed utilizing an internet-based allocation
- Performed an intention-to-treat analysis which analyzed patients in the group they were randomized
- Patient data was available on 99% of patients enrolled
Limitations:
- Patients, clinicians, and outcome assessors were unblinded due to the nature of the trial intervention
- The primary outcome was a composite of tracheal intubation or mortality within 30-days
- These are not equal
- The decision to intubate is subjective.
- There were no defined criteria for when to intubate patients.
- In a non-blinded study, this could lead to bias in the results
- Investigators did not achieve the planned sample size of 4000 patients because recruitment was stopped early
- Trials stopped early can sometimes overestimate results
- A large amount of crossover from conventional oxygen therapy arm to one or both interventions
- This can reduce the observed effect size of clinically effective treatments
- Unable to collect screening data and number of non-randomized patients who met eligibility criteria
- Did not capture information on patient recovery
Discussion:
- Blinding of this study would have been near impossible due to the stark differences in therapy.
- Some patients will perform better simply from the placebo effect, or the perceived benefit of being in the treatment group, in this case, HFNO or CPAP.
- Anecdotally, patients on CPAP often require more frequent management and vent/mask adjustments as the vent alarms ring frequently. This is an important point as it is much easier to do awake proning with HFNO than it is with CPAP.
- There were fewer adverse events with HFNO as well compared to CPAP.
- Additionally, adverse events, though minimal, were more common in the CPAP group, this seems to be consistent with common knowledge of the interventions.
- Again anecdotally, are we more likely to reassess patients we perceive to be on a potentially more dangerous therapy? How does frequent reassessment affect outcomes?
- Treatment escalation to tracheal intubation was not standardized. The investigators discuss the lower rate of tracheal intubation in the CPAP group may have been driven by greater willingness to delay intubation.
- Statistically significant differences in CPAP for the primary outcome can entirely be explained by the decreased need for tracheal intubation.
- There was no difference in mortality seen at any time for any intervention.
- It’s unlikely patients and families would care about intubation if they died anyway.
- There was a considerable amount of crossover from the conventional oxygen therapy group to the CPAP or HFNO group, which may underestimate the benefit of the CPAP and HFNO interventions.
- Additionally, the use of HFNO or CPAP was allowed for “clinical stabilization,” which wasn’t further defined but seems like treatment failure.
- Tracheal intubation and 30-day mortality are pragmatic, patient-oriented outcomes during a pandemic when resources may be scarce. Decreasing and even delaying intubation may provide a substantial benefit and allow the care team time to plan appropriate resource allocation at a time when hospitals may be strapped for medical equipment.
- We do not know the number of patients who were eligible but not selected for randomization which leads to selection bias.
- The study was stopped early due to the reducing numbers of COVID-19 and ethical obligations to share data.
- This seems interesting in light of multiple waves of pandemic and the fact that patients was eligible for recruitment from 75 hospitals
- Truncated RCTs are at risk for overestimating treatment effects.
- Ferreyro BL et al. 2020 [Link is here] performed a Systematic Review and Meta-analysis they looked at 25 RCTs (3800pts) in acute respiratory failure showed
- NIV reduced the incidence of both tracheal intubation and mortality
- HFNO reduced incidence of tracheal intubation, BUT not mortality
- The current trial was not powered to determine a difference in mortality
- Discordant findings could be explained by:
- Differences in the pathophysiology of COVID19 vs other causes of acute respiratory failure
- Location of patients. CPAP and HFNO outside of a critical care unit could influence the effectiveness of both interventions
Author’s Conclusion: “In conclusion, in this randomized trial of hospitalized adults with acute respiratory failure due to COVID-19, CPAP, compared with conventional oxygen therapy, reduced the composite outcome of tracheal intubation or death within 30 days of randomisation in hospitalized adults with acute respiratory failure due to COVID-19. There was no effect observed, compared with conventional oxygen therapy, with the use of HFNO.”
Clinical Bottom Line:
For patients with COVID-19 pneumonia and acute hypoxemic respiratory failure, CPAP reduced the need for intubation compared to conventional oxygen therapy. However, HFNO did not reduce the need for intubation compared to conventional oxygen therapy. Neither intervention showed a statistically significant mortality benefit compared to conventional oxygen therapy, however, the study was not powered for this outcome. Although the conclusion of the trial is CPAP > HFNO > COT, there may be some scenarios where HFNO > CPAP to reduce adverse events (i.e awake prone positioning, patient nutrition, etc).
More FOAMed:
- St. Emlyn’s Blog: JC – Non-Invasive Ventilation for COVID-19 Patients. The RECOVERY-RS Trial
- The Bottom Line: RECOVERY-RS
- Critical Care Reviews: RECOVERY-RS Trial Results
References:
- Guyatt G, Rennie D, Meade M, Cook D. Users’ Guides To The Medical Literature. 3rd ed. McGraw-Hill Education; 2015. [Link is here]
- Ferreyro BL, Angriman F, Munshi L, et al. Association of Noninvasive Oxygenation Strategies With All-Cause Mortality in Adults With Acute Hypoxemic Respiratory Failure: A Systematic Review and Meta-analysis. JAMA 2020. [Link is here]
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)