 Acute and recurrent pericarditis are frequently diagnosed in the emergency department. Traditionally, treatment has consisted of anti-inflammatory medications (eg. ASA or NSAIDs) or corticosteroids. Colchicine is an underutilized therapy for pericarditis and provides significant benefit when combined with NSAIDs/ASA. Addition of colchicine to standard therapy results in earlier reduction in pericarditis symptoms, greater remission at 1 week, and reduces the rate of recurrent pericarditis. Let’s review the literature for colchicine for treatment of pericarditis.
Acute and recurrent pericarditis are frequently diagnosed in the emergency department. Traditionally, treatment has consisted of anti-inflammatory medications (eg. ASA or NSAIDs) or corticosteroids. Colchicine is an underutilized therapy for pericarditis and provides significant benefit when combined with NSAIDs/ASA. Addition of colchicine to standard therapy results in earlier reduction in pericarditis symptoms, greater remission at 1 week, and reduces the rate of recurrent pericarditis. Let’s review the literature for colchicine for treatment of pericarditis.
What is Colchicine?

Colchicine is a plant derived compound that inhibits microtubule formation, thus effectively inhibiting mitosis. It also acts to inhibit neutrophil activity and has an anti-inflammatory effect. Known uses include treatment of gout and familial Mediterranean fever (FMF).
Studies of Colchicine for acute (1st Episode) pericarditis
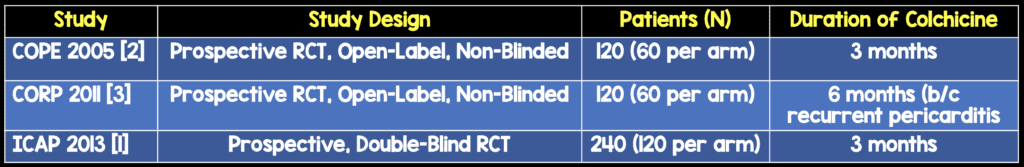
The COPE (Imazio, 2005) and ICAP (Imazio, 2013) trials both studied the effects of adding colchicine to standard anti-inflammatory therapy for treatment of pericarditis.
CORP (Imazio, 2011) studied use of colchicine in the first episode of recurrent pericarditis.
What were the outcomes? (All reported as colchicine vs. placebo)
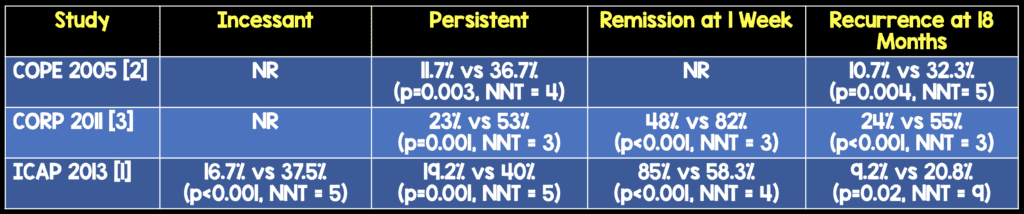
*Median number of recurrences at 20 months follow-up in CORP.

What dose of colchicine do you give?
In all trials, the dose was 1-2 mg on the first day, followed by 0.5 mg BID for patients > 70 kg or 0.5 mg once daily for patients < 70 kg.
What about side effects, especially diarrhea?
If patients on colchicine cannot tolerate due to GI upset, they should reduce the dose to once daily if > 70 kg, or stop it if < 70 kg.
What about using steroids for pericarditis?
Both COPE and ICAP performed multivariate analysis to determine risk factors for recurrence of pericarditis. In both trials, prednisone use was an independent risk factor for subsequent development of recurrences: COPE (OR 4.30, 95% CI 1.21-15.25; p=0.024) ICAP (OR 4.17; 95% CI, 1.28-13.53; p=0.02) In patients who cannot tolerate NSAIDs, have high GI bleed risk or have other contraindications for NSAID/colchicine use, steroids should be used. There should be solid clinical reasoning each time you prescribe steroids for pericarditis, and consideration for expert consultation should be given in these cases.
Who should get Colchicine for pericarditis?
Pretty much everyone in whom it is not contraindicated (see below).
What are the contraindications to Colchicine use?
Although it works well, many groups are excluded from studies of colchicine because of its side effects. In general, neoplastic pericarditis, bacterial pericarditis, significant liver or kidney disease, blood dyscrasias, and pregnancy are the big categories. Here is the list of exclusion criteria for ICAP:
Tuberculous pericarditis
Neoplastic pericarditis
Purulent pericarditis
Severe liver disease or aminotransferase levels ≥1.5x ULN
Serum creatinine >2.5 mg/dL (>221 umol/L)
Skeletal myopathy or CK >ULN
Blood dyscrasia IBD
Hypersensitivity to colchicine or other contraindication to its use
Life expectancy ≤18 months
Pregnancy or lactation
Women of childbearing potential not using contraception
Evidence of myopericarditis as evidenced by elevation in serum troponin
What other medication should everyone be prescribed?
A PPI (proton pump inhibitor). The combination of high dose NSAIDs/ASA + Colchicine or steroids is pretty much a recipe for gastritis/peptic ulcer disease, so PPIs were prescribed in all studies. Duration of PPI therapy was not disclosed, but I would prescribe it at minimum for the duration of NSAID use. Giving a PPI for the entire duration of colchicine use would also be reasonable.

Clinical Bottom Line
Unless there are contraindications to its use, colchicine should be prescribed in all cases of uncomplicated pericarditis, along with standard therapy of ASA/NSAID and a PPI. Glucocorticoids should be prescribed with caution, as they are an independent risk factor for pericarditis recurrence.
Bibliography:
- Imazio M, et al. “A Randomized Trial of Colchicine for Acute Pericarditis”. The New England Journal of Medicine. 2013. PMID:23992557
- Imazio M, et al. “Colchicine in Addition to Conventional Therapy for Acute Pericarditis : Results of the COlchicine for acute PEricarditis (COPE) Trial”Circulation. 2005. PMID:16186437
- Imazio M, et al. “Colchicine for Recurrent Pericarditis (CORP)” Ann Intern Med. 2011. PMID: 21873705



