Paper: Benary D et al. Ondansetron Prescription Is Associated With Reduced Return Visits to the Pediatric Emergency Department for Children With Gastroenteritis. Ann Emerg Med 2020. PMID 32471647
Clinical Question: Does a discharge outpatient prescription for ondansetron impact the rate of return visits for children discharged from the emergency department for vomiting or acute gastroenteritis at 72 hours?
What They Did:
- Retrospective cohort study of pediatric patients presenting to a large, urban, tertiary pediatric ED and 11 affiliated urgent care sites
- 5-year study period (April 2012 – December 2017)
- Multivariate logistic regression analysis used to measure association between an ondansetron prescription and odds of 72-hour return visits
Outcomes:
- Primary
- Rate of return visits to the ED or urgent care (UC) within 72 hours of index visit for patients with vomiting or gastroenteritis
- Secondary
- Rate of return visits to the ED or UC within 72 hours of index visit in subgroup of patients with a diagnosis of gastroenteritis
- Rates of select alternative diagnoses on return visits within 7 days, including:
- Appendicitis
- Intussusception
- Intracranial mass
- Meningitis
- Diabetic ketoacidosis
Inclusion:
- Age between 6 months and 18 years of age
- Index visit to ED or UC – no other ED or UC visits in the prior 30 days
- Discharged home with one or more of the following diagnoses:
- Gastroenteritis
- Vomiting and diarrhea
- Vomiting alone
- Gastritis
- Discharged home with the diagnosis dehydration only if there was an associated diagnosis of vomiting
Exclusion:
- Diagnosis of diarrhea without vomiting
- Age <6 months
- Patients admitted to the hospital or missing disposition
- Patient deemed to have a relevant pre-existing medical condition
Results:
- 82,139 patients in study
- Median age of 4 years
- 58.9% of visits were to the ED
- IV fluid bolus given in 7.9% of patients
- Ondansetron administered during the visit to 55.1% of patients
- 11,004 patients (13.4%) were given discharge prescription for ondansetron
- 3,851 patients (4.7%) had a return visit within 72 hours of index visit
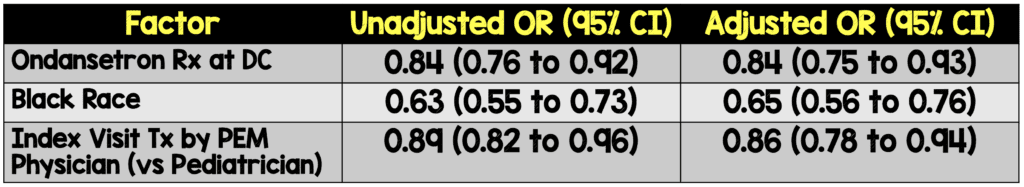
Factors associated with reduced odds of 72-hour return visit (adjusted OR)
- Ondansetron prescription at discharge
- Black race
- Index visit treatment by PEM physician (vs pediatrician)
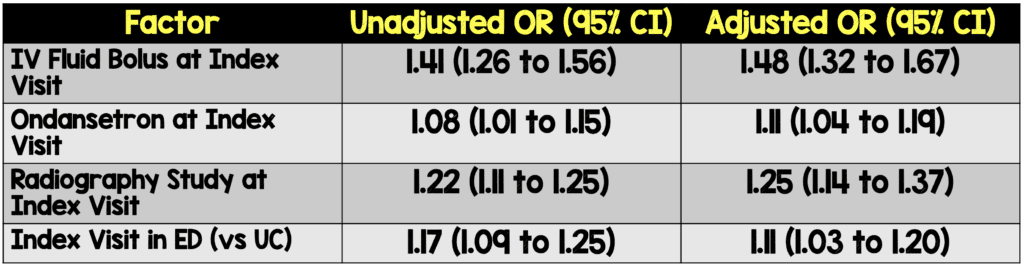
Factors associated with increased odds of 72-hour return visit
- Younger age (less than 3 years of age was more likely to return within 72 hours)
- IV fluid bolus at index visit
- Ondansetron given at index visit
- Radiography study performed at index visit
- Index visit in ED (vs UC)
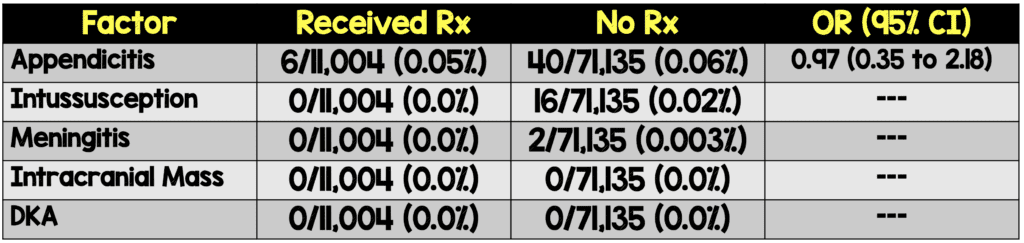
Return visit diagnoses:
Strengths:
- Large study population
- Asks clinically significant question
- Chart review was performed by the primary author on 100 randomly selected patient charts to ensure accuracy and consistency of the data.
- Performed subgroup analysis and adjusted analysis for confounding factors to confirm results.
- Included diagnoses other than gastroenteritis that cause vomiting which make results more applicable to daily practice. Also did a subgroup analysis of gastroenteritis vs other causes of vomiting which found similar results to the total population.
- Confounding variables were selected a priori from previous clinical experience to account for severity of disease between groups.
Limitations:
- Retrospective cohort study rather than randomized trial.
- There were statistically significant differences between most baseline characteristics between the two groups.
- Patients receiving ondansetron prescription were older than those who did not.
- Patients were less likely to receive ondansetron prescription if they were black, non-Hispanic or insured with Medicaid.
- 86.3% of study subjects were white, potentially limiting applicability to broader patient population.
- It is unclear how many doses of ondansetron were prescribed with prescriptions, whether the prescriptions were filled, and how much of the prescription was used.
- It is unclear what the education level of parents or access for follow-up with a pediatrician was in this population.
- Frequencies of alternative diagnoses were too low to draw any meaningful conclusions
- There may have been other confounding factors that were not measured and controlled for in this trial (i.e. patient care at discretion of treating physician).
- Follow up information was only within the hospital system. If a return visit happened outside the system, it would have been missed.
Discussion:
- Medicaid insured, black, and non-Hispanic patients were less likely to receive an ondansetron prescription
- Despite the finding of decreased odds of return for patients given ondansetron prescription (NNT = 138), the baseline return rate of 4.7% was low making the differences between groups small
- In the appropriate patients an ondansetron prescription can help with oral rehydration therapy at home while also decreasing return rates. Additionally, in this study, there was no increase in the risk of patients’ returning with an alternative diagnosis
- Included patients treated in urgent care settings. This may have been a less sick population compared to an ED setting. This could affect return visits and alternative diagnoses made (i.e. under reported in this trial)
- Due to the large size of the trial, some statistically significant differences may not be clinically meaningful
- One concern about prescribing ondansetron for home use is delayed presentations of appendicitis (i.e. perforated appendicitis). In this trial 13 cases of perforated appendicitis were found. Only 3 of these had prescriptions for home ondansetron. Of these 2 patients returned within 24hrs of the index visit and the third patient returned after 4 days
- All remaining alternative diagnoses were found in patients not given prescriptions for home ondansetron
- Salim: In my clinical practice, if I am sending a pediatric patient home with SL ondansetron, I typically do not give more than 48hrs worth. Most benign etiologies should improve in that time window in my experience. Therefore, patients are more likely to return when the rx runs out without significant delays in care
Author Conclusion: “An ondansetron prescription is associated with reduced 72-hour ED return visit rates for children with vomiting or acute gastroenteritis and is not associated with masking alternate diagnoses.”
Clinical Take Home Point: Provided a patient can receive good home monitoring and reliable follow up if needed, a discharge ondansetron prescription seems like a reasonable option for pediatric patients presenting to the emergency department with vomiting. The discharge prescription reduces 72-hour return visits which can contribute to ED crowding and cost without the risk of masking an alternate diagnosis.
References:
- Benary D, Lozano JM, Higley R, Lowe D. Ondansetron Prescription Is Associated With Reduced Return Visits to the Pediatric Emergency Department for Children With Gastroenteritis [published online ahead of print, 2020 May 26]. Ann Emerg Med. 2020. PMID 32471647
- Gray JM, Maewal JD, Lunos SA, Furnival RA, Hendrickson MA. Ondansetron Prescription for Home Use in a Pediatric Emergency Department. Pediatr Emerg Care 2020. PMID 29135900
- McLaren SH, Yim RB, Fleegler EW. Impact of Ondansetron Prescription on Return Emergency Department Visits Among Children with Acute Gastroenteritis [published online ahead of print, 2019 Sep 12]. Pediatr Emerg Care 2019. PMID 31524821
For More Thoughts on this Topic:
- Journal Feed: Maybe Ondansetron Rx Does Reduce Bouncebacks in Kids
- PEMBlog: Why we do what we do: Ondansetron for acute gastroenteritis associated vomiting
- The NNT: Ondansetron (Zofran) for Pediatric Gastroenteritis
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)



