 For the most part, the biggest concern with administering tPA is the bleeding complications, specifically intracranial hemorrhage. But there is another side effect that is being reported more frequently. I, myself, saw two cases in one week. This side effect is tPA-associated angioedema.
For the most part, the biggest concern with administering tPA is the bleeding complications, specifically intracranial hemorrhage. But there is another side effect that is being reported more frequently. I, myself, saw two cases in one week. This side effect is tPA-associated angioedema.
Case: A 70-year-old female with a past medical history of hypertension and diabetes presents to your department 45 minutes after onset of left facial droop, slurred speech and left-sided hemiparesis. The initial head CT is negative for acute hemorrhage. You diagnose your patient with an acute ischemic stroke. There are no contraindications, so you decide to treat the patient with tPA (we will leave this debate for another time).
Pathophysiology
tPA gets its antifibrinolytic properties by activating plasminogen to form plasmin. There are a series of chemical reaction that make most practicing physicians’ heads spin. The byproducts of these reactions include increased bradykinin, activation of the complement cascade (C3a and C5a), and increased release of histamine. These three factors lead to an anaphylactoid reaction or angioedema in some patients.
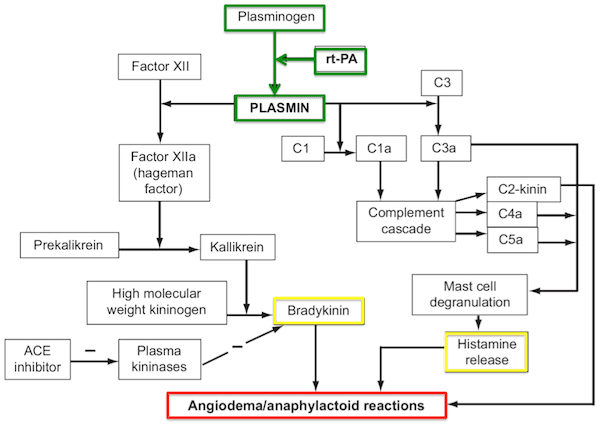
Image from [1]
Epidemiology
There are several case reports of angioedema follow tPA administration. Three separate studies have reported the incidence of tPA-related angioedema. In 2003, Hill et al published a series of 176 patients that received tPA. Nine of these patients (5.1%) developed tPA [2]. Engelter et al reported that 1.7% of 120 patients developed angioedema [3]. The largest study included 1,135 tPA patients, but only 1.3% developed angioedema [4]. It can be said that this is a rare event, but similar to hemorrhage, which has been reported from 2-9%. The use of ACE inhibitors increases the risk of developing angioedema due to baseline increase in bradykinin levels. Angiotensin receptor blockers have not shown the same risk, but care should be taken.
Presentation
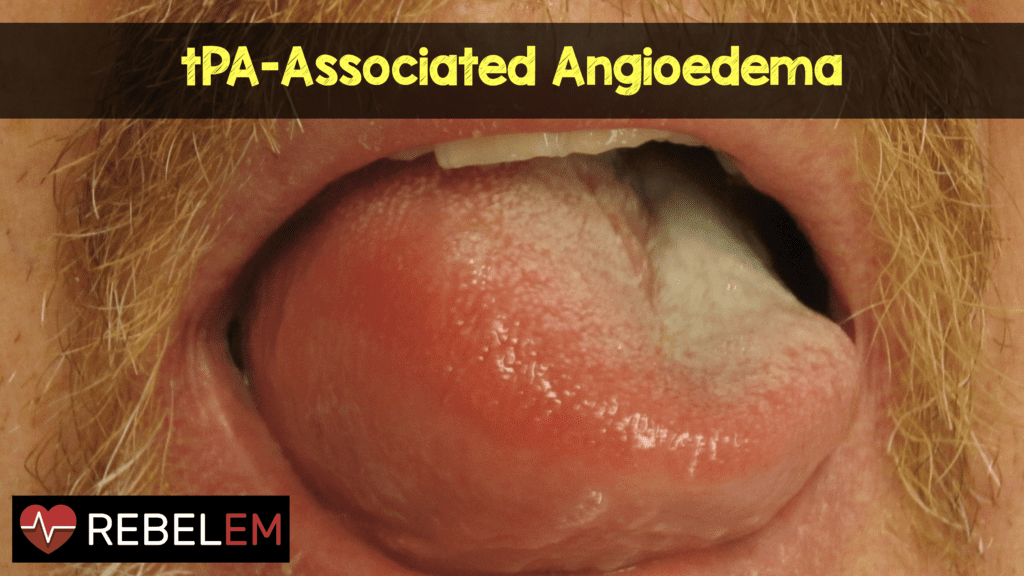
The onset of angioedema can be variable, but once the infusion of tPA has completed, the risk angioedema greatly decreases. The majority of tPA associated angioedema are orolingual versions. Symptoms may be asymmetric and often appear on the side contralateral to the ischemic hemisphere. One proposed theory is that infarction of the contralateral insular cortex can lead to autonomic dysfunction and vasomotor changes in the hemiparetic side. The onset of tongue swelling in these patients should also include in the differential diagnosis lingual hematoma. Look for signs of ecchymosis on the tongue.

Image from Wikipedia
Treatment
Most of these cases of angioedema have a mild, self-limited, and benign course. While tPA is infusing, the patient should be monitored every fifteen minutes. With the development of symptoms, the infusion of tPA should stop, if not already complete. Rapid airway assessment should be done to determine the need for intubation. Some clinical factors can help guide the decision to intubate.
- The rapidity of edema progression (i.e. ≤ 30 minutes) [5].
- The anatomic site. The more anterior the edema is (lips, anterior tongue), the less likely the need for intubation [6].
If you need to intubate, have the most experienced provider do it, and have many adjuncts and rescue methods ready. An awake intubation may be the best option. Fortunately, the need for a surgical airway is rare. Imagine cutting the neck of someone who just received tPA!!!
Even though most cases are self-limited, medical treatment is often undertaken. The mainstay of medical therapy is the use of corticosteroids and antihistamines. Some authors have reported the use of epinephrine safely [5], but there is a theoretical risk of inducing intracranial hemorrhage.
Clinical Bottom Line
tPA-associated angioedema is a rare (1.3 – 5.1% incidence), but known complication. One must remain vigilant and be on guard for this. While treating one potentially life-threatening disease, you may induce another. Be ready to manage the airway. You may never see this…but then again, you may see two in a single week.
References:
- Maertins M et al. Angioedema After Administration of tPA for Ischemic Stroke: Case Report. Air Med J 2011. PMID: 21930083
- Hill MD et al. Hemi-Orolingual Angioedema and ACE Inhibition After Alteplase Treatment of Stroke. Neurology 2003. PMID: 12743244
- Engelter ST et al. Life-Threatening Orolingual Angioedema During Thrombolysis in Acute Ischemic Stroke. J Neurol 2005. PMID: 16184341
- Hill MD et al. Thrombolysis for Acute Ischemic Stroke: Results of the Canadian Alteplase for Stroke Effectiveness Study. CMAJ 2005. PMID: 15883405
- Fugate JE et al. Angioedema After tPA: What Neurointensivists Should Know. Neurocrit Care 2012. PMID: 22311232
- Grant NN et al. Clinical Experience with Angiotensin-Converting Enzyme Inhibitor-Induced Angioedema. Otolaryngologists Head Neck Surg 2007. PMID: 18036423



