The authors of GRACE highlight the clinical questions faced by emergency medicine physicians every day:
- 1) Does a revisit represent a previously missed diagnosis?
- 2) Does the revisit warrant an escalation in the diagnostic approach?
- 3) What if the patient has already had what can be considered a recent, reasonable, and thorough diagnostic evaluation?
- 4) How long is this prior evaluation valid?
Paper:
Musey PI Jr, Bellolio F, Upadhye S, et al. Guidelines for reasonable and appropriate care in the emergency department (GRACE): Recurrent, low-risk chest pain in the emergency department [published online ahead of print, 2021 Jul 6]. Acad Emerg Med. 2021. [PMID: 34228849]
Clinical Questions:
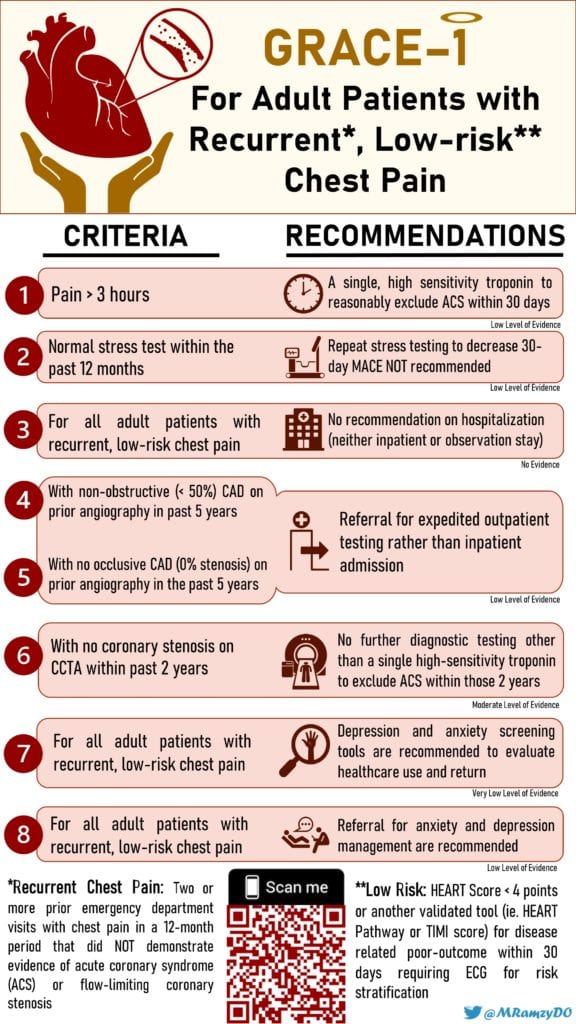
In adult patients with recurrent, low-risk chest pain…
- Is a single troponin vs serial troponins needed for ACS outcomes within 30 days?
- With normal or nondiagnostic stress testing within the last 12 months, does repeat stress testing vs no stress test have an effect on MACE within 30 days?
- How does admission to the hospital vs stay in the ED observation unit vs outpatient follow-up for ACS affect outcomes within 30 days?
- If a patient has a negative cardiac catheterization, defined as less than 50% stenosis, what is the risk of subsequent ACS and time to ACS?
- If a patient has a negative cardiac catheterization, defined as noncoronary disease (0% stenosis), what is the risk of subsequent ACS and time to ACS?
- If a patient has a negative coronary CT angiogram what is their risk of subsequent ACS and time to ACS?
- What is the yield of depression and anxiety screening tools in healthcare use and return to ED visits?
- What is the role of referral for anxiety/depression in healthcare use and return to ED visits?
What They Did:
- Multidisciplinary panel of ED physicians, cardiologists, three methodologists, and a patient representative used The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach to assess evidence
- Performed a comprehensive search of several databases from inception to August 16, 2019
- 5,252 articles were found during search and reviewed for possible inclusion
- 334 articles retrieved
- 44 supplied by content experts 38 were included
- Formulated 8 evidence-based recommendations for adults with recurrent low-risk chest pain based on available literature
HOW TO APPROACH GUIDELINES
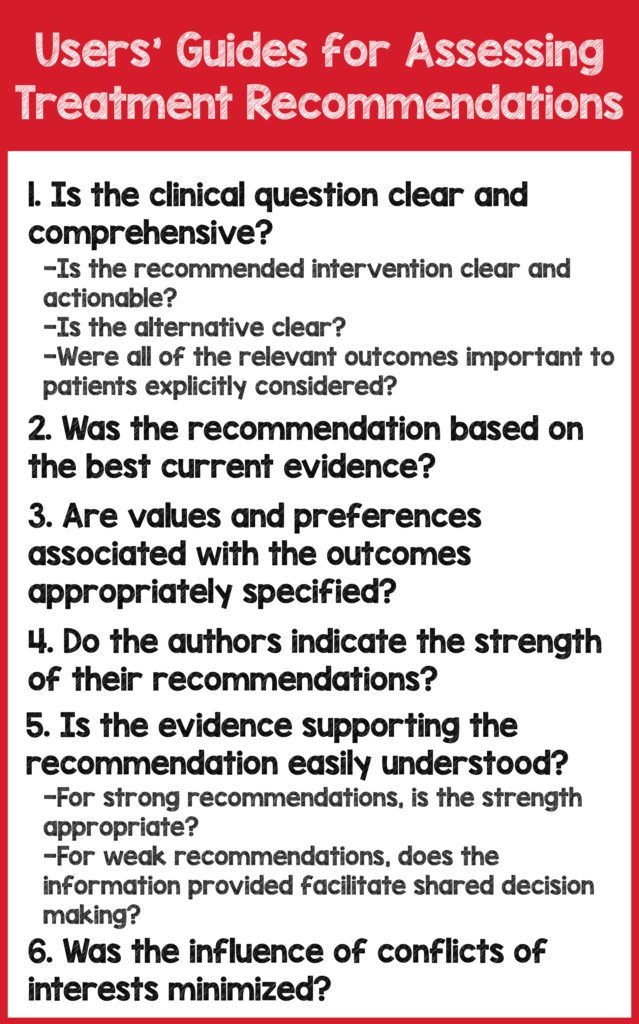
Adapted from: Guyatt G, Rennie D, Meade M, Cook D. Users’ Guides To The Medical Literature. 3rd ed. McGraw-Hill Education; 2015. [Link is here]
KEY DEFINITIONS
- Recurrent Chest Pain: patients with a previous ED visit with chest pain that
- led to a diagnostic protocol for its evaluation
- AND did not demonstrate evidence of ACS or flow-limiting coronary stenosis
- Included 2 or more ED visits for chest pain in a 12-month period
- Expedited follow up: 3-5 days
- Low-risk defined by HEART score <4 pts, HEART pathway, or TIMI score, specifically with regard to the risk for ACS or MACE in ED patients with recurrent chest pain
- MACE: Acute MI, need for PCI or CABG, and death
Recommendations:
- Recommendation 1: In adult patients with recurrent, low-risk chest pain, for greater than 3 hours duration we suggest a single, high-sensitivity troponin below a validated threshold to reasonably exclude ACS within 30 days. (Conditional, For) [Low level of evidence]
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Draw a single 3-hour troponin on low-risk patients with recurrent chest pain
- Low risk and recurrent chest pain are defined above
-
- Is the alternative clear?
-
- YES—Compares a single troponin versus serial troponins
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- YES—Looked at 30-day MACE which is a standard patient-oriented outcome for ACS
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor
-
- Does the information provided facilitate shared decision-making?
-
- YES—There were no studies available for low-risk patients with recurrent pain
- The recommendation is derived from 9 studies with low-risk chest pain
- 72/15,715 patients had MACE (0.5%)
- Strength of recommendation is appropriate given the lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- The paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 2: In adult patients with recurrent, low-risk chest pain, and a normal stress test within the previous 12 months, we do not recommend repeat routine stress testing as a means to decrease rates of MACE at 30 days. (Conditional, Against) [Low level of evidence]
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Do not perform a stress test on low-risk patients with recurrent chest pain
-
- Is the alternative clear?
-
- YES—Repeat stress test vs no stress test
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- YES and NO—One paper looked at 30-day MACE which is a standard patient-oriented outcome for ACS.
- Other paper reviewed looked “cardiac events”
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor
-
- Does the information provided facilitate shared decision-making?
-
- YES—There were no studies available for low-risk patients with recurrent pain and no direct evidence
- 2 Indirect studies focused on non-high-risk chest pain
- Not recurrent chest pain
- No recent testing
- Studies used “cardiac events” at 30d, not MACE
- Outpatient study looked at recent ED discharges who completed stress test in 3 days, 4-30 days, or not at all
- Looked at MACE
- Not recurrent chest pain
- In total, from all studies, 0/4906 patients (0%) died at 30 d
- 91/4906 (1.9%) experienced nonfatal significant cardiac event
- Strength of recommendation is appropriate given the lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 3: In adult patients with recurrent, low-risk chest pain, there is insufficient evidence to recommend hospitalization (either standard inpatient admission or observation stay) versus discharge as a strategy to mitigate major adverse cardiac events within 30 days. (No evidence, Either)
- Discussion: There was no evidence to support or refute
- Recommendation 4: In adult patients with recurrent, low-risk chest pain and non-obstructive (<50% stenosis) CAD on prior angiography within 5 years, we suggest referral for expedited outpatient testing as warranted rather than admission for inpatient evaluation. (Conditional, For) [Low level of evidence]
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Do not admit adult patients with recurrent, low-risk chest pain
- Patients should instead be referred for expedited (3-5 days) outpatient follow up
-
- Is the alternative clear?
-
- YES—Admission for inpatient testing vs. discharge with expedited outpatient follow up
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- YES—Looked at all-cause mortality and nonfatal MI within 5 years
- Did not look at MACE
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor
-
- Does the information provided facilitate shared decision-making?
-
- YES—One meta-analysis and a few retrospective observational studies
- Meta-analysis included 54 studies with 35,039 patients, 99,770 person-years of follow up
- Looked at non-obstructive CAD (<50%) vs. 0% stenosis
- All-cause mortality and non-fatal MI for patients with <50% stenosis: 1.32 cases per 100 patients followed for one year
- Observational Studies did not separate 0% vs <50%
- Strength of recommendation is appropriate given lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 5: In adult patients with recurrent, low-risk chest pain and no occlusive CAD (0% stenosis) on prior angiography within 5 years, we recommend referral for expedited outpatient testing as warranted rather than admission for inpatient evaluation. (Conditional, For) [Low level of evidence].
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Do not admit adult patients with recurrent, low-risk chest pain and 0% stenosis on prior angiography within 5 years
- Patients should instead be referred for expedited (3-5 days) outpatient follow up
-
- Is the alternative clear?
-
- YES—Admission for inpatient testing vs. discharge with expedited outpatient follow up
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- YES—Looked at all-cause mortality and nonfatal MI within 5 years
- Did not look at MACE
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor
-
- Does the information provided facilitate shared decision-making?
-
- YES—One meta-analysis and a few retrospective observational studies
- Meta-analysis included 54 studies with 35,039 patients, 99,770 person-years of follow up
- Looked at non-obstructive CAD (<50%) vs. 0% stenosis
- All-cause mortality and non-fatal MI for patients with 0% stenosis: 0.52 cases are expected for 100 patients followed for 1 year
- Strength of recommendation is appropriate given lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 6: In adult patients with recurrent, low-risk chest pain and prior CCTA within the past two years with no coronary stenosis, we suggest no further diagnostic testing other than a single, high-sensitivity troponin below a validated threshold to exclude ACS within that two-year time frame. (Conditional, For) [Moderate level of evidence]
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Do not perform additional testing beyond a single high-sensitivity troponin in patients with a normal CCTA within the last 2 years
-
- Is the alternative clear?
-
- YES—Any additional testing beyond high-sensitivity troponin vs. no additional testing
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- YES—18 papers looked at long-term coronary events
- 2 large studies, CONFIRM Registry and PROMISE Trial
- Looked at MACE and cardiovascular death and MI
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor with a moderate level of evidence
-
- Does the information provided facilitate shared decision-making?
-
- YES—CONFIRM Registry
- Patients with normal (0% stenosis) CCTA had a rate of MI 0.08%, all-cause mortality of 0.4%, and MACE rate 0.6% at 2 years
- Patients with 1-49% stenosis on CCTA had a rate of MI 1.3%, all-cause mortality of 0.5%, and MACE rate of 2.4% at 2 years
- PROMISE Trial
- Patients with normal (0% stenosis) CCTA had a rate of cardiovascular death and MI of 0.3% at 26 months
- Patients with 1-49% stenosis on CCTA had a rate of cardiovascular death and MI of 1.6%
- Neither study addressed recurrence
- Strength of recommendation is appropriate given the lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 7: In adult patients with recurrent, low-risk chest pain, we suggest the use of depression and anxiety screening tools as these might have an effect on healthcare use and return ED visits. (Conditional, Either) [Very low level of evidence]
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Use of depression and anxiety screening tools In adult patients with recurrent, low-risk chest pain,
-
- Is the alternative clear?
-
- NO—The absence of a direct alternative or comparator can cause variation in interpretations and lead to confusion.
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- NO—The papers reviewed focused exclusively on anxiety and depression
- There are many psychosocial factors that can contribute to ED utilization including other psychiatric disorders, homelessness, substance use disorder
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation in favor with a very low level of evidence
-
- Does the information provided facilitate shared decision-making?
-
- NO—6 studies were reviewed for depression, anxiety, and ED recurrence
- There was no direct evidence
- Depression study of 365 showed that low-moderate risk patients in the observation unit for chest pain who screened positive for clinically significant depression were at increased risk for chest pain recurrence and increased ED return visits
- Data from anxiety studies were conflicting
- Data from ED recurrence studies were conflicting
- Anecdotally this may make sense, though in practice it does not seem feasible to apply shared decision making to mental health screening tools
- Strength of recommendation is appropriate given the lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
- Recommendation 8: In adult patients with recurrent, low-risk chest pain, we suggest referral for anxiety or depression management, as this might have an impact on healthcare use and return ED visits. (Conditional/Either) [Low level of evidence].
- Discussion: Is the recommendation clear, comprehensive, and actionable?
-
- YES—Refer patients with recurrent, low-risk chest pain for management of anxiety or depression
-
- Is the alternative clear?
-
- NO—The absence of a direct alternative or comparator can cause variation in interpretations and lead to confusion.
-
- Were all of the relevant outcomes important to patients explicitly considered?
-
- NO—The papers reviewed focused exclusively on anxiety and depression
- There are many psychosocial factors that can contribute to ED utilization including other psychiatric disorders, homelessness, substance use disorder
-
- Are values and preferences associated with the outcomes appropriately specified?
-
- NO—Values and preferences not specifically specified for this guideline but mentioned in total
-
- Do the authors indicate the strength of their recommendations?
-
- YES—Conditional recommendation for either with a very low level of evidence
-
- Does the information provided facilitate shared decision-making?
-
- NO—2 systematic reviews were available with indirect evidence
- There was no direct evidence
- 17 RCTs with 1,006 pts with symptomatic management of nonspecific chest pain in patients with normal coronary anatomy
- Interventions: CBT, relaxation therapy, hyperventilation control, psychotherapy, hypnotherapy
- Reduction in chest pain in first 3 months [RR 0.70, 95% CI 0.53 to 0.92]
- Increase the number of chest pain-free days up to 3 months [MD 3.00; 95% CI 0.23 to 5.77]
- Reduced chest pain frequency [MD -2.26; 95% CI -4.41to -0.12]
- 7 RCTs of 319 patients
- Association between antidepressants and pain reduction [SMD -1.26; 95% CI -2.34 to -0.19]
- Strength of recommendation is appropriate given the lack of evidence
-
- Was the influence of conflict of interest (COI) minimized?
-
- YES—Conflicts were reviewed by a COI review group
- All members of the panel complied
- The chair and all members were reviewed by SAEM executive board and determined not to have and COI
- the paper was independently funded by SAEM
-
- Discussion: Is the recommendation clear, comprehensive, and actionable?
Strengths
- Attempts to answer a clinically important dilemma faced regularly by emergency medicine physicians
- Multidisciplinary panel included content experts, physicians, methodologists, and patient representatives
- Independently funded by SAEM
- Performed a comprehensive literature search
- Clinical guidelines were pragmatic and easily applicable to real-world EM clinical practice.
- Reinforces the importance of shared decision making with our patients
Limitations
- Guidelines are based on limited and often indirect evidence
- Guidelines are often based on a low level of evidence
- Often no studies were available that addressed recurrent chest pain
- Data derived from the literature was mostly derived from high-sensitivity troponin studies
- Some clinical settings may still be utilizing conventional troponins
- Most studies reviewed regarding stress testing did not define all parameters for a normal or negative stress test
- Expedited outpatient follow-up is likely more difficult in clinical settings with higher populations of uninsured and underinsured
- Some anxiety screening tools are cumbersome and may be time-consuming in clinical practice
DISCUSSION
These guidelines are comprehensive and pragmatic. However, they highlight how little evidence exists on recurrent low-risk chest pain and patient values and preferences for low-risk recurrent chest pain treatment. This lack of data represents an opportunity for future research to illuminate some gaps in knowledge. Also, of worthy discussion, some hospitals do not have high-sensitivity troponins. Therefore, some guidelines may not be applicable in all clinical settings. Likewise, expedited outpatient follow-up may also be difficult for some. Underinsured and uninsured patients are particularly vulnerable to follow-up loss. Accordingly, we often practice more cautiously with patients with limited resources. Moreover, the recommendations are based on derivative, indirect evidence stressing the importance of shared-decision making with our patients.
Clinical Bottom Line:
GRACE guidelines offer a pragmatic, evidence-based framework for shared-decision making in patients with recurrent low-risk chest pain.
References
- National Hospital Ambulatory Medical Care Survey: 2017 emergency department summary tables. National Center for Health Statistics, 2020. [Link is HERE]
- Fleet RP, Lavoie KL, Martel JP, Dupuis G, Marchand A, Beitman BD. Two-year follow-up status of emergency department patients with chest pain: Was it panic disorder? Cjem 2003;5:247-54. [PMID: 17472767]
- Guyatt G, Rennie D, Meade M, Cook D. Users’ Guides To The Medical Literature. 3rd ed. McGraw-Hill Education; 2015. [Link is HERE]
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)