 Background: Over the past few years there has been a shift in cardiac arrest from the mantra of ABC (Airway, Breathing, Circulation) to CAB (Circulation, Airway, Breathing). There has been increased emphasis on circulation and a de-emphasis of airway management in cardiac arrest. Physiologically, this makes sense as the only two interventions in cardiac arrest that have been shown to make a difference in neurological outcomes are early, high quality CPR and defibrillation. The reason for this is increased coronary and cerebral perfusion pressure, which improve oxygenation to ischemic tissue. The less ischemic cardiomyocytes are the more likely they will convert to a perfusing rhythm. Similarly, the less ischemic neurons are, the more likely we will have a better neurologic outcome for our patients. It has been fairly well established in the peer reviewed literature that advanced airway management in the prehospital setting is associated with decreased survival with good neurologic outcome. There is considerably less literature exploring this area in in-hospital cardiac arrest.
Background: Over the past few years there has been a shift in cardiac arrest from the mantra of ABC (Airway, Breathing, Circulation) to CAB (Circulation, Airway, Breathing). There has been increased emphasis on circulation and a de-emphasis of airway management in cardiac arrest. Physiologically, this makes sense as the only two interventions in cardiac arrest that have been shown to make a difference in neurological outcomes are early, high quality CPR and defibrillation. The reason for this is increased coronary and cerebral perfusion pressure, which improve oxygenation to ischemic tissue. The less ischemic cardiomyocytes are the more likely they will convert to a perfusing rhythm. Similarly, the less ischemic neurons are, the more likely we will have a better neurologic outcome for our patients. It has been fairly well established in the peer reviewed literature that advanced airway management in the prehospital setting is associated with decreased survival with good neurologic outcome. There is considerably less literature exploring this area in in-hospital cardiac arrest.
What They Did:
- A US multicenter, retrospective, observational cohort study of adult patients with an in-hospital cardiac arrest from the Get With the Guidelines Registry (GWTG-R), a prospective quality improvement registry of in-hospital cardiac arrest in US hospitals
- Patients intubated in the first 15 minutes of resuscitation were matched with patients at risk of being intubated, but not intubated in the first 15 minutes still receiving resuscitation
Definitions:
- Tracheal Intubation: Insertion of a tracheal or tracheostomy tube during cardiac arrest
- Time to Tracheal Intubation: The interval from loss of pulses until tracheal tube was inserted
- All times in the GWTG-R are recorded as whole minutes, therefore a time of 0 minutes indicates that the tracheal intubation was performed in the same minute that the pulses were lost
Outcomes:
- Primary Outcome: Survival to Hospital Discharge
- Secondary Outcomes:
- Return of Spontaneous Circulation (ROSC)
- Good Functional Outcome (Cerebral Performance Category of 1 or 2)
Inclusion:
- Age ≥18 years of age
- Index cardiac arrest in which chest compressions required
Exclusion:
- Invasive airway already in place at time of cardiac arrest (i.e. tracheal tube, tracheostomy, laryngeal mask airway, or other invasive airways not including nasopharyngeal or oropharyngeal airways)
- Hospital visitors and employees
- Patients missing data on tracheal intubation, covariates (except race), and survival
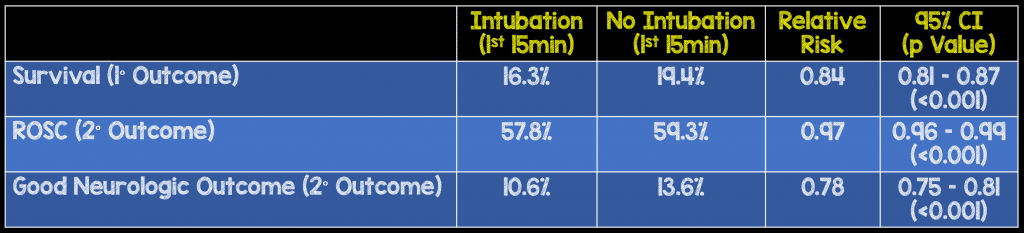
Results:
- Propensity-matched cohort selected from >108k patients from 668 hospitals
- 24,256 patients (22.4%) survived to hospital discharge
- 71,615 patients (66.3%) were intubated within first 15 minutes
- 67,540 patients (62.5%) achieved ROSC
- 16,504 patients (16%) had good neurologic outcome
- 43,314 patients were matched to a patient not intubated in the same minute
Strengths:
- Used a time-dependent propensity score matching and accounts for the fact that intubation might not occur during the cardiac arrest if ROSC or termination of efforts occurs first
- Study also tested whether association between tracheal intubation and survival to hospital discharge differed in pre-specified subgroups (i.e. shockable vs non-shockable rhythms), timing of matching (0 – 4, 5 – 9, 10 – 15min), illness category, preceding respiratory insufficiency, and location of event
Limitations:
- Unsuccessful intubation attempts were not registered as intubations in the registry.
- This study is not randomized so it’s unclear why intubation was undertaken in some patients and not in others
- Abstractors assessing outcomes not blinded to exposure status, but were unaware of the hypothesis of the study
- More patients in the intubation group were on a floor without telemetry (30% vs 17%) and more patients not intubated were in the ICU (48% vs 30%) which could be confounders in this study
- Epinephrine was more likely to be given in the intubation group (95% vs 76%). Studies on epinephrine have shown increased ROSC, but not necessarily improved survival or neurological outcomes
- Quality of CPR not documented, which is one of the most important interventions for neurologically intact survival
- As this was a registry trial, times may have been documented incorrectly
- At least one variable required for this study was missing in 25% of the patients included in the study
Discussion:
- Interestingly, there was a lower likelihood of survival in patients with an initial shockable rhythm intubated in the first 15 minutes (RR 0.68/ 95% CI 0.65 – 0.72) compared to patients without an initial non-shockable rhythm intubated in the first 15 minutes (RR 0.91; 95% CI 0.33 -0.94)
- Another interesting point is patients without preexisting respiratory insufficiency intubated in the first 15 minutes also had an association with lower likelihood of survival (RR 0.78; 95% CI 0.75 – 0.81), but there was no association with patients who did have a preexisiting respiratory insufficiency (RR 0.97; 95% CI 0.91 – 1.02)
- There are several potential reasons why tracheal intubation performed in the first 15 minutes of an in-hospital cardiac arrest have worsened neurologic outcomes:
- Prolonged interruptions of chest compressions
- Hyperventilation and hyperoxia
- Delay other interventions such as defibrillation
- Unrecognized esophageal intubation
- 10% of the patients included in each cohort were located in the emergency department
- In my practice during a cardiac arrest that is not already intubated, my focus is on coronary and cerebral perfusion pressure. Therefore, I frequently will either BVM or LMA intra-arrest and then intubate after successful ROSC.
Author Conclusion: “Among adult patients with in-hospital cardiac arrest, initiation of tracheal intubation within any given minute during the first 15 minutes of resuscitation, compared with no intubation during that minute, was associated with decreased survival to hospital discharge. Although the study design does not eliminate the potential for confounding by indication, these findings do not support early tracheal intubation for adult in-hospital cardiac arrest.”
Clinical Take Home Point: As there are currently no RCTs evaluating intubation during the first 15 minutes of an in-hospital cardiac arrest, this study may be some of the current best evidence that supports focusing on the interventions that matter most early on: High-Quality CPR and Defibrillation.
For More On This Topic Checkout:
- David Harvie at The Bottom Line: Association Between Tracheal Intubation During In-Hospital Cardiac Arrest and Survival
- Ken Milne at The SGEM: SGEM #197 – Die Trying – Intubation of In-Hospital Cardiac Arrests
References:
- Anderson, LW et al. Association Between Tracheal Intubation During Adult In-Hospital Cardiac Arrest and Survival. JAMA 2017. 317(5): 494 – 506. PMID: 28118660
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)