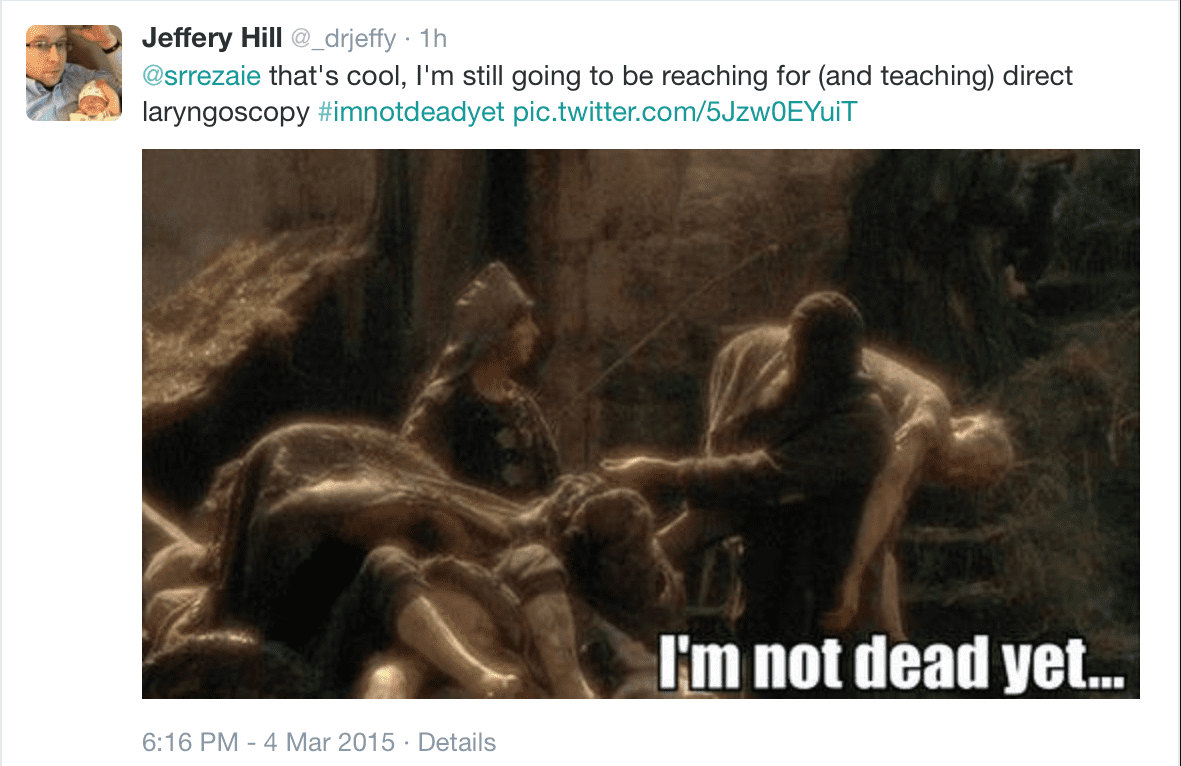
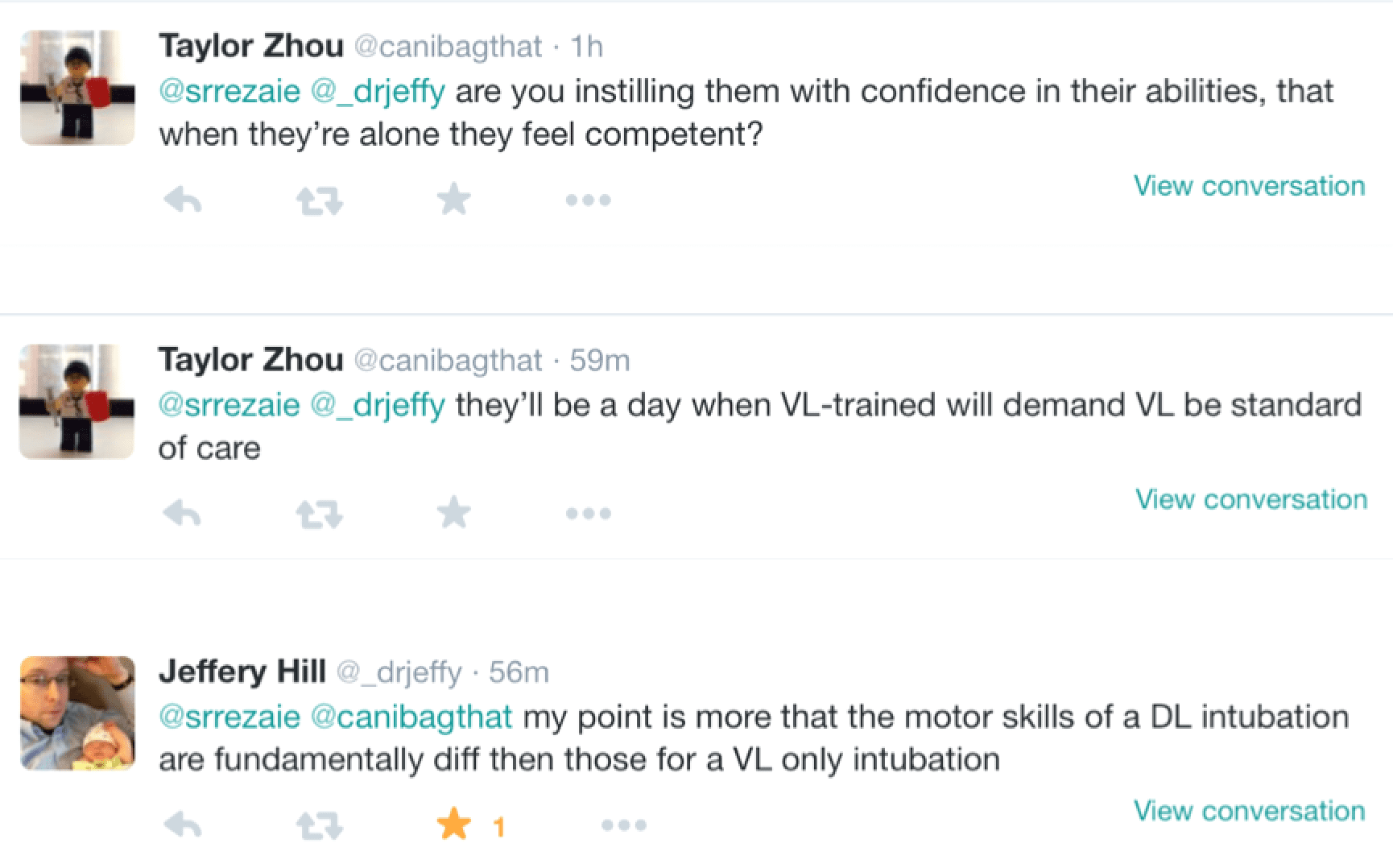
 According to a 2012 meta-analysis difficult and failed intubations in the operating room occur 1.8 – 5.8% and 0.13 – 0.30% of the time respectively. Emergent intubation, outside of this environment (i.e emergency department, ICU, and medical ward) is typically associated with a much higher risk of difficulty and complications due to many patients rapidly deteriorating. Recently, I had a discussion on twitter with Jeffrey Hill (@_drjeffy) and Taylor Zhou (@canibagthat) about what is the best way to teach trainees to intubate: Video Laryngoscopy (VL) or Direct Laryngoscopy (DL) for Trainees?
According to a 2012 meta-analysis difficult and failed intubations in the operating room occur 1.8 – 5.8% and 0.13 – 0.30% of the time respectively. Emergent intubation, outside of this environment (i.e emergency department, ICU, and medical ward) is typically associated with a much higher risk of difficulty and complications due to many patients rapidly deteriorating. Recently, I had a discussion on twitter with Jeffrey Hill (@_drjeffy) and Taylor Zhou (@canibagthat) about what is the best way to teach trainees to intubate: Video Laryngoscopy (VL) or Direct Laryngoscopy (DL) for Trainees?
How common is difficult airway and complications of intubation outside the OR?

In the ICU (136 Intubations) [1]
- 13.2% of all intubations required ≥3 attempts
- 6.6% of expert/faculty intubations required ≥3 attempts
- 10.3% of all intubations required > 10 minutes
- Overall risk of complications in 39% of intubations
- Severe Hypoxemia (19.1%)
- Severe Hypotension (9.6%)
- Esophageal Intubation (7.4%)
- Overall ICU and hospital mortality 15.4% and 29.4% respectively (p = 0.46 and 0.25 respectively)
Conclusion: Over 1/3 of intubations done in the ICU had complications associated with them in this study

On the Wards (150 Intubations) [2]
- 76% 1st pass intubation rate overall
- Complication rates: 27% emergent intubation vs 22% elective intubation
- Biggest complications:
- >2 attempts in 9%
- Esophageal Intubation in 9%
- No survival difference between emergent intubation (59%) vs elective intubation (50%) [p = 0.46]
- No survival difference between patients with complications (48%) vs no complications (54%) [p = 0.63]
Conclusion: Emergent intubation on the inpatient wards had a nearly 1/3 complication rate in this study

In the Emergency Department (280 Intubations) [3]
- 83% 1st pass intubation rate overall
- 1st pass intubation rate 81% for VL vs 83% for DL (p = 0.59)
- Intubation failure rate 14% for VL vs 8% for DL (p = 0.12)
- Median time to successful intubation 42 seconds for VL vs 30 seconds for DL (p <0.01)

Does video laryngoscopy increase success rate of emergent tracheal intubation vs direct laryngoscopy in untrained medical personnel? [4]
- Overall success rate GlideScope technique (93%) vs Direct laryngoscopy technique (51%) [P < 0.01]
- Time for intubation: 89 +/- 35 s for direct laryngoscopy vs 63 +/- 30 s for GlideScope technique (P < 0.01)
Conclusion: In untrained medical personal, VL had higher success rate of intubation and quicker time to intubation vs DL
How important is successful 1st pass intubation in care of patients? [5]
- First attempt success = 14.2% complication rate
- Two attempts = 47.2% complication rate
- Three attempts = 63.6% complication rate
- Four or more attempts = 70.6% complication rate
- Most common complication was oxygen desaturation
Clinical Take Home Point: As the number of attempts at intubation increases, so does the incidence of complications
Thoughts on Twitter
Results from Voting
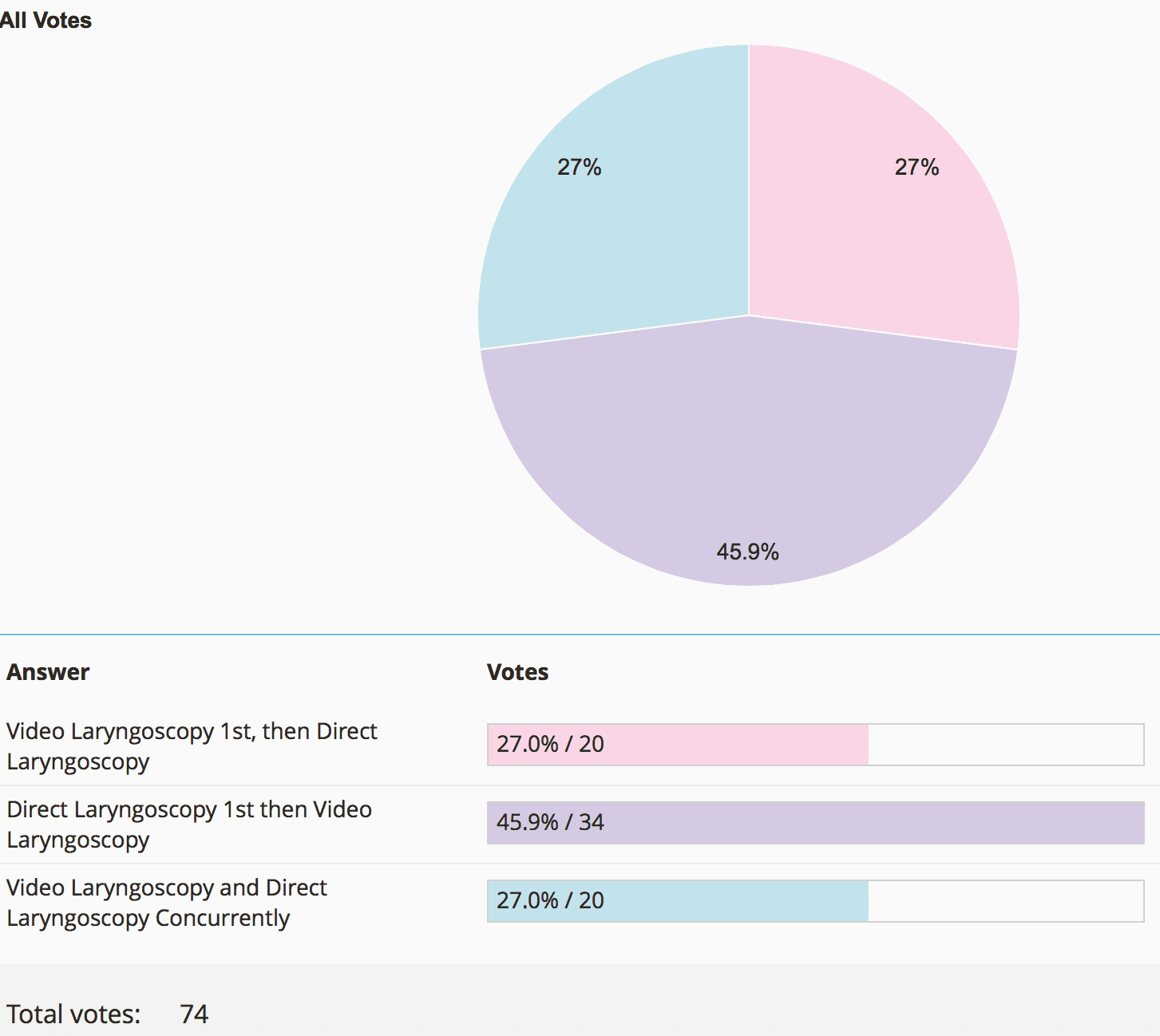
How Should Trainees Be Trained to Intubate?
Should Video Laryngoscopy Be the 1st Attempt Best Practice For Intubation?
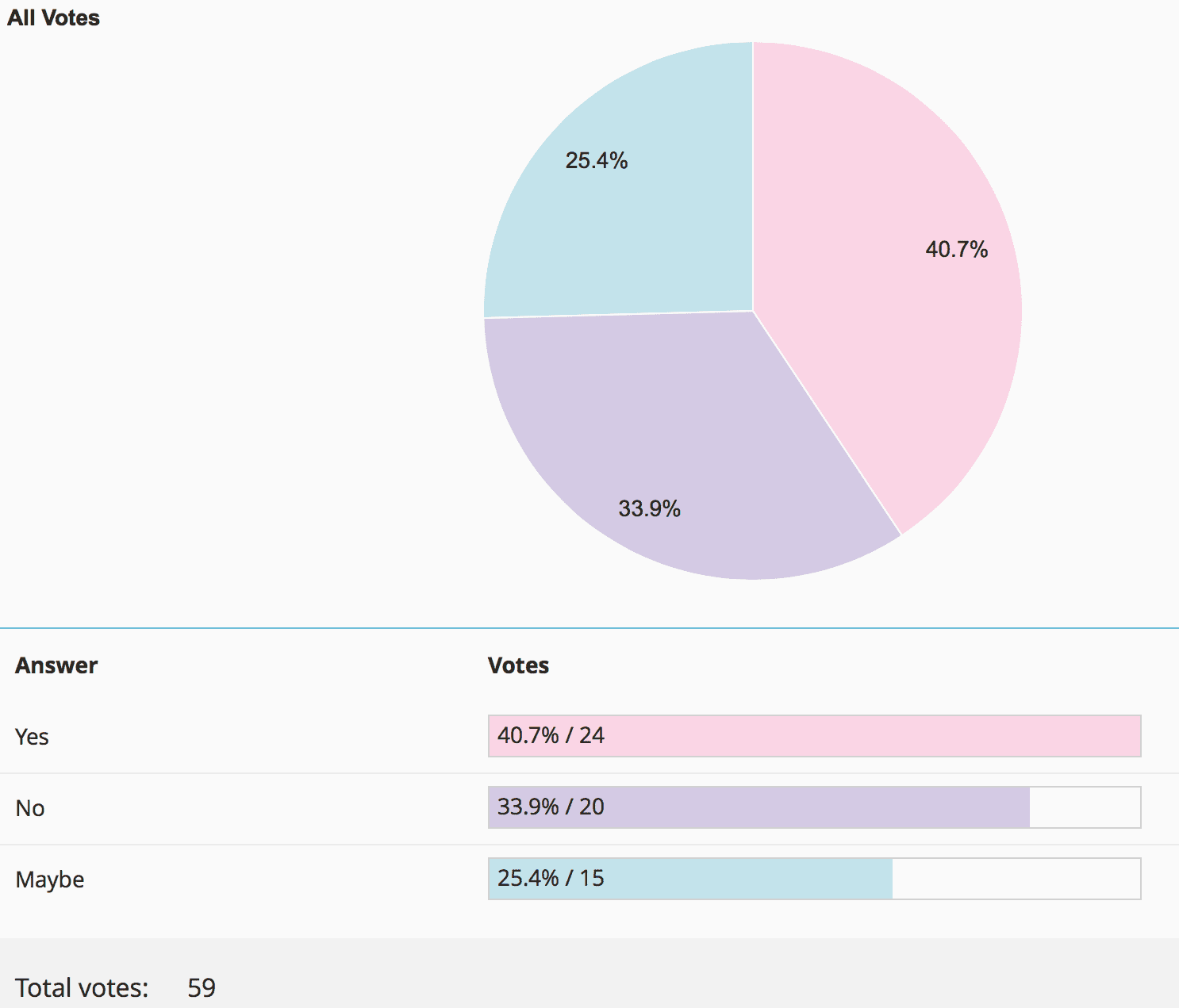
Results from Voting: Its a draw!!! What this tells us is that it doesn’t matter what your plan A is for intubation, but you should also be good at a plan B and plan C so that you can work in any environment!!!
 References:
References:
- Griesdale DE et al. Complications of Endotracheal Intubation in the Critically Ill. Intensive Care Med 2008. PMID: 18604519
- Benedetto WJ et al. Urgent Tracheal Intubation in General Hospital Units: An Observational Study. J Clin Anesth 2007. PMID: 17321922
- Platts-Mills TF et al. A Comparison of GlideScope video Laryngoscopy versus direct Laryngoscopy Intubation in the Emergency Department. Acad Emerg Med 2009. PMID: 19664096
- Nouruzi-Sedeh P et al. Laryngoscopy via Macintosh Blade Versus GlideScope: Success Rate and Time for Endotracheal Intubation in Untrained Medical Personnel. Anesthesiology 2009. PMID: 19104167
- Sakles JC et al. The Importance of first Pass Success When Performing Orotracheal Intubation in the Emergency Department. Acad Emerg Med 2013. PMID: 23574475
For Other Peoples Opinions Check Out:
- Scott Weingart at EMCrit: Podcast 94 – Has Video Laryngoscopy Killed the Direct Laryngoscope?
- Ken Milne at The SGEM: SGEM#75: Video Killed Direct Laryngoscopy?
- Jo Deverill at LITFL: DL Terminated
- PulmCCM: Should video-guided intubation be standard training in critical care? (And should anesthesiologists teach it?)
- Minh Le Cong at PHARM: PHARM PODCAST 104 – VL vs DL with Levitan and Strayer




