 In October 2016, I was exposed to the vast world of Free Open Access Medical Education and MedTwitter. I was astounded and inspired by the different educators who were trying to make learning easier. The Knowledge Translation (KT) gap was being vastly shortened by some very smart people who took to social media to educate the rest of the world. Although there were knowledge bombs in all areas of medicine, I was particularly drawn to the ones most relevant to emergency medicine and critical care.
In October 2016, I was exposed to the vast world of Free Open Access Medical Education and MedTwitter. I was astounded and inspired by the different educators who were trying to make learning easier. The Knowledge Translation (KT) gap was being vastly shortened by some very smart people who took to social media to educate the rest of the world. Although there were knowledge bombs in all areas of medicine, I was particularly drawn to the ones most relevant to emergency medicine and critical care.
Each day in 2017, I used Twitter to share a few pearls with the world as my contribution to #FOAMed. I included the hashtag #TodayILearned (Today I Learned) so I could keep track of them to use for future projects. Here are just a few of those pearls:
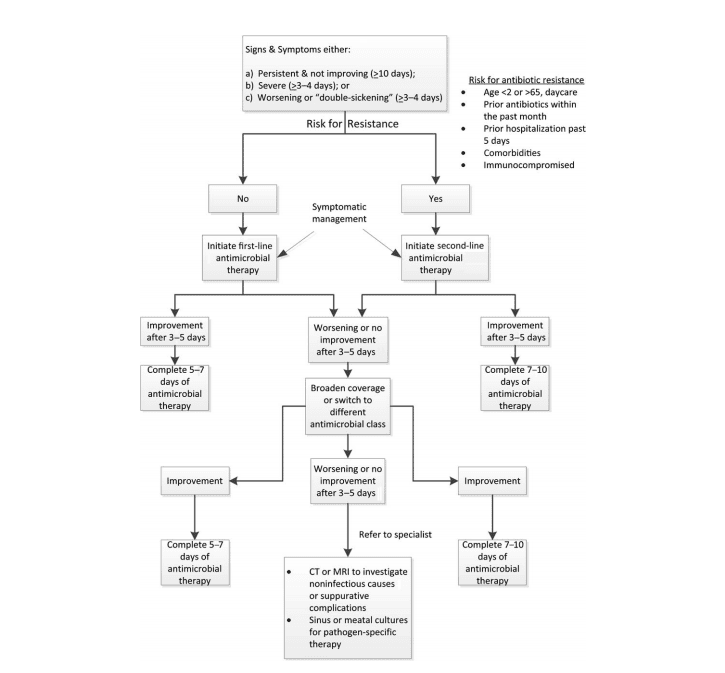
Antibiotics for Acute Rhinosinusitis Protocol [1]
Covered by CoreEM: Sinusitis
- Give antibiotics if any of these are present:
- Persistent symptoms and not improving ≥10 days
- Severe symptoms ≥3-4 days
- Worsening or “double sickening” (initial improvement of symptoms followed by worsening ≥5 days after start of illness)
- If patient has risk for antibiotic resistance, use second-line therapy; if not, use first-line therapy.
- Resistance risk factors: Age<2 or >65, antibiotic use in the last month, hospitalization in the last week, comorbidities, immunocompromised
- First-line:
- Adults: Amoxicillin-Clavulanate 875mg-125mg TID
- Children: Amoxicillin-Clavulanate 45mg/kg of Amoxicillin component in two divided doses (Max 4g)
- Second-line:
- Adult: High dose Amoxicillin-Clavulanate (2000mg-125mg)
- Children: Amoxicillin-Clavulanate 90mg/kg of Amoxicillin component in two divided doses (Max 4g) OR Cefpodoxime 10mg/kg in two divided doses (max 400mg/day)
- 5-7 days of treatment if first-line therapy; 7-10 days of treatment if second-line therapy.
- If worsening or not improving after 3 days of treatment, switch antibiotic class.
- Respiratory fluoroquinolone (Levofloxacin)
- Adults: 750mg daily
- Children: 20mg/kg in two divided doses, max 500mg/day
- Doxycycline
- Adults only: 100mg BID
- Respiratory fluoroquinolone (Levofloxacin)
- If improving, treat for 5-7 days if first-line therapy and 7-10 days if second-line therapy.
- If worsening or not improving, consider CT/MRI or culture and sensitivity for pathogen-specific therapy.
CPR-Induced Consciousness (CPRIC) [2][3][4]
Covered by EMUpdates: CPR Induced Consciousness: 30 Second Video
CPRIC is a real thing! Patients will move, track people or objects, and even answer questions during resuscitations. This is occurring more frequently as we implement evidence-based resuscitation protocols emphasizing early and high-quality CPR. Unfortunately, resuscitation can be a traumatic experience for our patients so have a sedation plan for CPRIC. Here is a sample prehospital protocol from Nebraska EMS [5]:
- Ketamine
- IV: 0.5-1.0mg/kg
IM: 2-3mg/kg - Re-dose after 5-10 minutes if needed, or start infusion: 2-7mcg/kg/min.
***After some research, these seem like very low doses to me and may have been done so purposefully as this was for a prehospital protocol. Doses up to 90mcg/kg/min have been suggested for maintenance of anesthesia [6]. More data are needed to determine the appropriate in-hospital dosing.
- IV: 0.5-1.0mg/kg
- Consider Midazolam coadministration
- IV: 1mg
IM: 2mg
- IV: 1mg
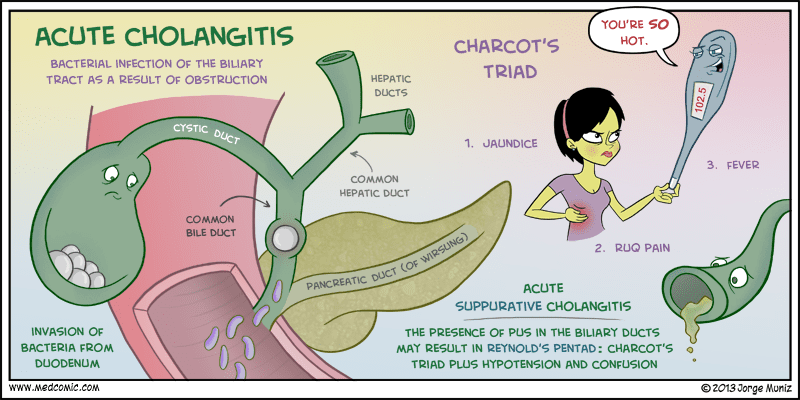
Cholangitis Eponyms [7][8]
Charcot’s Triad = RUQ Pain + Jaundice + Fever
Reynold’s Pentad* = Charcot’s Triad + Altered Mental Status + Hypotension
Fun Fact: Jean-Martin Charcot, the “Napoleon of neuroses,” is associated with at least 15 medical eponyms.
*seen in less than 10% of patients with cholangitis
Acute Heart Failure Management [9][10]
You have diagnosed your patient with acute heart failure in the emergency department. What next?
- ABCs, oxygen (only if SaO2 is <93%), continuous cardiac and vital signs monitoring, patient positioning, sodium and fluid restriction
- Labs to consider: CBC, electrolytes, kidney and liver function tests, BNP, troponin, blood gas
- Other tests: EKG, CXR, POCUS
- Search for cause of the AHF
- Consider the following interventions:
- Loop diuretic therapy
- 1-2.5 times patient’s total daily oral dose, divided into two equal doses per day
- Diuretic naïve: start with 20-40mg Furosemide
- Nitroglycerin
- Sublingual: 0.4mg tab, one per minute until relief or IV infusion is started
- IV infusion: 0.5-0.7mcg/kg/min, titrated to BP up to 200mcg/min*
- Noninvasive Positive Pressure Ventilation
- Urine output monitoring
- VTE prophylaxis if patient is not already on anticoagulation
- Opioids are still controversial but may provide anxiolysis and decrease work of breathing
- Loop diuretic therapy
- If hypotensive, consider an inotrope (Dobutamine or Milrinone) or vasopressor (Norepinephrine)
*Editor’s note: Nitrate dosing can be done many different ways. The key is to reach high doses quickly to drop both preload and afterload. This can be done by starting around 100 mcg/min and rapidly titrating up or, by starting with a loading dose (400-500 mcg/min) and then dropping down to 150-200 mcg/min when the patient begins to improve. See this discussion for more perspective on the topic.
What’s next?
Just as I have done above, I would like to continue sharing the learning points that I gathered over the course of the year. I am working on codifying the pearls into the form of a daily calendar that I would like to share with everyone as a free resource. Medical students and residents interested in emergency medicine and/or critical care can learn or review a new pearl each day to use on shift that day. I would love to hear your thoughts on this, so feel free to comment below or contact me directly at smuramed@gmail.com or on Twitter @smuramed.
Guest Post By:
References:
- Chow AW et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clinical Infectious Disease 2012. PMID: 22438350.
- Parnia S et al. AWARE-AWAreness during Resuscitation-a prospective study. Resuscitation 2014. PMID: 25301715.
- Olaussen A et al. Consciousness induced during cardiopulmonary resuscitation: An observational study. Resuscitation 2017. PMID: 28161214.
- Strayer R. CPR Induced Consciousness. EMUpdates 2018. http://emupdates.com/cpric/.
- Rice DT et al. CPR induced consciousness: It’s time for sedation protocols for this growing population. Resuscitation 2016. PMID: 26956842.
- Miller RD, Miller’s Anesthesia, 7th ed, Philadelphia PA: Churchill Livingstone, 2010.
- Wada K et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. J Hepatobiliary Pancreatic Surgery 2007. PMID: 17252297.
- Reynolds BM et al. Acute obstructive cholangitis; a distinct clinical syndrome. Annals of Surgery 1959. PMID: 13670595.
- Tintinalli J et al. Tintinalli’s Emergency Medicine: a Comprehensive Study Guide, 8th Ed. Chapter 53.
- http://www.uptodate.com/contents/treatment-of-acute-decompensated-heart-failure-components-of-therapy
Post Peer Reviewed By: Anand Swaminathan, MD (@EMSwami) and Salim R. Rezaie, MD (@srrezaie)



