To go back to the main post, click on the image below…
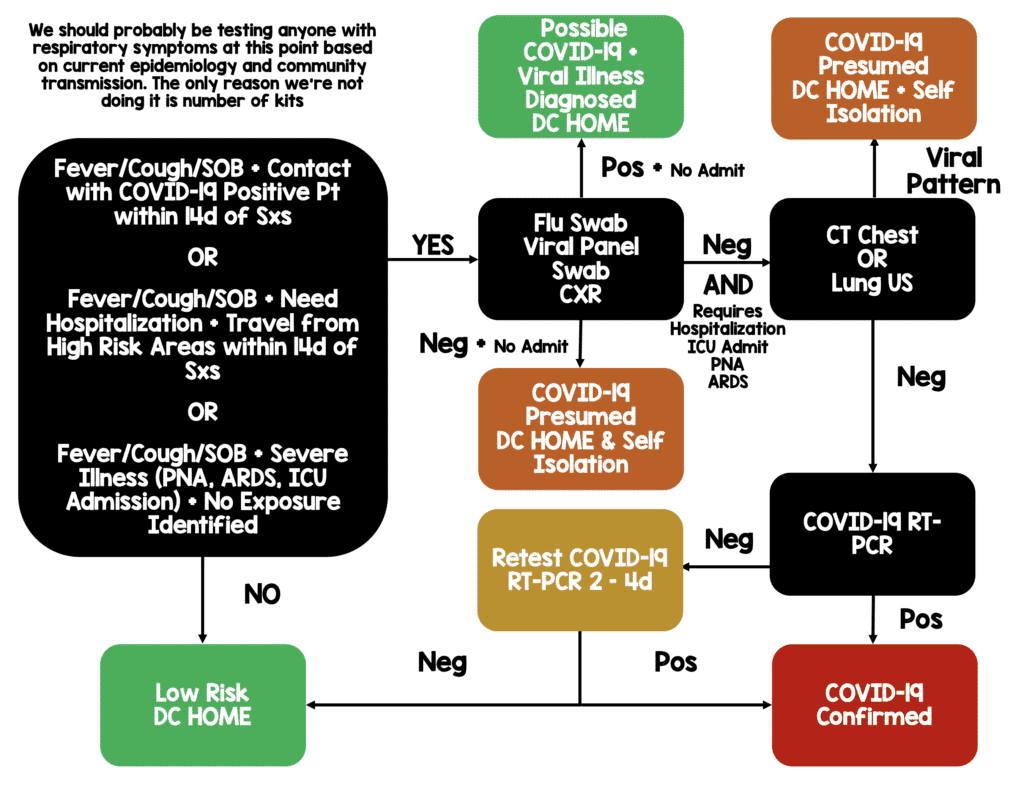
Potential Workflow for COVID-19 Patients (March 20th, 2020):
- Thank you to Anand Swaminathan, MD (Twitter: @EMSwami) and Josh Farkas, MD (Twitter: @PulmCrit) for their input on this
- None of our current diagnostic tools are great, and until we have a RT-PCR assay that has a rapid turnaround time (currently 1 – 7d) and availability (we simply don’t have enough tests to test everyone) this seems to be what makes the most sense
- CT chest and Lung US are faster than RT-PCR in terms of turnaround time, therefore in the sickest patients (i.e. requiring hospitalization, ICU admit, PNA, ARDS) this seems to be the best 1st step (i.e. This is not for all patients)
- One obvious drawback of using the CT scanner is this will be the potential to contaminate the CT scanner
- Patients with negative flu swab, viral panel swabs, CXR and mild disease (i.e. none of the sickest patients from above) can most likely be diagnosed with presumed COVID-19 as they won’t really require any specific in-hospital treatment and be discharged home with specific self isolation instructions (i.e. we already do this for influenza)
- Patients with positive flu swab, viral panel swabs, and mild disease can most likely be diagnosed with a viral infection, but due to the rate of co-infection, COVID-19 is possible
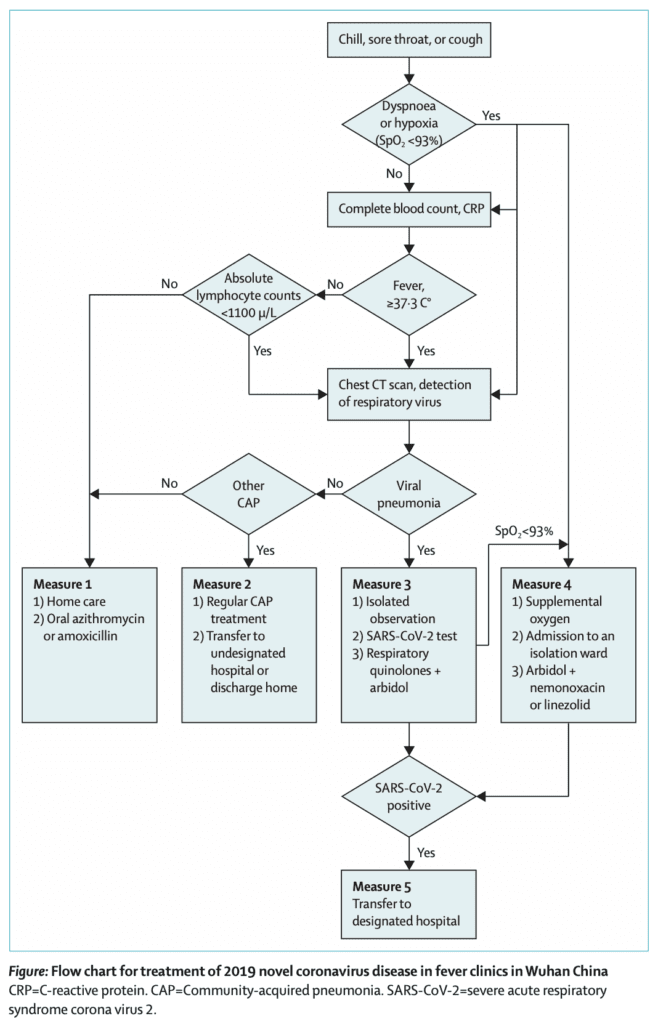
- One effective strategy that has been used during the COVID-19 epidemic in China is the use of fever clinics. An extrapolation of this might be tents outside the hospital. Attached is the workflow that is being used. [24] Interestingly, absolute lymphocyte count and CT scan is part of their algorithm.
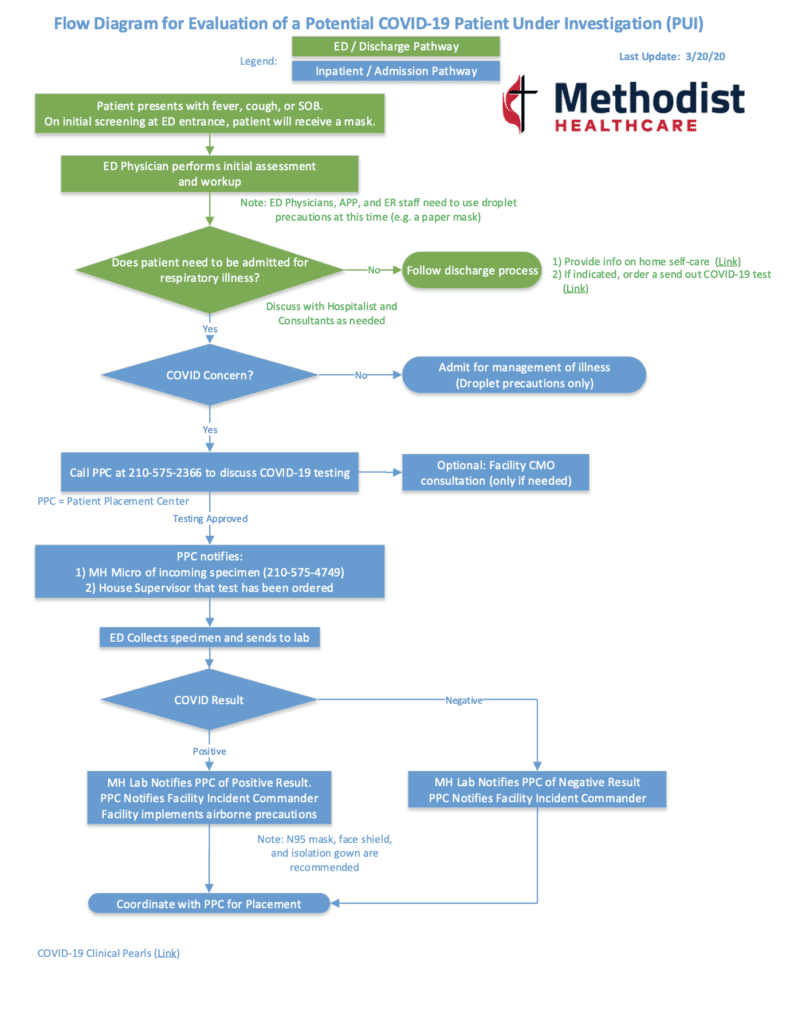
Flow Diagram for Evaluation of a Potential COVID-19 Patient Under Investigation (PUI) at my Home Institution (Last Updated Mar 20th, 2020)
viral coinfection: the struggle is real. we should be testing for all viruses *simultaneously*… (that is, if we were living in a country with a functional healthcare system) https://t.co/V5sRwpldpX pic.twitter.com/fV73zbTJvW
— 𝙟𝙤𝙨𝙝 𝙛𝙖𝙧𝙠𝙖𝙨 💊 (@PulmCrit) March 18, 2020
I have been working on a #COVID #COVID19 decision tool that is based on #BSTImaging and NHS guidelines but incorporates #POCUS lung ultrasound. Resources will vary and different places will have to determine their own guidelines but I would love some general feedback. #FOAMed pic.twitter.com/ABBVCrUzvi
— Jacques Loubser (@JPLoubser) March 19, 2020
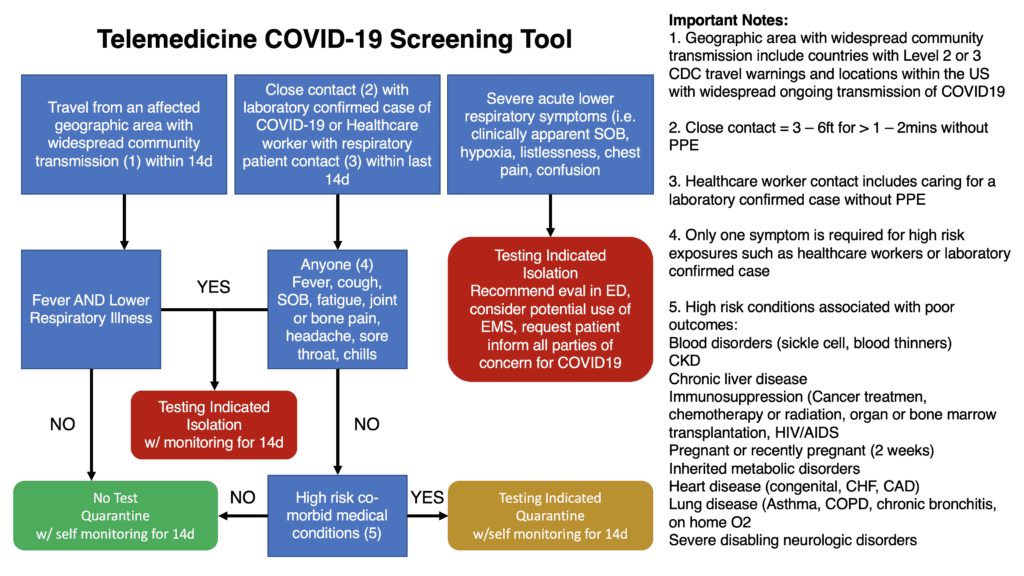
Telemedicine COVID19 Screening Algorithm Used at my Home Institution (Last Updated March 17th, 2020)
- Summary of CMS’s March 9th COVID-19 EMTALA Guidance for Alternative Locations: CMS’s March 9th COVID-19 EMTALA Guidance
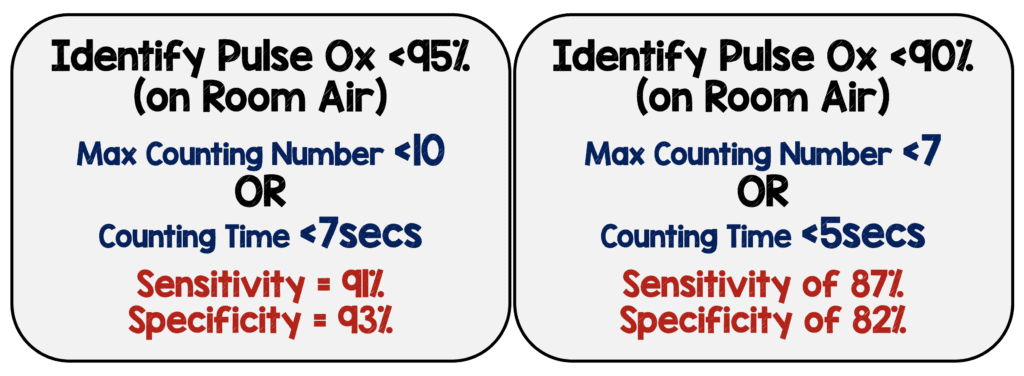
Roth Index to Assess O2 saturation (on room air)[1]
- What They Did:
- Prospective, controlled-cohort study
- Patients admitted to internal medicine service or cardiac ICU in Israel
- Included: Pulse oximetry on room air requiring 2L to 6L NC O2 to maintain O2 saturation >92%
- Excluded: Hypoxia requiring advanced noninvasive or invasive oxygenation
- Control group: 103 Healthy volunteers
- Roth Score:
- Have patient take a deep breath in and count out loud from 1 to 30 in their native language, in a single breath, as rapidly as possible
- Primary result:
- Duration of time elapsed between counting from 1 to 30 in 1 breath OR until patient took another breath
- Highest number reached in 1 breath (measured with stopwatch in seconds from 1 to highest number reached)
- Languages evaluated: Hebrew, Arabic, Russian, French, and English
- Results:
- Most common admission diagnoses: CHF (25%), PNA (17%), and ACS (15%)
- Strong positive correlation between pulse oximetry and both:
- Maximal count achieved in 1 breath: r = 0.67; P < 0.001
- Counting time: r = 0.59; p <0.001
- All healthy volunteers counted to at least 15 in 1 breath and 97 (94%) counted to at least 20
- Constructed ROC curve with room air saturation as primary variable:
- Identifying O2 sat <95% (on room air)
- ROC curve for max count number: 0.828
- ROC curve for counting time: 0.764
- Identifying O2 sat <90% (on room air)
- ROC curve for max count number: 0.843
- ROC curve for counting time: 0.812
- Identifying O2 sat <95% (on room air)
- Limitations:
- Test is patient effort-dependent
- Hypoxia is only one element of dyspnea
- Tool has not been validated
- This tool is not intended to replace more advanced testing in diagnosing respiratory distress or etiology of dyspnea
- Bottom Line: In a setting of increased demand with resource scarcity telemedicine is an option, as it is cost effective and resource-sparing and although the Roth Score still needs to be validated, it may be one option to determine patients oxygen saturation
References:
- Chorin E et al. Assessment of Respiratory Distress by the Roth Score. Clin Cardiol 2016. PMID: 27701750
For More Thoughts on This Topic Checkout:
- REBEL EM: COVID-19 – The Novel Coronavirus 2019
- St. Emlyn’s: COVID 19 Preparations in Virchester
- The Bottom Line: Pandemic Triage
- EM Cases: COVID-19 Part 2 – ED Surge Capacity Strategies in the COVID-19 Pandemic
- ACEM: Australasian College for Emergency Medicine Clinical Guidelines for the Management of COVID-19
- DFTB: Time for Telehealth
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Mizuho Morrison, DO (Twitter: mizuhomorrison)




