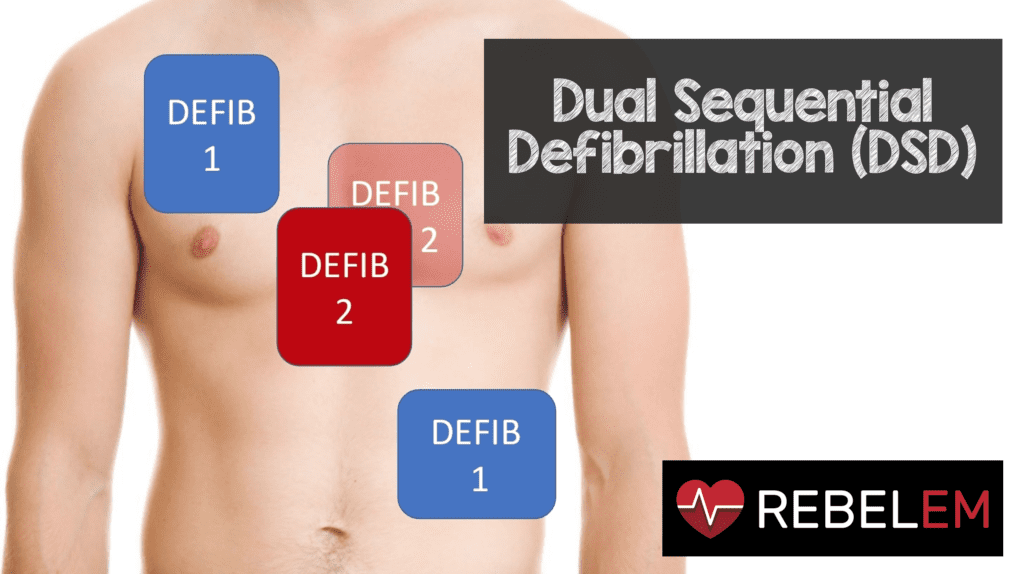
 Background: In the United States 424,000 out of hospital cardiac arrests occur per year with a 10.4% overall survival rate.1 Refractory Ventricular Fibrillation (RVF) is a complication of cardiac arrest and has varying definitions in the literature but is commonly defined as ventricular fibrillation that does not respond to, or resists, three or more defibrillation attempts.2,3Although the estimated incidence of refractory ventricular fibrillation is 0.5-0.6 per 100,000 of the population, some authors report that 10-25% of cardiac arrest cases could develop RVF or recurrent VF.3-5 Patients who experience RVF during their cardiac arrest have a mortality of up to 97%.6,7 Several case reports have shown success with excellent neurologic outcomes in terminating RVF using dual defibrillation after failure of traditional Advance Cardiac Life Support (ACLS) measures.8-12 It is important to note and distinguish that dual defibrillation can either be simultaneous or sequential depending on the duration of the defibrillation potential as well as the intershock interval between the two defibrillator shocks.9-13 The terms “sequential” and “simultaneous” are often used interchangably due to the lack of accurately measuring pulse intervals when performing dual defibrillation in the actual clinical environment. The authors of this review utilize the term dual sequential defibrillation (DSD). They present a case of RVF in a patient with cardiac arrest, on whom DSD was successful in reversion to sinus rhythm and provide a thorough review of similar cases in the literature.
Background: In the United States 424,000 out of hospital cardiac arrests occur per year with a 10.4% overall survival rate.1 Refractory Ventricular Fibrillation (RVF) is a complication of cardiac arrest and has varying definitions in the literature but is commonly defined as ventricular fibrillation that does not respond to, or resists, three or more defibrillation attempts.2,3Although the estimated incidence of refractory ventricular fibrillation is 0.5-0.6 per 100,000 of the population, some authors report that 10-25% of cardiac arrest cases could develop RVF or recurrent VF.3-5 Patients who experience RVF during their cardiac arrest have a mortality of up to 97%.6,7 Several case reports have shown success with excellent neurologic outcomes in terminating RVF using dual defibrillation after failure of traditional Advance Cardiac Life Support (ACLS) measures.8-12 It is important to note and distinguish that dual defibrillation can either be simultaneous or sequential depending on the duration of the defibrillation potential as well as the intershock interval between the two defibrillator shocks.9-13 The terms “sequential” and “simultaneous” are often used interchangably due to the lack of accurately measuring pulse intervals when performing dual defibrillation in the actual clinical environment. The authors of this review utilize the term dual sequential defibrillation (DSD). They present a case of RVF in a patient with cardiac arrest, on whom DSD was successful in reversion to sinus rhythm and provide a thorough review of similar cases in the literature.
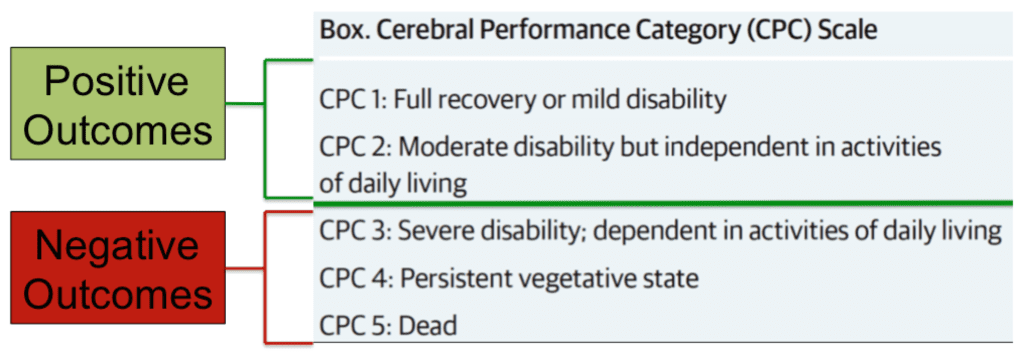
Clinical Question: Does dual sequential defibrillation(DSD) lead to more successful conversion of refractory ventricular fibrillation, return of spontaneous circulation (ROSC) or improved Cerebral Performance Category (CPC) Scores?
Inclusion Criteria:
- Published papers found using the following search terms:
- “Heart Arrest”
- “Electric Countershock”
- “Ventricular Fibrillation”
- “Out-of-hospital Cardiac Arrest”
- “Double Sequential Defibrillation”
- “Refractory Ventricular Fibrillation”
- “Dual Shock”
- “Dual Defibrillation”
- “Double Simultaneous Defibrillation”
Exclusion Criteria:
- Lack of dual defibrillation
- Lack of refractory ventricular fibrillation
- Language other than English
Results:
- 12 published papers describing a total of 38 cases
- One paper had 10 cases, another had 12, another had 7
Critical Results:
- 77% of the 39 had their VF successfully terminated with DSD
- 54% had ROSC
- 28% had a CPC <2 at discharge from the hospital
- 1% of the patients died within 24 hours of arresting
- Mean time to DSD was 31.4 minutes +/- 12
- On average DSD was performed a total of 2 times
Strengths:
- Very inclusive literature review of all published cases between 1946 and 2018
- Used a wide variety of databases: Google Scholar, Cochrane Library, Medline, PubMed
- Had 2 levels of study screening
- Inclusion and exclusion criteria as described above
- Further inclusion required unprovoked cardiac arrest or occurrence of V-Fib and reports on patients rather than summary statistics
- Commented on the findings of other published papers that did not meet their inclusion criteria
Limitations:
- Studies are not prospective or randomized. Performing a RCT would be difficult as RVF is a rare phenomenon
- Selection bias with case reports limits us in knowing how many times DSD was performed without any success in the clinical setting.
- Did not come to a consensus in the literature on the definition of refractory VF
- Simultaneous vs Sequential = This could have been the stepping stone to a study that helped identify which was more effective.
- No defined optimal pulse interval in any of the published papers or cases
- Use of CPC score vs Rankin Score
- Authors did not include data from a retrospective cohort analysis on the use of pre-hospital dual defibrillation which showed no neurologically intact survival
Discussion:
- Patients discharged with a CPC score of 2 or less were not only younger but also had a shorter time-to-DSD interval and resuscitation time
- RVF depends on multiple variables:
- Amount of time in VF
- Body habitus (despite animal models showing inverse relationship with defibrillation)
- Total defibrillator energy used
- Chronic lung disease
- Antiarrhythmic agents
- Energy waveforms
- Higher energy and myocardial stunning are concerns with higher amounts of energy however several studieshave confirmed their safety in humans.14-17
- Pad Placement: First set of pads is placed in the traditional anterolateral position with the second sets adjacent to them or in the anteroposterior position
- **Authors do not state this but it is IMPORTANT that the pads are NOT touching otherwise you risk damaging BOTH defibrillators***
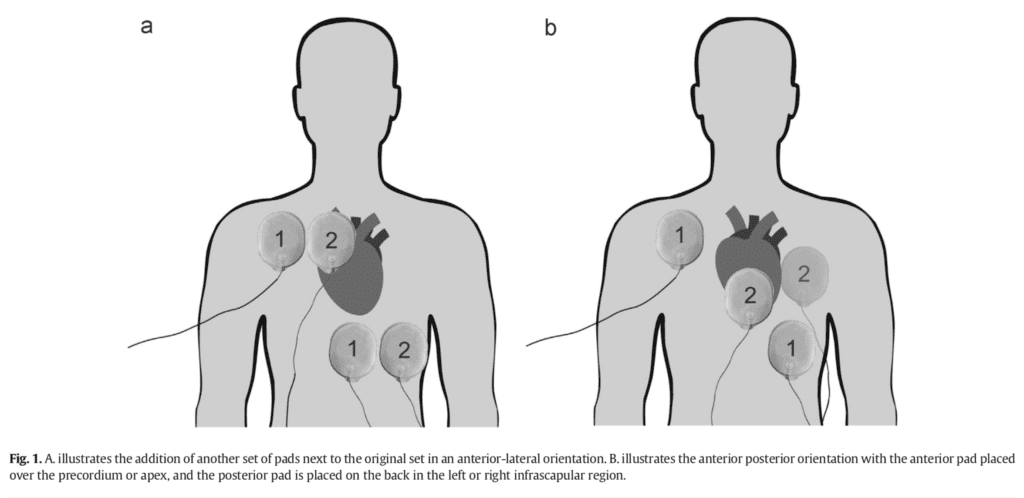
Image from Pourmand A et al. AJEM 2018 PMID: 29880409
- Addressed that some studies suggest the use of an optimal interval (0.5 – 4 s) to override the relative refractory period of cardiac muscle.
- The study that the authors omitted was a retrospective cohort analysis of 3470 cases of OHCA by Ross et al.
- 302 cases had recurrent or refractory VF identified, 23 had incomplete data.
- Of the remaining 279, 50 were treated with DD and 229 received standard single defibrillation
- The authors of this study report no statistically significant difference in neurologically intact survival between the two groups
- It is important to note some of the limitations of this study
- Selection bias given that it is an observational study and decision to perform DD was left to the lead paramedic
- Confounding variable bias given lack of a structured protocol for a new and unknown intervention, thus contributing to a questionable or flawed method of performing the overall study.
- In smaller ambulance companies a second defibrillator was not always immediately available thus preventing the intervention from being performed when it may have been indicated.
- Authors combined both refractory VF and recurrent VF together which may have falsely increased their total numbers as DD is indicated for only refractory VF at this time.
- Incomplete data: The authors were unable to obtain how many defibrillation attempts were performed prior to DD, number of times DD was performed, timing of DD shock and the practice or technique that DD was performed.18
- Further studies are required to generate a prediction model of double defibrillation success.
Author’s Conclusions:
- Previous published data shows promising results with the use of double sequential defibrillation. Randomized control trials are required to institute recommendations on its use and implementations in ACLS algorithms
Our Conclusion:
- Although heterogenous, dual defibrillation appears to be a useful low resource intervention for the termination of refractory ventricular fibrillation.
- Dual defibrillation serves as another tool in your resuscitation armamentarium and should be considered with other advanced life-saving therapies such as ECMO and cardiac catherization.
- Future research is required to distinguish double sequential from double simultaneous defibrillation as well as the efficacy of each
- There may be some potential in utilizing double defibrillation sooner when a patient presents in refractory ventricular fibrillation
- One last point to mention is publication bias. There are likely many failed attempts at DSD and when it does not lead to ROSC or termination of RVF, one is less likely to write up a case report or perform a case series. This in turn limits our understanding of whether or not it works as we are only seeing the successful cases.
Clinical Bottom Line:
- Consider the use of a second defibrillator for cardiac arrest patients in refractory ventricular fibrillation.
Guest Post By:
 Mark Ramzy DO, EMT-P
Mark Ramzy DO, EMT-P
Drexel University
Philadelphia, PA
Twitter: @MRamzyDO
References:
- Go AS, et al. On behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014; PMID: 24446411
- Eifling M, et al. The evaluation and management of electrical storm. Tex Heart Inst J 2011; PMID: 21494516
- Sakai T, et al. Incidence and outcomes of out-of hospital cardiac arrest with shock-resistant ventricular fibrillation: data from a large population-based cohort. Resuscitation. 2010; PMID: 20653086
- Sarkozy A et al, Strategies for reversing shock resistant ventricular fibrillation. Curr Opin Crit Care. 2003; PMID: 12771668
- Dorian P, et al, Amiodarone as compared with lidocaine for shock resistant ventricular fibrillation. N Engl J Med. 2002; PMID: 11907287
- Windecker S, et al. Percutaneous left ventricular assist devices for treatment of patients with cardiogenic shock. Curr Opin Crit Care 2007; PMID: 17762230
- Herlitz J, et al, Rhythm changes during resuscitation from ventricular fibrillation in relation to delay until defibrillation, number of shocks delivered and survival. Resuscitation 1997; PMID: 9051819
- Sena R, et al. Refractory Ventricular Fibrillation Successfully Cardioverted With Dual Sequential Defibrillation. J Emerg Med. 2016; PMID: 27369859
- Bell C, et al. Make it two: A case report of dual sequential external defibrillation. CJEM. 2017; PMID: 28587703
- Boehm K. et al. First Report of Survival in Refractory Ventricular Fibrillation After Dual-Axis Defibrillation and Esmolol Administration. Western Journal of Emergency Medicine. 2016; PMID: 27833686
- El Tawil C, et al. Double sequential defibrillation for refractory ventricular fibrillation. Am J Emerg Med. 2017; PMID: 28978402
- Leacock B, Double Simultaneous Defibrillators for Refractory Ventricular Fibrillation. J Emerg Med. 2014; PMID: 24462025
- Johnson E, et al. Effect of pulse separation between two sequential biphasic shocks given over different lead configurations on ventricular defibrillation efficacy. Circulation 1992; PMID: 1591840
- Chen B, et al. Retrospective evaluation of current-based impedance compensation defibrillation in out-of-hospital cardiac arrest. Resuscitation. 2013; PMID: 23000364
- Zhang Y, et al. Body weight is a predictor of biphasic shock success for low energy transthoracic defibrillation. Resuscitation. 2002; PMID: 12204462
- Stiell I, et al. BIPHASIC Trial: A Randomized Comparison of Fixed Lower Versus Escalating Higher Energy Levels for Defibrillation in Out-of-Hospital Cardiac Arrest. Circulation. 2007; PMID: 17353443
- White RD, et al. Body weight does not affect defibrillation, resuscitation, or survival in patients with out-of-hospital cardiac arrest treated with a nonescalating biphasic waveform defibrillator. Crit Care Med 2004; PMID: 15508666
- Ross EM, et al. Dual defibrillation in out-of-hospital cardiac arrest: a retrospective cohort analysis. Resuscitation 2016; PMID: 27344928
For More Thoughts on This Topic Checkout:
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)