How is Submassive PE Defined in the Literature:
- Acute PE without hypotension (SBP <90mmHg) but with any of the following:
- RV dysfunction on POCUS
- RV dilation (RV:LV Diameter >0.9 on POCUS)
- Elevated BNP (>500pg/mL)
- Elevated Troponin I (>0.4ng/mL)
- Elevated Troponin T (>0.1ng/mL)
- New ECG Changes (Complete or Incomplete RBBB, Anteroseptal ST-Segment Elevation/Depression, or Anterolateral T-Wave Inversion)
What do Different Organizations Say About the Use of Systemic Thrombolytics for Submassive PE:
- American College of Chest Physicians (ACCP): NO (Grade IB)
- American Heart Association (AHA): Select Patients (Grade IIB)
- European Heart Association (EHA): Select Patients
- American College of Emergency Physicians (ACEP): Insufficient Evidence to Make a Recommendation
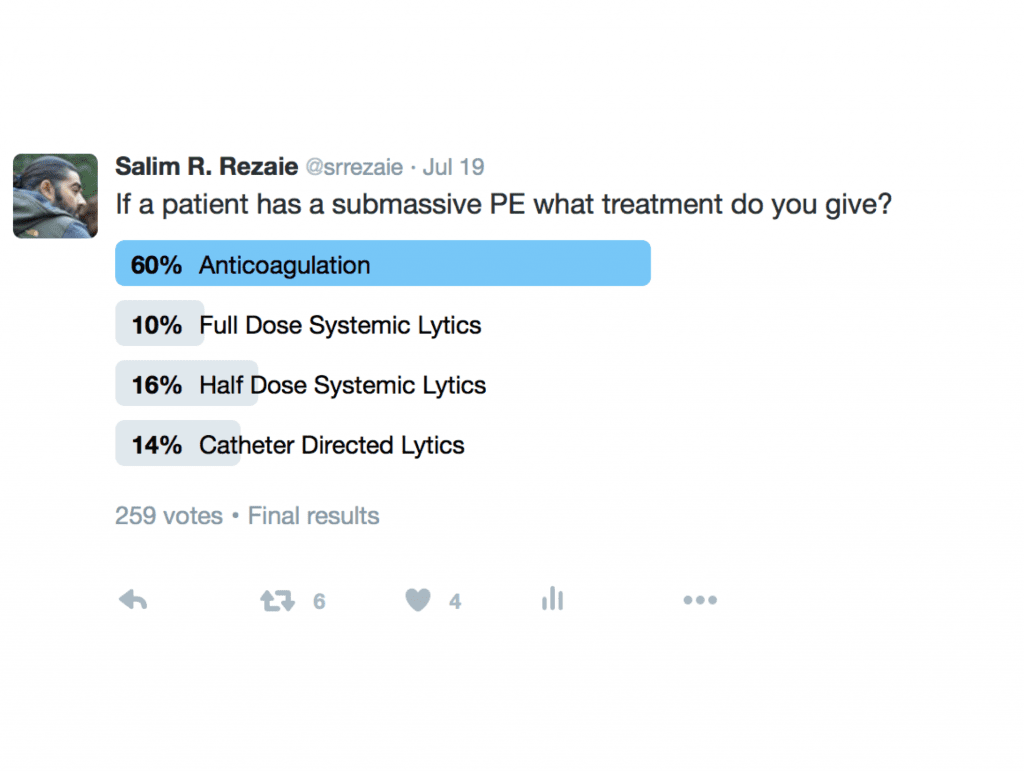
What Does the Twitterverse Say About the Treatment of Submassive PE:
Full Dose Systemic Thrombolytics:
- PEITHO Trial (Largest RCT to Date) – 2014
- 1005 patients with submassive PE and evidence of RV strain
- Weight based tenecteplase + standard dose parental anticoagulation vs anticoagulation alone
- Primary Outcome: Death or hemodynamic decompensation
- Reduced but primarily driven by reduction in hemodynamic decompensation
- Increased Major Bleeding and ICH (Primarily in patients ≥75 years of age)
- TOPCOAT (Treatment of Submassive PE with Tenecteplace or Placebo: Cardiopulmonary Outcomes at 3 months) – 2014
- 83 patients with submassive PE
- Full Dose Tenecteplase with standard dose heparin vs Placebo with standard dose heparin
- Primary Endpoint: Death, Need for intubation or Surgical thrombectomy at 5d and 6 weeks
- Improved quality of life, RV function, exercise capacity, and perception of physical wellness at 6 weeks in thrombolytic group but with increased ICH
- Major Bleeding
- 0% in both groups
- ICH
- Tenecteplase 1/40 (2.5%)
- Anticoagulation Alone = 0%
- Major Bleeding
- MAPPET-3 (Management Strategies and Prognosis of PE Trial-3) – 2002
- 256 patients double-blinded, randomized clinical trial
- Alteplase 100mg + standard dose heparin vs placebo + standard dose heparin
- Primary Endpoint In-Hospital Death or Clinical Deterioration (Need for vasopressors, surgical embolectomy, cardiopulmonary resuscitation, intubation or secondary thrombolysis)
- No difference in mortality
- Patients treated with heparin alone had more cases of deterioration
- No difference in bleeding between groups
- Chaterjee S et al 2014 Meta-Analysis
- All-cause mortality lower with thrombolysis vs anticoagulation alone in patients with moderate and high-risk PE (2.17 vs 3.89%) NNT = 59
- Major bleeding and ICH higher in thrombolysis vs anticoagulation alone in patients with moderate and high-risk PE (9.24% vs 3.42%) NNH = 18 and (1.46 vs 0.19%) NNH = 78
- Submassive PE mortality lower with thrombolysis vs anticoagulation alone (1.39% vs 2.92%) NNT = 65
- Submassive PE major bleeding higher with thrombolysis vs anticoagulation alone (7.74% vs 2.25%) NNH = 18
- Clinical Bottom Line: These three studies showed mixed results in terms of mortality benefits. However, there was also a consistent decrease in hemodynamic decompensation and quality of life with full dose thrombolytic therapy. Conversely, there was a uniform increased risk of major bleeding in patients > 65 years of age
Half Dose Systemic Thrombolytics:
- MOPETT (Moderate PE Treated with Thrombolysis) Trial
- Single Center, Unblinded Randomized trial of 121 patients
- ½ dose tPA + modified dose anticoagulation vs placebo + standard anticoagulation
- Primary Outcome: Pulm HTN defined by TTE at 28months
- Thrombolytic Group 16%
- Anticoagulation Alone 57%
- NNT = 2
- No bleeding in either group
- No functional outcomes assessed
- Bottom Line: Improved pulmonary pressures, no functional outcomes assessed, but no increase in major bleeding or ICH
- Levine et al – 1990
- 58 patients
- Alteplase 0.6mg/kg (Max: 50mg) IV vs Heparine Alone
- Primary Outcome: Clot Burden on V/Q Scan at 7d and 28d
- Decreased with thrombolysis vs Anticoagulation alone
- No Major Bleeding in either group
- Mortality not assessed
- Bottom Line: Decreased Clot Burden on V/Q scan with no increase in major bleeding
- Clinical Bottom Line: Improves Surrogate outcomes (i.e. Mortality not assessed) but no increased major bleeding
Full Dose vs Half Dose:
- Prospective, RCT 118 pts HD Instability or massive pulmonary artery obstruction
- 24hr & 14days
- 50mg/2h tPa vs 100mg/2h tPa
- Any Improvement in Pulmonary Artery Obstruction
- No difference in primary outcomes at 24hr or 14days
- Any Bleeding Complications
- More bleeding complications and major bleeding with full dose thrombolytics
- Systematic Review and Meta-Analysis of 5 RCTs (444 patients) – 3 compared full dose vs half dose
- Low Dose 0.6mg/kg with Max of 50mg vs Full Dose 100mg IV
- More Major Bleeding Events with Full Dose (OR 0.33)
- No Statistical Difference in Recurrent PE or Mortality
- Low Dose 0.6mg/kg with Max of 50mg vs Full Dose 100mg IV
- Clinical Bottom Line: Similar efficacy in death and recurrent PE in patients with massive and submassive PE, but a tendency toward less bleeding with half dose thrombolytics
Full Dose vs Half Dose vs Anticoagulation Alone
- Systematic Review and Meta-Analysis of 5 RCTs (444 patients)
- Two Studies Compared Low Dose (0.6mg/kg Max 50mg/2hr or 10mg Bolus + ≤40mg/2hr vs heparin drip alone
- No Difference in Major Bleeding Events, Recurrent PE or All-Cause Mortality
- Improved Clot Burden 7 days:
- Levine et al 12% vs 34.4% on V/Q Scan
- Sharifi et al 16% vs 57% on Echo
Catheter Directed +/- Ultrasound
- SEATTLE-2 (2015)
- Prospective, Single-arm, Multi-center trial of Ekosonic Endovasucular System and Activase for Treatment of Acute Pulmonary Embolism Trial
- US-Facilitated, catheter directed, low-dose thrombolysis
- Primary Outcome was RV/LV ratio at 48h
- Secondary Outcome was Pulmonary Pressure
- 31 patients with massive PE and 119 with submassive PE
- Treatment decreased RV dilatation, reduced Pulmonary HTN, decreased clot burden, and minimized risk of ICH in patients with PE, but increased length of hospital stay (8.8d +/- 5)
- Zero cases of ICH but one groin hematoma that suffered some transient hypotension
- PERFECT Trial (2015)
- Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis (PERFECT)
- Prospective Multicenter Single-Arm Study
- 101 Patients
- Clinical Success = Stabilization of HD, Improvement in Pulm HTN, Improved RV Strain & Survival to Hospital DC
- Safety Outcomes = Major procedure related Complications & Major Bleeding Events
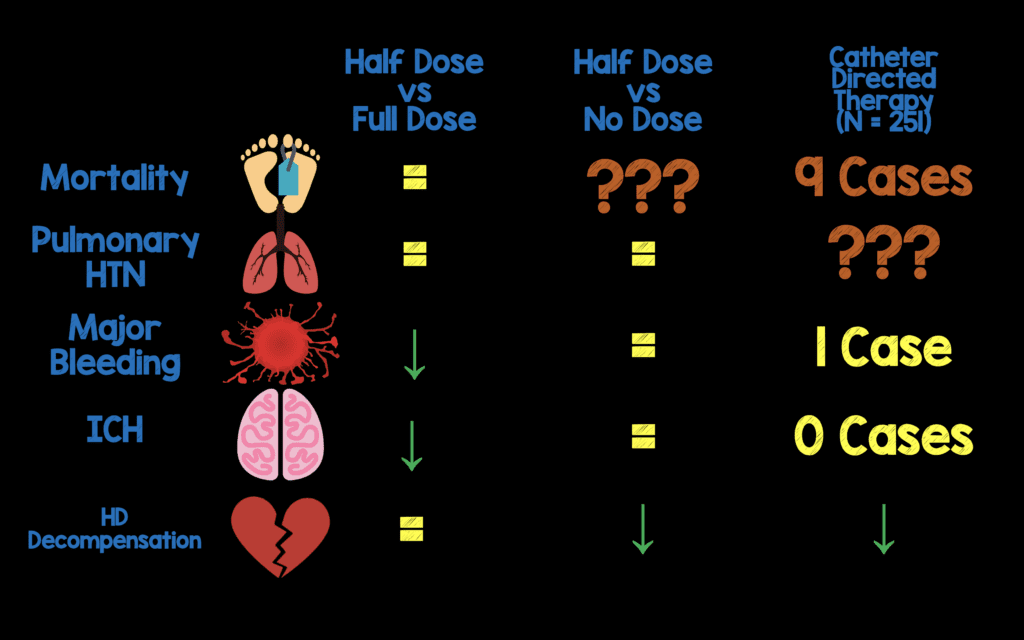
Clinical BOTTOM LINE:
- There is not a clear cut answer based on the available evidence, but with a shared decision making strategy, consideration of patient age (≥65 years vs <65 years) and functional status considerations, some generalizations can be made:
- Full dose systemic thrombolysis is effective BUT has a high bleeding complication rate. Acceptable /Unacceptable bleeding rates should be discussed on a case by case basis with patients using a shared decision making strategy
- Low dose systemic thrombolysis has less bleeding with equal efficacy compared to full dose systemic thrombolysis, however more data is needed on mortality outcomes. This may be a good strategy in patients over the age of 65 years who have increased risk of major bleeding and ICH.
- The evidence for CDT is very scant and not compared to systemic thrombolysis, but it does appear to be more expensive and cause longer length of ICU stay compared to systemic thrombolysis. This may be another option to consider in patients with increased risk of bleeding (i.e. Patients 65 years and older) while balancing cost and use of resources
- CDT and low dose systemic thrombolysis improve symptoms, hemodynamics, RV/LV size, other echo parameters and PA pressures, but long-term clinical correlates are still lacking
For More on This Topic Checkout:
- Anand Swaminathan at St. Emlyn’s Blog: The Argument for Systemic Thrombolytics in Submassive Pulmonary Embolism
- Rory Spiegel at EM Nerd (EMCrit): The Case of the Shadowy Spector
- Josh Farkas at PulmCrit (EMCrit): Submassive PE 2017 – Getting ’em Off the Cliff
References:
- Sharifi M et al. Systemic Full Dose, Half Dose, And Catheter Directed Thrombolysis for Pulmonary Embolism. When to Use and How to Choose? Curr Treat Options Cardio Med 2016; 18: 31. PMID: 26923384
- Long B and Koyfman A. Current Controversies in Thrombolytic Use in Acute Pulmonary Embolism 2016. JEM 51(1): 37 – 44. PMID: 27071316
- Kuo WT, Banerjee A, Kim PS, et al. Pulmonary embolism response to fragmentation, embolectomy, and catheter thrombolysis (PERFECT): initial results from a prospec- tive multicenter registry. Chest. 2015;148:667–73. PMID: 25856269
- Piazza G et al. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism: The SEATTLE II Study. JACC 2015; 8(10_ 1382 – 92. PMID: 26315743
- Chatterjee S et al. Thrombolysis for Pulmonary Embolism and Risk of All-Cause Mortality, Major Bleeding, and Intracranial Hemorrhage: A Meta-Analysis. JAMA 2014; 311 (23): 2414 – 2421. PMID: 24938564
- Meyer G et al. Fibrinolysis for Patients with Intermediate-Risk Pulonary Embolism. NEJM 2014; 370(15): 1402 – 1411. PMID: 24716681
- Konstantinides S et al. Heparin Plus Alteplase Compared with Heparin Alone in Patients with Submassive Pulmonary Embolism. NEJM 2002; 347 (15): 1143 – 1150. PMID: 12374874
- Stein PD et al. Intracerebral Hemorrhage with Thrombolytic Therapy for Acute Pulmonary Embolism. Am J Med 2012; 125(1): 50 – 6. PMID: 22115025
- Kline JA et al. Treatment of Submassive Pulmonary Embolism with Tenecteplase or Placebo: Cardiopulmonary Outcomes at 3 Months: Multicenter Double-Blind, Placebo-Controlled Randomized Trial. J Thromb Haemost 2014; 12(4): 459 – 68. PMID: 24484241
- Sharifi M et al. Moderate Pulmonary Embolism Treated with Thrombolysis (from the “MOPETT” Trial). Am J Cardiol 2013; 111(2): 273 – 7. PMID: 23102885
- Wang C et al. Efficacy and Safety of Low Dose Recombinant Tissue-Type Plasminogen Activator for the Treatment of acute Pulmonary Thromboembolism: A Randomized, Multicenter, Controlled Trial. CHEST 2010; 137(2): 654 – 62. PMID: 19741062
- Zhang Z et al. Lower Dosage of Recombinant Tissue-Type Plasminogen Activator (rt-PA) in the Treatment of Acute Pulmonary Embolism: A Systematic Review and Meta-Analysis. Thrombosis Research 2014; 133(3): 357 – 63. PMID: 24412030
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
Cite this article as: Salim Rezaie, "Treatment of Submassive Pulmonary Embolism (PE): Full Dose, Half Dose, or No Dose?", REBEL EM blog, November 3, 2016. Available at: https://rebelem.com/treatment-of-submassive-pe-full-dose-half-dose-or-no-dose/.



