The 2017 edition of the Social Media And Critical Care (SMACC) conference was held in Berlin, Germany this year (#dasSMACC). Over 2000 emergency physicians, intensivists, anesthetists, EMS providers, and nurses piled into the Tempodrom for three days of inspiring lectures and an all-around good time. This conference is truly a leader in innovation and continues to push the boundaries of medical education and entertainment. Here are some of the lessons learned and take home messages from the first day of the conference.
The 2017 edition of the Social Media And Critical Care (SMACC) conference was held in Berlin, Germany this year (#dasSMACC). Over 2000 emergency physicians, intensivists, anesthetists, EMS providers, and nurses piled into the Tempodrom for three days of inspiring lectures and an all-around good time. This conference is truly a leader in innovation and continues to push the boundaries of medical education and entertainment. Here are some of the lessons learned and take home messages from the first day of the conference.
dasSMACC – Day #1
Tempodrom in Berlin, Germany

Day #1: June 27th, 2017
Brian Burns started the conference off by discussing the future of prehospital trauma care:
- Trauma kills 5 million/year and predicted to be 8 million/year by 2020
- Trauma is the number one killer of people <40 years of age
- 1/4 of trauma deaths in the world are due to motor vehicle accidents
- 90% of prehospital trauma deaths are due to bleeding
- Future of prehospital trauma:
- Early warning systems – Automated response technology in vehicles
- Real-time patient data from biosensor watches and kinematic data from vehicle
- Point of care TEG – Blood products could be dispatched with drone technology to trauma scene to initiate prehospital massive transfusion protocol
- Remote site POCUS interpretation
- Avoiding communication blackout with trauma center receiving live data as medics extricate via telemedicine
Jess Mason relayed the story of one of her patients, a former EMT, that succumbed to Sickle Cell Disease:
- Medical education mixed with the human condition = narrative medicine (i.e. The patient becomes the teacher)
- If you remember the story, you will remember the medicine
- Sickle cell disease is a terminal condition, not unlike metastatic cancer
- Life expectancy for these patients is only into the mid 40s
- Give early IV analgesia
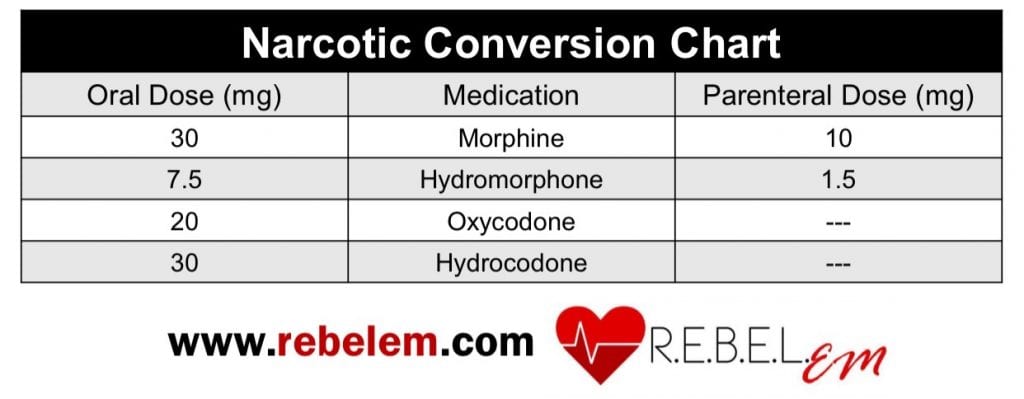
- Know how to convert different types of narcotics so you don’t under or overdose your patient
Sara Gray gave a talk giving us permission to be kind to ourselves when things don’t go as expected:
- The voices in your head are critical and judgmental
- Our culture of silence is killing us. Not talking about our fears and anxieties can lead to anxiety, depression, burnout, and ultimately suicide
- Self-compassion has positive physiologic effects
- Self-compassion is a resuscitation skill that need s to be practiced
- Have a failure friend = a go to person you can talk to when you make a mistake
- Your emotional/psychological state can influence your performance during critical events
- Calling for help is not a sign of weakness. Knowing when to ask for help is an important skill
- Great resources for this are located at www.selfcompassion.org
- Take Home Message: Listen to your inner dialogue, practice better self talk, and have empathy toward others
Alex Psirides spoke on “Doing Everything” at the end of life:
- Talking about dying does not lead to death, just as talking about sex does not lead to pregnancy
- Beware of optimism bias. We often overestimate the benefits of what we can do and deliver, but underestimate the potential harms
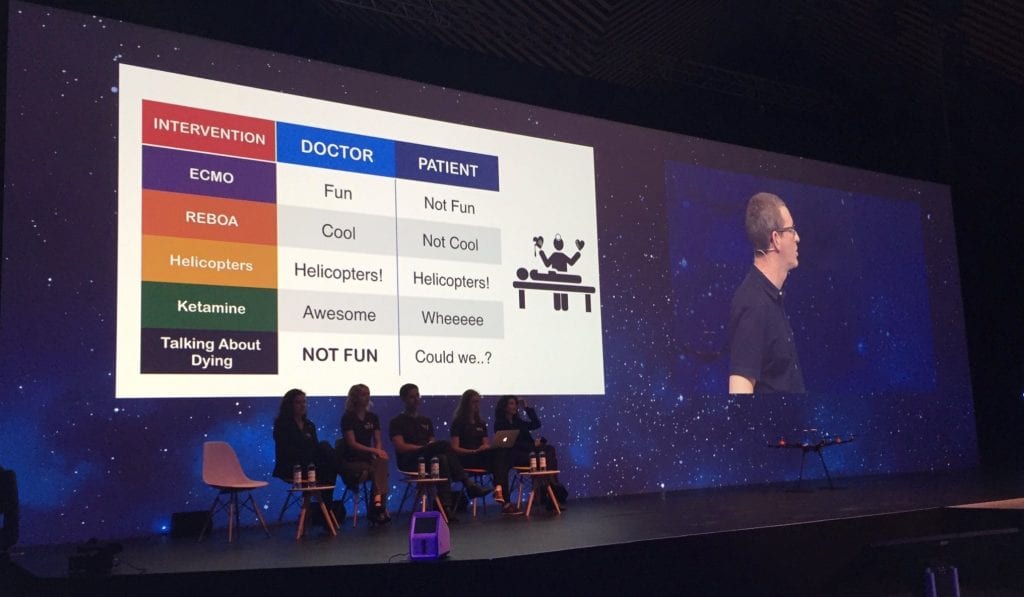
- Give your patients the death you would want
- Remember to provide maximal care to your patients, whether you resuscitate or you palliate
Rinaldo Bellomo dropped some fantastic points on general patient care and faulty thought processes:
- The biggest threat to understanding is the illusion of knowledge
- Doctors suffer from physiologic seduction. We always try to make everything normal, but this may actually cause more harm to patients
- Human beings are perfectible, but not perfect
- “It ain’t what you don’t know that gets you into trouble. It’s what you know for sure that just ain’t so.” Mark Twain
- In reference to the publication of bad research: The amount of energy necessary to refute bullshit is an order of magnitude bigger than to produce it
- We make the measurable important, but we don’t make the important measurable
David Carr gave a brilliant talk in an effort to make endocarditis “sexy”:
- Valve replacement (mechanical or animal) patient’s risk of endocarditis increases 1% per year.
- Other at risk populations for endocarditis: IVDU (obviously), cancer (especially adenocarcinoma), and lupus
- Fever + 1 should lead you to look for endocarditis
- + Stroke
- + Back pain
- + Heart failure
- + 1° AV block (high risk for perivalvular abscess)
- Up to 95% of endocarditis patients have fever
- Up to 90% of endocarditis patients have a murmur
- Coagulase negative Staph aureus is the 2nd leading cause of endocarditis (25%) in valve replacement patients
- Get 3 culture sets, from 3 different locations, one hour apart
- Empiric treatment for endocarditis = Vancomycin + Rocephin
Paul Young then gave a very though provoking talk on the current state of research:
- P values suck…instead we should be thinking about probability and use a Bayesian model in interpreting research
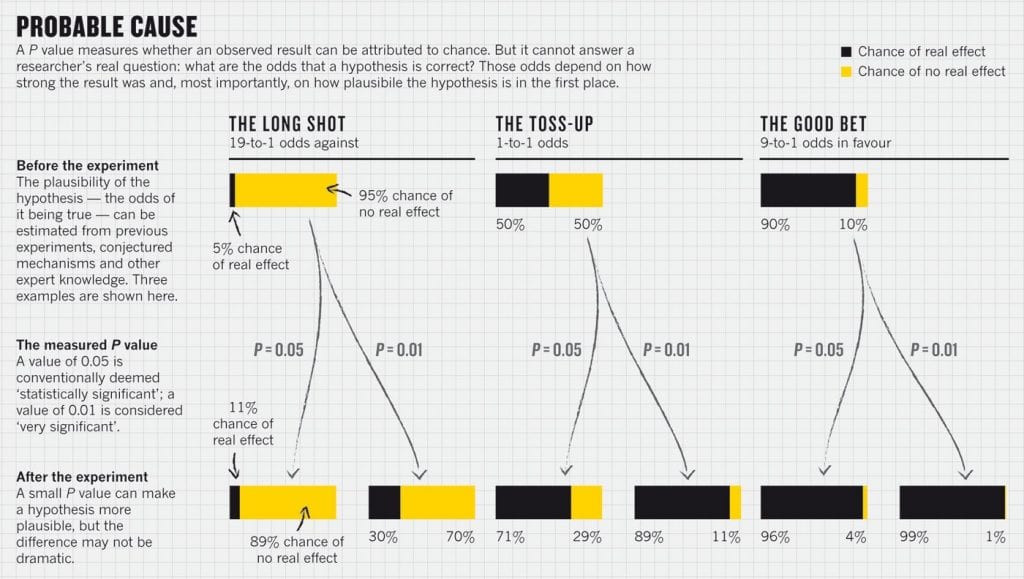
Image from HERE
- The fragility index is a useful tool to help assess usefulness of randomized trials
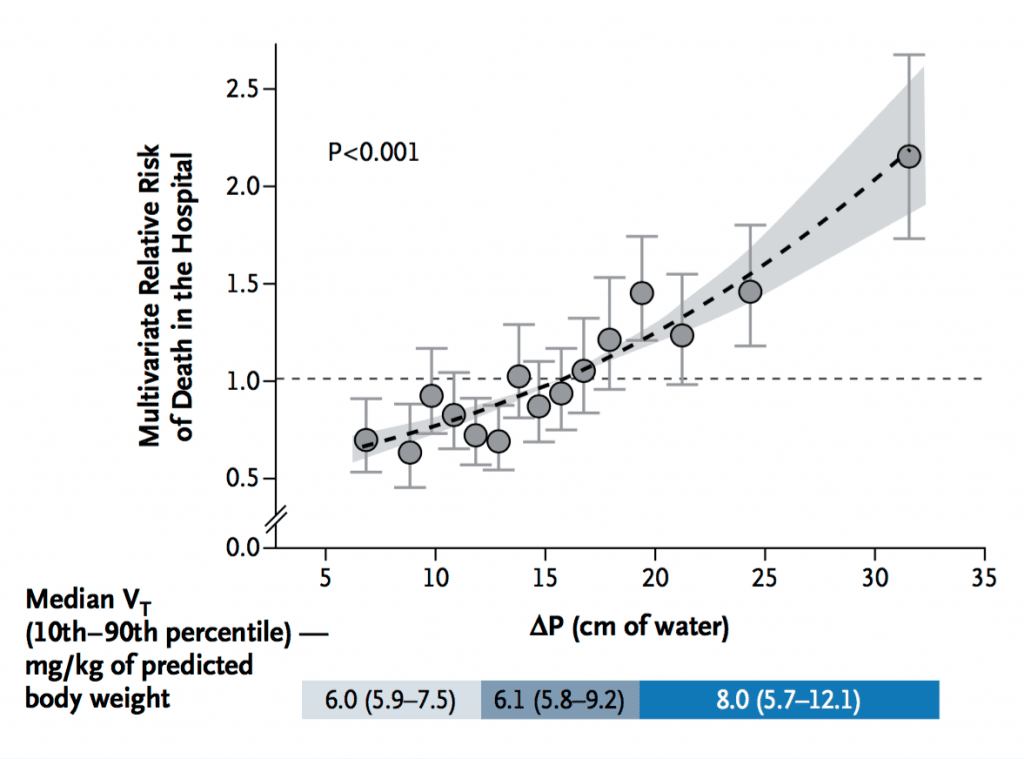
Marcelo Amato was the lead author on the paper introducing driving pressure in ventilated patients with ARDS:
- Size of tidal volume is not important, it is the pressure generated that leads to lung injury
- Targeting tidal volume is a “one-size-fits-all” approach. It is not right for every patient
- Driving pressure = Plateau pressure – PEEP
- Decrease in driving pressure is directly proportional to increase in survival in ARDS
- Link to New England Journal of Medicine 2015 Publication HERE
Michelle Johnston sent a backdoor shot to thrombolytics for stroke by saying we really don’t know how it works and called for more specific treatments for clot removal:
- The treatment of choice for bleeding after giving tPa is cryoprecipitate
- Other choices include platelets, fresh frozen plasma (not enough factors), and prothrombin complex concentrates
For More on This Topic Checkout:
- Simon Carley at St. Emlyn’s: #dasSMACC Day 1 With St. Emlyn’s
- Lauren Westafer & Jeremy Faust at FOAMCast: #dasSMACC – Endocarditis, Statistics, & Sickle Cell
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)