REBEL Cast Ep99: The INTUBE Study – Adverse Peri-Intubation Events in the Critically Ill
Paper: Russotto V et al. Intubation Practices and adverse Peri-Intubation Events in Critically Ill Patients From 29 Countries. JAMA 2021. PMID: 33755076 [Access on Read by QxMD]
Clinical Question: Among critically ill patient undergoing tracheal intubation worldwide, how common are major adverse events during the peri-intubation period?
What They Did:
- International Observational Study to Understand the Impact and Best Practices of Airway Management in Critically Ill Patients (INTUBE)
- International, multicenter, prospective cohort study of consecutive critically ill patients undergoing tracheal intubation in the ICU, ED, and wards
- Took place from October 2018 go July 2019
- 197 sites from 29 countries across 5 continents
Outcomes:
- Primary: Incidence of major adverse peri-intubation events
- Defined as at least one of the following events occurring within 30 minutes from start of intubation procedure
- CV instability (SBP <65mmHg at least once, <90mmHg for >30min, new or increased need for vasopressors or fluid bolus >15mL/kg)
- Severe hypoxemia (Peripheral O2 sat <80%)
- Cardiac arrest
- Important Secondary Outcomes:
- ICU mortality
- 28d mortality (post-hoc analysis)
- Incidence of
- Cardiac arrhythmias
- Difficult intubation
- Cannot-intubate or cannot-oxygenate scenario
- Emergency front of neck airway
- Pulmonary aspiration of gastric contents
- Esophageal intubation
- Pneumothorax or pneumomediastinum
- Airway injury
- Dental injury
- Defined as at least one of the following events occurring within 30 minutes from start of intubation procedure
Inclusion:
- Critically ill adult patients (≥18 years of age)
- Life-threatening impairment of cardiovascular, respiratory or neurological systems
- Requiring in-hospital intubation in the ED, ICU, and wards
Exclusion:
- Out of hospital intubation following cardiac arrest
- Intubated for purposes of general anesthesia
- Patients that had an outcome parameter prior to intubation (i.e. hypotension at time of intubation)
- Patients meeting a criterion before the stat of laryngoscopy (i.e. SpO2 <80% at the end of preoxygenation)
Results:
- 3659 patients screened
- 2964 patients included in analysis
- Median age = 63 years
- 67.2% of intubations occurred in the ICU
- 21.0% of intubations occurred in the ED
- Resident physicians intubated 51.9% of patients
- Anesthesiologists intubated 54.0% of patients
- Main reasons for intubation:
- Respiratory failure: 52.3%
- Neurological impairment: 30.5%
- Cardiovascular instability: 9.4%
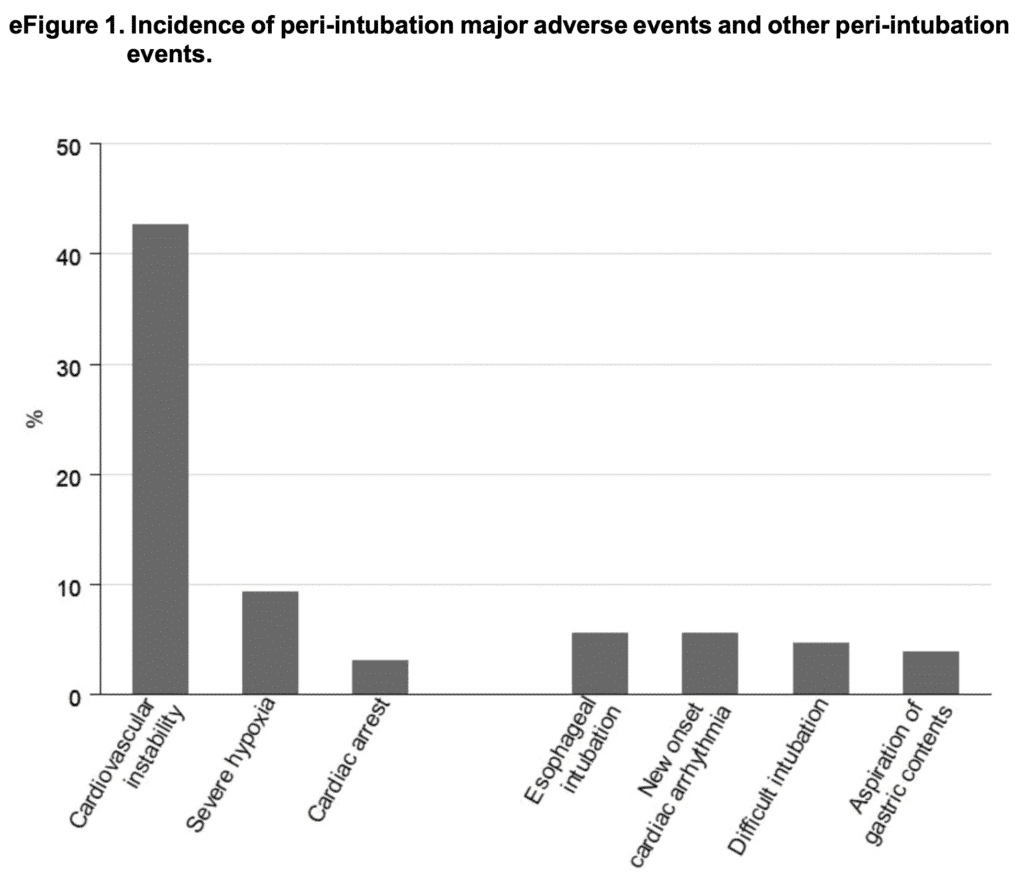
- 45.2% of patients experienced at least 1 major adverse peri-intubation event
- Predominant event was CV instability: 42.6%
- New need or increase of vasopressors: 89.9%
- SBP <90mmHg for >30min: 24.6%
- Severe hypoxemia: 9.3%
- Cardiac arrest: 3.1%
- With ROSC: 52.7%
- Without ROSC: 47.3%
- Causes of Cardiac Arrest:
- Hypovolemia or hemodynamic instability: 36.9%
- Hypoxia: 25.0%
- Thrombosis (coronary or pulmonary): 20.6%
- Other Adverse Events:
- Esophageal intubation: 5.6%
- New onset cardiac arrhythmia: 5.6%
- Difficult intubation: 4.7%
- Aspiration of gastric contents: 3.9%
- Predominant event was CV instability: 42.6%
- Overall ICU mortality: 32.8%
- Experienced a major adverse peri-intubation event: 40.7% died
- Did NOT experience a major adverse peri-intubation event: 26.3% died
- Absolute risk difference: 14.4%; 95% CI 10.9 to 17.9%; p<0.001
- Tracheal Intubation Practices:
- Preoxygenation:
- BVM: 62.4%
- Standard facemask: 13.2%
- NIV: 11.6%
- HFNC: 5.4%
- Apneic oxygenation: 10.4%
- RSI: 62.2%
- Induction Agent:
- Propofol: 41.5%
- Midazolam: 36.4%
- Etomidate: 17.8%
- Ketamine: 14.2%
- In patients with concurrent hemodynamic instability the use of propofol was associated with CV instability in 63.7% vs 49.5% in patients receiving etomidate
- Paralytic:
- Rocuronium: 41.8%
- Succinylcholine: 21.8%
- Laryngoscopy:
- DL: 81.5%
- VL: 17.1%
- Adjuncts:
- Stylet: 77.4%
- Bougie: 21.8%
- 1st Method Used to Confirm Intubation:
- Auscultation: 57.9%
- Waveform capnography: 25.6%
- Capnography was not used for 68.9% of patients who had undergone esophageal intubation
- Successful Tracheal Intubation:
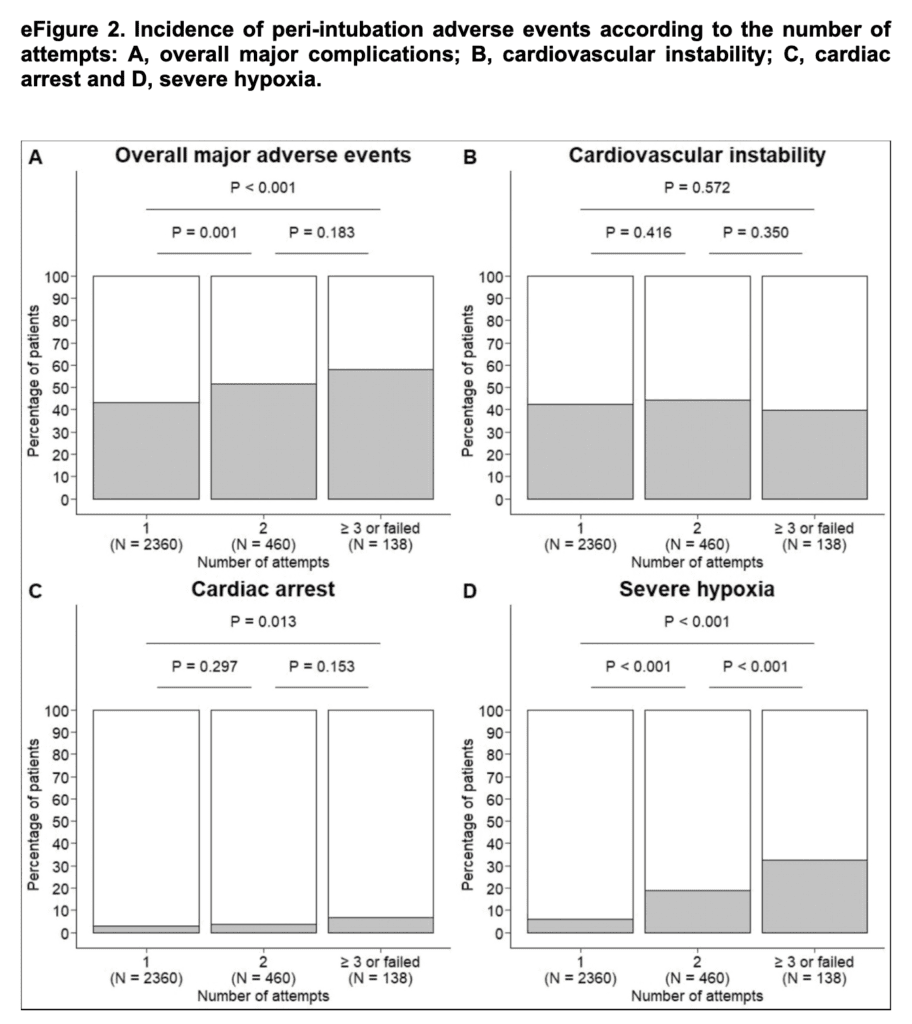
- 1st pass: 79.8%
- 2nd pass: 15.6%
- FONA: 0.13%
- Rate of major adverse events was significantly lower with 1st pass success than it was for patients requiring 2 attempts
- Preoxygenation:
Strengths:
- Large, heterogenous cohort from variable practice settings
- Asks a clinically important question
Limitations:
- Self-reporting of adverse events may have led to an overestimation of some conditions or underestimation of procedure-related adverse events (i.e. cases left out where there were bad outcomes)
- Describe issues, but don’t give granular details of what was done prior to limit effects of intubation on hemodynamic parameters (i.e. what resuscitation), what doses of agents given (dose more important than agent)
- Granular detail on ED vs ICU vs ward intubations would be good to know (i.e. did we see different problems in different locations)
- Unclear if this is truly a consecutive or convenience sample which could lead to selection bias
- Results could be biased by unmeasured confounders
- Unclear long-term consequences of adverse peri-intubation events (i.e. hypoxic brain injury) – Not patient centered (except for cardiac arrest)
Discussion:
- Cardiovascular instability was the most frequent adverse event following intubation
- We have spent lots of time figuring out how to preoxygenate optimally. We rarely start RSI with an oxygen saturation of 80 to 85% if we can avoid it but start intubations all the time with a SBP of ≈90mmHg. This may reflect practice pattern in terms of resuscitation and how we’ve been trained to resuscitate prior to intubation
- Interventions aiming to achieve better cardiovascular stability before tracheal intubation will be key
- Fluid replacement where appropriate
- Peripheral vasopressors (drip or push-dose)
- Dosing sedatives low and paralytics high
- Consider awake intubation
- Optimizing 1st pass success is also important in reducing adverse events
- Use of video laryngoscopy
- Authors don’t discuss what types of devices used as hyperangulated and standard geometry blades are very different
- Bougie 1st intubation
- Optimal patient placement (head of bed elevation)
- Use of video laryngoscopy
- Recognizing esophageal intubation
- Waveform capnography should be standard practice
- 9% of esophageal intubations did not have waveform capnography in place
- It is important to remember the authors excluded patients who were already hemodynamically unstable. If patients are hypotensive, things will worsen with intubation, so be ready with post-intubation support or maybe we should be working to push VS higher prior to intubation. It is all about anticipation. The predominance of hemodynamic issues shows that we need to spend more time training on this part of intubation. Areas of future research should focus on the meds we use and the doses we use as well.
Author Conclusion: “In this observational study of intubation practices in critically ill patients from a convenience sample of 197 sites across 29 countries, major adverse peri-intubation events – in particular cardiovascular instability – were observed frequently.”
Clinical Take Home Point: In critically ill patients from 197 sites across 29 countries, major adverse peri-intubation events occurred frequently. In particular cardiovascular instability was very common. RESUSCITATE BEFORE YOU INTUBATE. Strategies to consider in reducing cardiovascular instability prior to intubation include: IV fluids where appropriate, peripheral pressors (push-dose and/or drips), dosing sedatives low/paralytics high, and consideration for awake intubation.
References:
- Russotto V et al. Intubation Practices and adverse Peri-Intubation Events in Critically Ill Patients From 29 Countries. JAMA 2021. PMID: 33755076 [Access on Read by QxMD]
For More Thoughts on This Topic Checkout:
- REBEL EM: Critical Care Updates – Resuscitation Sequence Intubation – Hypotension Kills (Part 1 of 3)
- REBEL EM: Dosing Sedatives Low and Paralytics High in Shock Patients Requiring RSI
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)



