What They Did:
- The European Society of Intensive Care Medicine and The Society of Critical Care Medicine convened a task force of 19 critical care, infectious disease, surgical, and pulmonary specialists in Jan 2014
- When compiled, the task force recommendations with supporting evidence, including original research, were circulated to major international societies and other relevant bodies for peer review and endorsement (31 endorsing societies)
Issues Addressed:
- Differentiation of sepsis from uncomplicated infection
- Update definitions of sepsis and septic shock
- Recognition that sepsis is a syndrome without at present, a validated criterion standard diagnostic test, leading to major variations in reported incidence and mortality rates
- Identify clinical criteria that identify all the elements of sepsis (infection, host response, and organ dysfunction). This should be simple to obtain, available promptly and at a reasonable cost.
- Provide a more consistent and reproducible picture of sepsis incidence and outcomes.
Identified Challenges and Opportunities:
- There is no gold standard diagnostic test that exists to diagnose sepsis. Instead it is a constellation of clinical signs and symptoms in a patient with suspected infection.
- The original concept of sepsis as infection with at least 2 of the 4 SIRS criteria focused solely on inflammatory excess, but may also be present in the absence of infection entirely.
- The use of 2 or more SIRS criteria to identify sepsis was unanimously considered by the task force to be unhelpful. In addition, it has been shown that 1 in 8 patients admitted to critical care units with infection and new organ failure will not have a minimum of 2 SIRS criteria to fulfill the definition of sepsis.
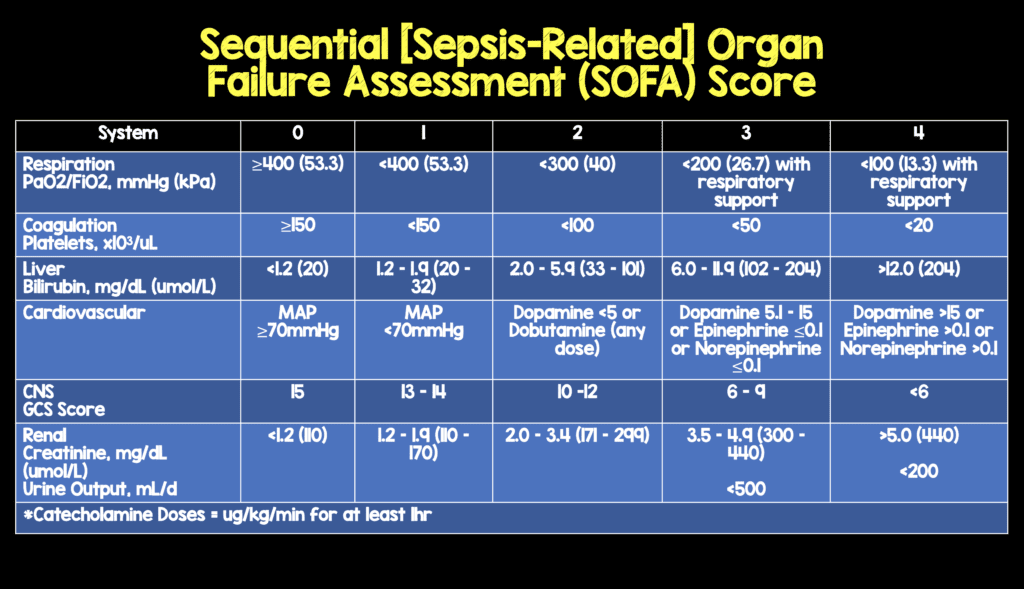
- Severity of organ dysfunction has been assessed with various scoring systems, however the predominant score in current use is the Sequential Organ Failure Assessment (SOFA) Score. Simply put the higher the SOFA score, the increased probability of mortality. The score does require many laboratory variables including PaO2, platelet count, creatinine level, and bilirubin for full computation.
Results/Recommendations:
- Sepsis is now defined as life-threatening organ dysfunction caused by a dysregulated host response to infection
- Organ dysfunction can be identified as an acute change in total SOFA score ≥2 points due to the infection (The baseline SOFA score can be assumed to be zero in patients not known to have preexisting organ dysfunction)
- A SOFA score ≥2 reflects an overall mortality risk of approximately 10% in a general hospital population with suspected infection
- Screening Patients Likely to Have Sepsis: Patients with suspected infection that are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at bedside with qSOFA (i.e. Altered mental status, systolic blood pressure ≤100mmHg, or respiratory rate ≥22/min). The qSOFA score is less robust than a SOFA score of 2 or greater, but it does not require laboratory tests and can be assessed quickly and repeatedly.

- Septic Shock: Patients with septic shock can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain MAP ≥65mmHg and having a serum lactate level >2mmol/L (18mg/dL) despite adequate volume resuscitation. With these criteria, hospital mortality is in excess of 40%
Controversies/Limitations:
- Sepsis is a broad term being applied to an incompletely understood process, therefore pragmatic compromises were necessary placing emphasis on generalizability
- Initial retrospective analysis showed that qSOFA could be a useful clinical tool for screening of sepsis. It only uses clinical examination findings, but still needs prospective validation to confirm its robustness and possible incorporation into future iterations of the sepsis definitions.
- Neither qSOFA nor SOFA are intended to be a stand-alone definition of sepsis and that failure to meet 2 or more qSOFA or SOFA criteria should not defer investigation or treatment of infection or delay any other aspect of clinical care
- Some of the task force argued that lactate measurement should be mandated as an important biochemical identifier of sepsis in an infected patient. Since lactate measurement was not listed alongside the simple bedside criteria, should not constrain the monitoring of lactate as a guide to therapeutic response or as an indicator of illness severity.
- The focus of this update of definitions was in adult patients, and there is still a need to develop similar updated definitions for pediatric populations
- This document was not endorsed by all societies (i.e. Latin American Sepsis Institute, American College of Chest Physicians, and American College of Emergency Physicians)
- There were no members from the low- and middle-income countries on the task force, which is important as they had minimal input and sepsis care is different in these settings.
Discussion:
- Lactate level is a sensitive, but nonspecific, stand-alone indicator of cellular or metabolic stress rather than “shock.” But the combination of hyperlactatemia with fluid-resistant hypotension identifies a group with particularly high mortality and thus offers a more robust identifier of the physiologic and epidemiologic concept of septic shock than either criterion alone.
- SIRs is non-specific and now no longer used for sepsis recognition/screening, but patients with SIRs criteria are still potentially critically ill patients.
Operationalization of New Sepsis and Septic Shock Criteria:

Authors Conclusions: “These updated definitions and clinical criteria should clarify long-used descriptors and facilitate earlier recognition and more timely management of patients with sepsis or at risk of developing it. This process, however, remains a work in progress. As is done with software and other coding updates, the task force recommends that the new definition be designated Sepsis-3. With the 1991 and 2001 iterations being recognized as Sepsis-1 and Sepsis-2, respectively, to emphasize the need for future iterations.”
Clinical Take Home Points:
- Sepsis = life-threatening organ dysfunction caused by a dysregulated host response to infection
- Septic Shock = Need for Vasopressors AND Lactate >2 mmol/L
- Severe Sepsis is OUT
- SIRS is OUT and qSOFA/SOFA are IN
References:
- Singer M et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315(8): 801 – 810. [epub ahead of print]
For More Thoughts on This Topic Checkout:
- Jeremy Faust and Lauren Westafer at FOAMCast: Sepsis – Redefined
- Richard Carden and Natalie May at St. Emlyn’s Blog: Holy Smokes! Batman, the SOFA and the Latest Sepsis Definitions
- Justin Morgenstern at First 10 in EM: Sepsis 3.0?
- Josh Farkas at Pulmcrit/EMCrit: Top 10 Problems with the new Sepsis Definition
- Intensive Care Medicine Working Knowledge (ICMWK): Sepsis 3 – The Rise of the SOFA
- Scott Weingart at EMCrit: Sepsis 3.0 with Melv Singer
- Scott Weingart at EMCrit: Wee – Cliff Deutschman with Additional Thoughts on Sepsis 3.0
- Matthew MacPartlin at Intensive Care Network: Sepsis is Not a Disease
- Josh Farkas at PulmCrit(EMCrit): Bad news for Sepsis-3.0: qSOFA Fails Validation
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)



